
Cognitive behavioural therapy (CBT) for patients with chronic lung disease and psychological comorbidities undergoing pulmonary rehabilitation
Introduction
Chronic lung conditions such as chronic obstructive pulmonary disease (COPD), asthma, interstitial lung disease (ILD) and bronchiectasis are common conditions with high rates of mortality and morbidity (1). Although pathophysiological changes secondary to each respiratory condition has an impact on the well-being of patients, psychological comorbidities also have an important negative influence on these patients. Psychological comorbidities are highly prevalent among patients with chronic lung disease (2-5) and are correlated with worsened quality of life (3,5,6), increased exacerbation rates (7), poor adherence to treatment (8), and in COPD their presence has been correlated with increased mortality (9-11). The presence of anxiety and depression is common with incidence varying among each chronic lung disease (3,4,12-14), disease severity (12,14-17) and poor quality of life (3,6,14,15,18,19).
Cognitive behavioural therapy (CBT) is a type of psychotherapy used in the management of a range of psychiatric disorders. It is based on an information-processing model in which emotional symptoms are thought to be driven by negatively-biased evaluations of the world, the future, or the self (including bodily sensations) (20). CBT has demonstrated promising results in reducing anxiety and depression symptoms in patients with COPD (21-30), asthma (31) and bronchiectasis (32). CBT is likely to be as effective when delivered face-to-face or by telephone (33-35), with telephone delivery potentially improving adherence to CBT (27). Pulmonary rehabilitation is an important standard of care for patients with symptomatic chronic lung diseases (36,37) and after completion of a comprehensive pulmonary rehabilitation program symptoms of anxiety and depression have been shown to improve (38-42). Conversely, anxiety and depression have been associated with non-completion of pulmonary rehabilitation programs (43,44), reduced adherence (45) and fear of exercise (46). In patients with COPD, the addition of face-to-face CBT to pulmonary rehabilitation improved 6-minute walk test (6MWT), and symptoms of depression, anxiety and stress (28,47).
CBT and pulmonary rehabilitation are both forms of therapy with strong evidence for treating anxiety and depression in patients with chronic lung disease, and although distinct, they are theoretically synergistic therapies. CBT could, therefore, be incorporated into pulmonary rehabilitation programs to potentiate the beneficial effects of both therapies (26,48,49). The study aimed to assess the impact and feasibility of CBT given through a mixed face-to-face and telephone format as a treatment for patients with chronic lung disease and coexisting anxiety and/or depression symptoms who were undergoing pulmonary rehabilitation.
Methods
Design
This was a prospective, randomized controlled trial in patients with chronic lung diseases undertaking pulmonary rehabilitation. The Intervention group received CBT given in 6 sessions, with the first 2 sessions being delivered face-to-face and the last 4 sessions delivered by telephone. The face-to-face sessions occurred during the 8 weeks of pulmonary rehabilitation. The telephone sessions occurred after the pulmonary rehabilitation sessions. Telephone-based CBT has shown to be an effective treatment approach for treating depression and anxiety in patients with COPD (27,50). The use of mixed approach with initial face-to-face sessions then telephone-based therapy, was intended to have the established face-to-face therapy to improve therapeutic alliance and minimise the possibility of reduced effectiveness of a solely telephone-based therapy and then continue with telephone-based therapy to maximise adherence. The Control group received usual treatment and 4 brief sham telephone calls at approximately similar time points as the Intervention group. Due to the nature of the therapy, the therapists, investigators and participants were not blinded to the allocated group.
Data were collected at the end of the pulmonary rehabilitation program, 3 months and 12 months following completion of the program for each participant. The study was approved by the ethics committee of The University of Queensland and The Prince Charles Hospital in Queensland, Australia, and is registered with the ANZCTR (ACTRN12614000915651). Written informed consent was obtained from all participants before enrolling in the study.
Participants
This study included patients above 18 years of age with chronic lung diseases including COPD, asthma, ILD, or bronchiectasis diagnosed by a thoracic physician and undertaking pulmonary rehabilitation at The Prince Charles Hospital, Brisbane, Australia. COPD diagnosis was based on Global Initiative in Obstructive Lung Disease (GOLD) criteria. Asthma diagnosis was determined by the presence of variable symptoms and bronchodilator reversibility present on spirometry. ILD was diagnosed based on CT scan, respiratory lung function and/or by histopathology findings. Bronchiectasis was diagnosed by high-resolution CT chest scan. The presence of clinical or subclinical anxiety or depression in COPD patients based on previous studies was defined by GDS of ≥4/15 (51) and GAI score ≥3/20 (52), respectively.
Patients were excluded if they had a known psychotic disorder, were undergoing psychological therapy, unable to give written informed consent or were participating in another research project. Patient with cognitive impairment, defined by impairment determined by Mini Mental State Examination (MMSE) score of <23/30 (53) were excluded.
Randomization and intervention
Screening forms were sent before rehabilitation program commencement. Forms review and recruitment were done during the first 2 weeks of a comprehensive 8-week pulmonary rehabilitation program with exercise and education. Patients enrolled in the study were randomised in a 1:1 basis to the Intervention group (CBT) or Control group (usual care) using pre-printed sealed assignments generated by a computer-generated software package. No minimum block size was used in the randomization.
Both groups attended together a comprehensive 8-week pulmonary rehabilitation program. Each week of the program consisted of 2 sessions of 2 hours duration, involving 1 hour of supervised exercise (walking and/or stationary cycling and upper and lower limb strengthening) and 1 hour of multidisciplinary education. All participants received a hard copy of the Lung Foundation Australia’s Better Living with COPD patient information booklet, which contained a chapter on stress, anxiety and depression (54).
The Intervention group received CBT conducted by postgraduate psychology interns under the supervision of a qualified psychologist. The CBT intervention was based on a manualised approach that was developed by the Psychology Department of The Prince Charles Hospital. One session was videotaped and later reviewed by a specialist in clinical psychology to ensure adherence to the manual and quality of the intervention. The intervention comprised 2 face-to-face sessions of 1 hour each, just before or after the pulmonary rehabilitation classes. In addition, 4 telephone sessions of 45 minutes each were undertaken for counselling, within the first 2 months after the face-to-face sessions. The CBT intervention was tailored to the patient’s individual needs.
CBT sessions aimed to build skills in self-management, behavioural activation, identifying and challenging unhelpful thinking, improving relaxation and breathing skills, and promoting effecting coping through training in problem-solving. Components of the intervention included: Cognitive interventions; Psychoeducation about the interaction between anxiety and physical symptoms (the anxiety-dyspnoea cycle); Challenging and modifying unhelpful cognitions; Problem-solving training to address barriers to effective coping; Behavioural interventions: Relaxation and distraction techniques; Breathing techniques (in conjunction with Pulmonary Rehabilitation nurses); Reinforcement of activity scheduling; Planning and “pacing” skills; Development of a personalized “good coping plan” (55-57).
To minimise the difference caused by social interaction gained by CBT in the Intervention group, participants in the Control group received telephone contacts with the study personnel at similar time points as the Intervention group. The telephone call to the Control group participants was of a shorter duration (5 to 10 minutes) than the CBT calls to the Intervention group and consisted of a brief assessment of respiratory symptoms.
Outcomes and follow-up
The primary outcome of interest was the efficacy of CBT as an effective treatment of depression and anxiety among patients with chronic lung disease attending a pulmonary rehabilitation program. GDS and GAI were used to assess depression and anxiety symptoms respectively. Secondary measures included the St George’s Respiratory Questionnaire (SGRQ) to assess quality of life (58); 6-minute walk distance at baseline and the end of pulmonary rehabilitation to assess exercise capacity, and pulmonary rehabilitation attendance and participation.
Demographic and clinical data, body mass index (BMI), Montreal cognitive assessment (MoCA) score (to identify frontal dementia) (59) and MMSE score (to identify cognitive impairment) (53) were assessed in all patients. In COPD patients, modified Medical Research Council dyspnoea scale (mMRC) and the body-mass index, airflow obstruction, dyspnoea, and exercise capacity index were assessed, to calculate the BODE score (60).
Statistical analysis
Descriptive statistics were used for exploratory analysis. To determine correlation coefficients between continuous variables, Pearson’s correlation was used. To determine differences between the Intervention and Control groups, t-tests and χ2 tests were undertaken for continuous and categorical outcomes, respectively. Intention to treat analysis was performed. A P value (two-tailed) <0.05 was considered statistically significant.
For data collected at multiple points in time, a longitudinal analysis was undertaken, by comparing the change in outcomes over time in the Intervention and Control group using repeated measures tests. For these paired measures, a Wilcoxon signed-rank test was used to determine any significant difference over time. Statistical analyses were run using Stata 17 (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC).
A power calculation estimated that a sample size of 50 Intervention and 50 Control participants would have 80% power at alpha (significance) level 0.05 to detect a 3-fold increase in significant improvement of anxiety or depression scores, based on the assumption of improvement of 10% of the Control group and 33% of the Intervention group.
Results
Baseline characteristics of participants
Of the 193 patients screened, 126 patients (65.3%) were eligible to be enrolled in the study, based on a GDS ≥4 and/or GAI ≥3. Twenty-two (11.4%) patients declined enrolment in the study, 9 (4.7%) did not attend pulmonary rehabilitation for further assessment, and another 19 (9.8%) were excluded. Results are outlined in the CONSORT diagram (Figure 1).
Sixty-five patients were enrolled in the study and randomized (24 patients to Intervention and 41 patients to Control). Ten of 24 patients (41.7%) in the Intervention group failed to complete the intervention, consisting of 6 patients (25%) who withdrew before the commencement of CBT and 4 patients (16.7%) who started but did not complete CBT therapy (with an average of one CBT session attended). 3 of these patients also did not continue pulmonary rehabilitation. 4 of 41 patients (9.75%) in the Control group did not complete the study, consisting of 1 patient (2.4%) who withdrew, 2 patients (4.9%) who failed to attend 6 or more pulmonary rehabilitation sessions, and 1 patient (2.4%) who died during the pulmonary rehabilitation study period (Figure 1).
Demographic details of the patients enrolled are described in Table 1. The mean age of the group studied was 68.8 years and 60% were females. The majority of patients had COPD (75.4%), and the remainder had asthma (10.8%), bronchiectasis (9.2%) and ILD (4.6%). A wide range of lung function impairment was observed. Fourteen (21.5%) had only symptoms of depression and 12 (18.4%) had symptoms of anxiety while 39 (60.0%) had both symptoms of depression and anxiety.

Full table
Twenty-two percent of patients had a known mood disorder and 22% were on antidepressants, with selective serotonin reuptake inhibitors (SSRI) being the most common antidepressant. Twenty percent of the population enrolled had a low MoCA score. There were no statistically significant differences in baseline parameters between the Intervention and Control groups (Table 1).
There was a weak but statistically significant correlation between failure to attend pulmonary rehabilitation (<6 sessions) and GDS (r=0.18, P=0.01) but not for GAI (r=0.12, P=0.09).
The final number of participants (n=65) was approximately two-thirds of the total number originally planned (n=100), due to the slower than anticipated recruitment rate, limited resources available and the high dropout rate from the Intervention (CBT) group. A decision was therefore made to finish the study early at a total of 65 randomised participants.
Outcomes at end of pulmonary rehabilitation
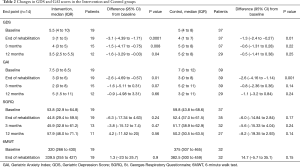
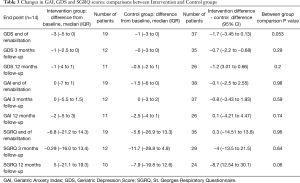
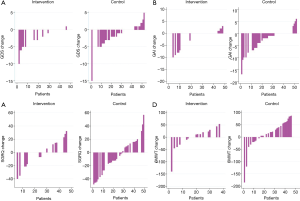
At the end of pulmonary rehabilitation, there was a statistically significant decrease in GDS (improvement in depression symptoms) compared to baseline, in both the Intervention and Control groups. The mean decrease in GDS was 3.1 in the Intervention group (P=0.0001), while in the Control group, the mean decrease was 1.3 (P=0.01). For GAI, there was a mean decrease of 2.6 in both the Intervention and Control groups (Table 2). There was no statistically significant difference in the changes in GDS or GAI scores between the Intervention and Control groups (Table 3). The waterfall plot demonstrates that almost all patients that completed the CBT program improved their GDS, while the same was not seen in the Control group. GAI showed the same improvement pattern in both Intervention and Control groups (Figure 2). SGRQ and 6-minute walk test did not demonstrate a significant improvement in either the Intervention or Control groups (Table 2).
Full table
Full table
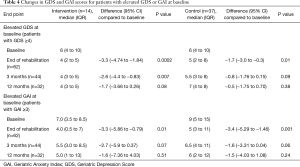
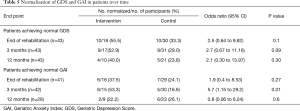
For those patients with symptoms of depression at baseline (GDS score ≥4/15), there was a significant improvement in GDS by the end of rehabilitation, within each of the Intervention and Control groups (P=0.0002) and (P=0.01), respectively (Table 4), which was not statistically different between these groups (P=0.16). By the end of pulmonary rehabilitation, 55.5% in the Intervention group and 33% in the Control group achieved no demonstrable symptoms of depression based on a normal GDS, although the difference was not significant between groups (P=0.1) (Table 5). Patients with symptoms of anxiety at baseline (GAI score ≥3/20) there was an improvement in GAI in both the Intervention and Control groups, which was not statistically different between these groups (P=0.32). CBT did not lead to significant increase of GAI normalization (37.5% vs. 24%; P=0.27) (Table 5).
Full table
Full table
The Intervention group showed a significant increase in the number of pulmonary rehabilitation sessions attended, with the mean number of attended sessions of 14.0 (±1.7) in the Intervention group and in 12.4 (±2.6) in the Control group, out of the maximum number of 16 sessions (P=0.03).
Outcomes at 3 and 12 months follow-up
There was a sustained improvement in depression symptoms measured by GDS at 3 (P=0.008) and 12 months (P=0.04) in the Intervention group, that was not demonstrated in the Control group (Table 2). These changes at 3 and 12 months were not significantly different between the Intervention and Control groups (Table 3). For anxiety symptoms measured by GAI, there was no difference from baseline or between groups at the 3- and 12-month follow-up for the Intervention and Control groups (Tables 2,3). Similar to anxiety symptoms, health-related quality of life showed no significant difference from baseline in both groups, and there was no significant difference between the groups at 3 and 12 months (Table 3).
Outcomes in patients with significant symptoms of GDS or GAI at baseline
For patients with an elevated GDS score at baseline, there was a sustained improvement in GDS scores at 3 months (P=0.007) but not at 12 months (P=0.08) follow-up in the Intervention group, which was not demonstrated in the Control group at 3 and 12 months (Table 4); and there was no significant difference between groups at both 3 months (P=0.3) and 12 months (P=0.48). CBT did not lead to a significant improvement in patients achieving a normal GDS, with 53% of patients in the Intervention group achieving a normal GDS at 3 months and 40% achieving a normal GDS at 12 months follow-up; while the Control group 39% and 24% of patients achieved a normal GDS at 3 and 12 months, respectively (Table 5).
For patients with an elevated GAI score at baseline, there was no significant improvement in GAI in the Intervention and Control groups at 3 and 12 months follow-up (Table 4). There was also no significant difference between the groups at 3 months (P=0.13) and 12 months (P=0.84). At 3 months there was a significant increase in the rate of GAI normalization in the Intervention groups [53% vs. 17%; OR −1.63 (−3.31 to 0.04); P=0.01], which was not present at 12 months (22.2% vs. 26.1%; P=0.6) (Table 5).
Discussion
This study evaluated the effects of CBT as an addition to pulmonary rehabilitation for patients with chronic lung conditions of moderate to severe disease severity and symptoms of depression and anxiety. As demonstrated in previous studies, there was a significant reduction in symptoms of anxiety and depression in all patients by the end of pulmonary rehabilitation. However, unlike those studies, our study did not show an improvement in health-related quality of life (as determined by SGRQ) (38-40). The study by Catalfo et al. (40), which evaluated patients with COPD with symptoms of anxiety and depression, employed a more intensive pulmonary rehabilitation program of 2 hours daily for 6 weeks, which was significantly more than the standard 2 hours twice a week in our pulmonary rehabilitation program. Their more intensive exercise protocol could have played a significant role in improving both quality of life and mood symptoms and highlights the link between physical capacity and quality of life. Our study showed that despite the lack of improvement in SGRQ, there was an improvement in depression and anxiety symptoms in both Intervention and Control group, which may suggest that these symptoms are more responsive to the effects of pulmonary rehabilitation.
As demonstrated in previous studies (26,28), our study showed a significant improvement in GDS by the end of rehabilitation for both the Intervention and Control groups. The Intervention group seemed to have a numerically larger reduction in mean GDS of 3.1 (almost 50% of baseline score) compared to the Control group (1.34), although this did not reach statistical significance. Interestingly, in almost all patients that undertook CBT, there was a reduction in GDS as shown in the waterfall plots, while in the Control group approximately two-thirds of the patients improved their GDS. After CBT, the level of reduction of depression scores in our study was similar to the study by Catalfo et al. (40) which had a more rehabilitation program sessions, which may indicate that CBT could augment the psychological benefits of pulmonary rehabilitation. A factor that could have contributed to the lack of significance observed between Intervention and Control groups by the end of rehabilitation was the overall improvement in each patient group. This improvement might have had a dampening effect, an issue that may have contributed to a reduced effect in another study that used 6 sessions of group based CBT given with a similar pulmonary rehabilitation program (28). Our study showed a sustained improvement in GDS at 3 and 12 months in the Intervention group, which was not significantly different from the Control group at both time intervals. The lack of a significant difference could be secondary to the reduced sample size analysed. It is possible that CBT could prolong pulmonary rehabilitation benefits in patients with symptoms of depression, a fact supported by the demonstration of sustained improvement of GDS between baseline and follow-up for the Intervention group but not for the Control group. When analysing only those with elevated GDS at baseline, there is also a sustained improvement at 3 months but unexpectedly not at 12 months, which may reflect smaller numbers of participants at 12 months follow up since the overall improvement was larger in those with high GDS. With regards to anxiety symptoms, by the end of pulmonary rehabilitation, the results were similar to GDS, and there was no significant sustained improvement at 3 and 12 months.
With regards to anxiety symptoms, the Intervention group failed to show significant improvement in GAI at 3 and 12 months follow-up, although there was a significant difference in reaching normal GAI at 3 months follow up. The reason for the lack of sustained improvement in GAI or the discrepancy between anxiety and depression was not clear, although similar results were demonstrated in a comparable study that used mindfulness and CBT added to pulmonary rehabilitation (49). Possible reasons for the heterogeneity of results could be due to different methods of anxiety symptoms assessment tools (28), durations of CBT, method of delivery of therapy or if CBT was aimed at panic symptoms or generalized anxiety. There have been heterogeneous results regarding therapy delivery, duration and improvement in anxiety and depression scores. A previous study by Hynninen et al. (22) showed sustained improvement in both depression and anxiety, although the study involved 7 sessions of 2 hours of group delivered CBT, which is significantly more than our protocol of 6 sessions of one hour duration of 2 face to face and 4 phone delivered sessions. On the other hand, a study by Farver-Vestergaard et al. (49) using mindfulness-based CBT provided 8 telephone sessions and 8 group sessions added to pulmonary rehabilitation and showed a reduction in depression symptoms but not anxiety. The study by Livermore et al. (25) which had a targeted protocol to panic-related anxiety symptoms given to post-pulmonary rehabilitation patients, showed a significant reduction in anxiety score up to 18 months post treatment, although there was no change in depression scores. This may imply that the panic-related anxiety symptoms are more significant is this group and that treatment targeted to these symptoms is more effective to improve anxiety scores.
Similar to previous studies, the presence of depression was associated with poor pulmonary rehabilitation attendance and completion (43,44,61-63). Non-attendance in pulmonary rehabilitation programs may reflect poor overall adherence to other forms of treatment, as depression has been associated with poor medication adherence (8). The cause is unclear, but lack of energy, motivation and poor perception of self-worth could all contribute to the lack of engagement with treatment in this population. This is unfortunate since due to the negative impact of depression and the positive effects of pulmonary rehabilitation for these patients, they are a group who could possibly benefit the most from engagement with treatment. As hoped, a targeted psychological therapy such as CBT for this at-risk population of poor adherence improved attendance at pulmonary rehabilitation in our study. However, this improved attendance did not translate to improved markers such as 6MWT or improved health-related quality of life.
Limitations
The main limitation in our study was slower than expected enrolment and high rates of withdrawal or failure to attend therapy, leading to a relatively small number of patients completing the Intervention group. In the Intervention group, 10 of 24 patients (42%) withdrew or did not attend pulmonary rehabilitation and CBT. Compared to another study that had only employed telephone-based CBT (27), this was a lower than expected completion rate. 17% of eligible patients declined to participate and most patients that declined therapy did this before receiving any CBT sessions, which could reflect negative preconceptions of what CBT entails and its effectiveness, or the stigma associated with psychological conditions. Our study did not randomize patients based on pharmacotherapy treatment which resulted in a non-significant difference in use between the Intervention and Control group and may have impacted the efficacy of CBT. However the impact of pharmacotherapy is likely minimal as there is some controversy regarding the benefit of pharmacotherapy as a monotherapy for depression or anxiety (64), and the likely minimal effects when added to CBT (65). The addition of CBT to pulmonary rehabilitation treatment could be seen by some patients as too time-consuming, as many patients who did not wish to attend CBT still attended pulmonary rehabilitation. It is possible that solely telephone-based therapy would have fewer withdrawals, as all patients that withdrew or failed to attend CBT did so during the face-to-face period of therapy; possibly making telephone-based a more attractive method of additional CBT therapy. A more individualised case-formulation approach to CBT may have also improved compliance and yielded better outcomes. Although there was a significant withdrawal rate that may have led a reduced effect size and which would make the analysis more susceptible to type 2 error, this was mitigated by the intention to treat analysis. The high withdrawal rate could also have led to a selection bias in the study. CBT seems to improve depression scores, but possibly only for patients already predisposed to engage in treatment. Independent of this matter, offering CBT to patients with depression during pulmonary rehabilitation could be beneficial, even if only for those willing to participate.
The study used a pragmatic approach of the same type of CBT intervention for all patients, independent of their underlying respiratory condition. This approach was chosen based on the hypothesis that an integrated pulmonary rehabilitation program with psychological treatment would benefit all types of patients. Although there was ultimately no difference in major outcomes between groups, it is possible that psychological comorbidities are different between respiratory conditions and consequently require different approaches, an aspect that was not assessed in our study.
Future considerations
Improvement in depression scores in the CBT group indicates the possible benefit in adding this treatment to patients with depressive symptoms attending pulmonary rehabilitation. Patients have the opportunity to learn strategies to manage depressive symptoms like cognitive restructuring and have opportunities to practice those techniques during safe and supervised exposures that cause dyspnoea. The pulmonary rehabilitation sessions can create positive experiences for patients and has the potential for desensitization of the symptoms of dyspnoea. How much teaching or how many sessions are sufficient to achieve proficiency in deploying these strategies is not clear; however, more sessions are likely to improve the likelihood of success (22,24,26). The target of therapy could play an essential role in the improvement of anxiety symptoms, as possibly the addition of therapy more directed at panic attack-related anxiety be more beneficial to those with anxiety symptoms (25). More intensive pulmonary rehabilitation programs are also likely to be more effective to improve mood symptoms (40), and in this context, the addition of CBT can lead to more opportunities to employ learnt strategies and possibly be a more effective treatment. Other options for rehabilitation such as home rehabilitation (66) are possibly as effective as usual pulmonary rehabilitation, making telephone-based CBT an ideal additional therapy for this form of rehabilitation. Another aspect that needs clarification is which method of delivery is the most efficient and cost-effective; as face-to-face may be more effective for anxiety symptoms (25), while telephone-based therapy may have better patient compliance (27).
Conclusions
This study did not find evidence that the addition of CBT in a mixed face-to-face and telephone approach to pulmonary rehabilitation was more effective in improving depression, anxiety and quality of life symptoms, compared to pulmonary rehabilitation alone. There was an associated sustained improvement in depression scores in the Intervention group at 3- and 12-month follow-up that was not significantly different from the Control group. The addition of CBT to pulmonary rehabilitation did not improve anxiety symptoms or quality of life compared to pulmonary rehabilitation alone. The use of CBT did improve pulmonary rehabilitation attendance, although this did not translate into an improvement in psychological or physical outcomes. A number of factors—slower than anticipated recruitment rate, high withdrawal rate from the Intervention (CBT) group and limited resources available—resulted in the premature cessation of this study at two-thirds of the planned sample size, which could have limited the effectiveness of the intervention in this study. Future studies should better determine the effect of targeted therapy against panic attack-related anxiety for those with anxiety symptoms and assess the difference in effectiveness and adherence to face-to-face therapy, telephone-based or group CBT in this population.
Acknowledgments
We would like to thank the patients and staff of The Prince Charles Hospital for their involvement in this study. The authors gratefully the valuable help of the psychology interns from The Prince Charles Hospital, who were instrumental in providing care to the patients during this study. This research was financially supported by the SEED Innovation Program, Queensland Health.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Human Research Ethics Committee of The Prince Charles Hospital (HREC/14/QPCH/57) and The University of Queensland (ID: 2014001654). All patients provided written informed consent.
References
- Mortality GBD. Causes of Death C. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117-71. [Crossref] [PubMed]
- Tay TR, Hew M. Comorbid "treatable traits" in difficult asthma: Current evidence and clinical evaluation. Allergy 2018;73:1369-82. [Crossref] [PubMed]
- Olveira C, Olveira G, Gaspar I, et al. Depression and anxiety symptoms in bronchiectasis: associations with health-related quality of life. Qual Life Res 2013;22:597-605. [Crossref] [PubMed]
- Carvajalino S, Reigada C, Johnson MJ, et al. Symptom prevalence of patients with fibrotic interstitial lung disease: a systematic literature review. BMC Pulm Med 2018;18:78. [Crossref] [PubMed]
- Pumar MI, Gray CR, Walsh JR, et al. Anxiety and depression-Important psychological comorbidities of COPD. J Thorac Dis 2014;6:1615-31. [PubMed]
- De Vries J, Kessels BL, Drent M. Quality of life of idiopathic pulmonary fibrosis patients. Eur Respir J 2001;17:954-61. [Crossref] [PubMed]
- Laurin C, Moullec G, Bacon SL, et al. Impact of anxiety and depression on chronic obstructive pulmonary disease exacerbation risk. Am J Respir Crit Care Med 2012;185:918-23. [Crossref] [PubMed]
- DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med 2000;160:2101-7. [Crossref] [PubMed]
- Abrams TE, Vaughan-Sarrazin M, Van der Weg MW. Acute exacerbations of chronic obstructive pulmonary disease and the effect of existing psychiatric comorbidity on subsequent mortality. Psychosomatics 2011;52:441-9. [Crossref] [PubMed]
- Ng TP, Niti M, Tan WC, et al. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med 2007;167:60-7. [Crossref] [PubMed]
- Divo M, Cote C, de Torres JP, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2012;186:155-61. [Crossref] [PubMed]
- Raherison C, Ouaalaya EH, Bernady A, et al. Comorbidities and COPD severity in a clinic-based cohort. BMC Pulm Med 2018;18:117. [Crossref] [PubMed]
- Scott KM, Von Korff M, Ormel J, et al. Mental disorders among adults with asthma: results from the World Mental Health Survey. Gen Hosp Psychiatry 2007;29:123-33. [Crossref] [PubMed]
- Gao YH, Guan WJ, Zhu YN, et al. Anxiety and depression in adult outpatients with bronchiectasis: Associations with disease severity and health-related quality of life. Clin Respir J 2018;12:1485-94. [Crossref] [PubMed]
- Omachi TA, Katz PP, Yelin EH, et al. Depression and health-related quality of life in chronic obstructive pulmonary disease. Am J Med 2009;122:778 e9-15.
- Schneider C, Jick SS, Bothner U, et al. COPD and the risk of depression. Chest 2010;137:341-7. [Crossref] [PubMed]
- de Carvalho-Pinto RM, Cukier A, Angelini L, et al. Clinical characteristics and possible phenotypes of an adult severe asthma population. Respir Med 2012;106:47-56. [Crossref] [PubMed]
- Yohannes AM, Willgoss TG, Baldwin RC, et al. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatry 2010;25:1209-21. [Crossref] [PubMed]
- Aydin IO, Ulusahin A. Depression, anxiety comorbidity, and disability in tuberculosis and chronic obstructive pulmonary disease patients: applicability of GHQ-12. Gen Hosp Psychiatry 2001;23:77-83. [Crossref] [PubMed]
- Greenberger D, Padesky CA. Mind Over Mood: A Cognitive Therapy Treatment. Manual for Clients. . New York, NY: Guilford Press.; 1995.
- Emery CF, Schein RL, Hauck ER, et al. Psychological and cognitive outcomes of a randomized trial of exercise among patients with chronic obstructive pulmonary disease. Health Psychol 1998;17:232-40. [Crossref] [PubMed]
- Hynninen MJ, Bjerke N, Pallesen S, et al. A randomized controlled trial of cognitive behavioral therapy for anxiety and depression in COPD. Respir Med 2010;104:986-94. [Crossref] [PubMed]
- Kunik ME, Braun U, Stanley MA, et al. One session cognitive behavioural therapy for elderly patients with chronic obstructive pulmonary disease. Psychol Med 2001;31:717-23. [Crossref] [PubMed]
- Kunik ME, Veazey C, Cully JA, et al. COPD education and cognitive behavioral therapy group treatment for clinically significant symptoms of depression and anxiety in COPD patients: a randomized controlled trial. Psychol Med 2008;38:385-96. [Crossref] [PubMed]
- Livermore N, Sharpe L, McKenzie D. Prevention of panic attacks and panic disorder in COPD. Eur Respir J 2010;35:557-63. [Crossref] [PubMed]
- de Godoy DV, de Godoy RF. A randomized controlled trial of the effect of psychotherapy on anxiety and depression in chronic obstructive pulmonary disease. Arch Phys Med Rehabil 2003;84:1154-7. [Crossref] [PubMed]
- Doyle C, Bhar S, Fearn M, et al. The impact of telephone-delivered cognitive behaviour therapy and befriending on mood disorders in people with chronic obstructive pulmonary disease: A randomized controlled trial. Br J Health Psychol 2017;22:542-56. [Crossref] [PubMed]
- Luk EK, Gorelik A, Irving L, et al. Effectiveness of cognitive behavioural therapy in a community-based pulmonary rehabilitation programme: A controlled clinical trial. J Rehabil Med 2017;49:264-9. [Crossref] [PubMed]
- Hundt NE, Renn BN, Sansgiry S, et al. Predictors of response to brief CBT in patients with cardiopulmonary conditions. Health Psychol 2018;37:866-73. [Crossref] [PubMed]
- Pollok J, van Agteren JE, Esterman AJ, et al. Psychological therapies for the treatment of depression in chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2019;3:CD012347. [PubMed]
- Pateraki E, Morris PG. Effectiveness of cognitive behavioural therapy in reducing anxiety in adults and children with asthma: A systematic review. J Asthma 2018;55:532-54. [Crossref] [PubMed]
- Parkin CL, Margereson C, McLoughlin B, et al. A pilot study of the effects of a specialist nurse-led cognitive-behavioural therapy service on coping, respiratory function and quality of life for patients with bronchiectasis. J Clin Nurs 2006;15:782-4. [Crossref] [PubMed]
- Stiles-Shields C, Kwasny MJ, Cai X, et al. Therapeutic Alliance in Face-to-Face and Telephone-Administered Cognitive Behavioral Therapy. J Consult Clin Psychol 2014. [Crossref] [PubMed]
- Mohr DC, Hart SL, Julian L, et al. Telephone-administered psychotherapy for depression. Arch Gen Psychiatry 2005;62:1007-14. [Crossref] [PubMed]
- Mohr DC, Vella L, Hart S, et al. The Effect of Telephone-Administered Psychotherapy on Symptoms of Depression and Attrition: A Meta-Analysis. Clin Psychol (New York) 2008;15:243-53. [PubMed]
- Ries AL, Bauldoff GS, Carlin BW, et al. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest 2007;131:4S-42S. [Crossref] [PubMed]
- Coleman PG, Philp I, Mullee MA. Does the use of the Geriatric Depression Scale make redundant the need for separate measures of well-being on geriatrics wards? Age Ageing 1995;24:416-20. [Crossref] [PubMed]
- Paz-Diaz H, Montes de Oca M, Lopez JM, et al. Pulmonary rehabilitation improves depression, anxiety, dyspnea and health status in patients with COPD. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists 2007;86:30-6.
- Griffiths TL, Burr ML, Campbell IA, et al. Results at 1 year of outpatient multidisciplinary pulmonary rehabilitation: a randomised controlled trial. Lancet 2000;355:362-8. [Crossref] [PubMed]
- Catalfo G, Crea L, Lo Castro T, et al. Depression, body mass index, and chronic obstructive pulmonary disease - a holistic approach. Int J Chron Obstruct Pulmon Dis 2016;11:239-49. [PubMed]
- Agbetile J, Singh S, Bradding P, et al. P147. Outcomes of pulmonary rehabilitation in severe asthma. Thorax 2011;66:A127. [Crossref]
- Kenn K, Gloeckl R, Behr J. Pulmonary rehabilitation in patients with idiopathic pulmonary fibrosis--a review. Respiration 2013;86:89-99. [Crossref] [PubMed]
- Bhandari NJ, Jain T, Marolda C, et al. Comprehensive pulmonary rehabilitation results in clinically meaningful improvements in anxiety and depression in patients with chronic obstructive pulmonary disease. Journal of cardiopulmonary rehabilitation and prevention 2013;33:123-7. [Crossref] [PubMed]
- Garrod R, Marshall J, Barley E, et al. Predictors of success and failure in pulmonary rehabilitation. Eur Respir J 2006;27:788-94. [Crossref] [PubMed]
- Pierobon A, Sini Bottelli E, Ranzini L, et al. COPD patients' self-reported adherence, psychosocial factors and mild cognitive impairment in pulmonary rehabilitation. Int J Chron Obstruct Pulmon Dis 2017;12:2059-67. [Crossref] [PubMed]
- Harris D, Hayter M, Allender S. Improving the uptake of pulmonary rehabilitation in patients with COPD: qualitative study of experiences and attitudes. The British journal of general practice: the journal of the Royal College of General Practitioners 2008;58:703-10.
- Williams MT, Cafarella P, Paquet C, et al. Cognitive Behavioral Therapy for Management of Dyspnea: A Pilot Study. Respir Care 2015;60:1303-13. [Crossref] [PubMed]
- Wiles L, Cafarella P, Williams MT. Exercise training combined with psychological interventions for people with chronic obstructive pulmonary disease. Respirology 2015;20:46-55. [Crossref] [PubMed]
- Farver-Vestergaard I, O'Toole MS, O'Connor M, et al. Mindfulness-based cognitive therapy in COPD: a cluster randomised controlled trial. Eur Respir J 2018.51. [PubMed]
- Moayeri F, Dunt D, Hsueh YA, et al. Cost-utility analysis of telephone-based cognitive behavior therapy in chronic obstructive pulmonary disease (COPD) patients with anxiety and depression comorbidities: an application for willingness to accept concept. Expert Rev Pharmacoecon Outcomes Res 2019;19:331-40. [Crossref] [PubMed]
- Julian LJ, Gregorich SE, Earnest G, et al. Screening for depression in chronic obstructive pulmonary disease. COPD 2009;6:452-8. [Crossref] [PubMed]
- Cheung G, Patrick C, Sullivan G, et al. Sensitivity and specificity of the Geriatric Anxiety Inventory and the Hospital Anxiety and Depression Scale in the detection of anxiety disorders in older people with chronic obstructive pulmonary disease. Int Psychogeriatr 2012;24:128-36. [Crossref] [PubMed]
- Molloy DW, Alemayehu E, Roberts R. Reliability of a Standardized Mini-Mental State Examination compared with the traditional Mini-Mental State Examination. Am J Psychiatry 1991;148:102-5. [Crossref] [PubMed]
- State of Queensland (Queensland Health) TALF. Better living with Chronic Obstructive Pulmonary Disease: A patient guide. 2012.
- Padesky CA, Mooney KA. Clinical tip: Presenting the cognitive model to clients. International Cognitive Therapy Newsletter, 6, 13-14 Retrieved from 1990.www.padesky.com
- Singh VP, Rao V, V P, et al. Comparison of the effectiveness of music and progressive muscle relaxation for anxiety in COPD--A randomized controlled pilot study. Chron Respir Dis 2009;6:209-16. [Crossref] [PubMed]
- Cafarella PA, Effing TW, Usmani ZA, et al. Treatments for anxiety and depression in patients with chronic obstructive pulmonary disease: a literature review. Respirology 2012;17:627-38. [Crossref] [PubMed]
- Jones PW, Quirk FH, Baveystock CM, et al. A self-complete measure of health status for chronic airflow limitation. The St. George's Respiratory Questionnaire. Am Rev Respir Dis 1992;145:1321-7. [Crossref] [PubMed]
- Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695-9. [Crossref] [PubMed]
- Celli BR, Cote CG, Lareau SC, et al. Predictors of Survival in COPD: more than just the FEV1. Respir Med 2008;102 Suppl 1:S27-35. [Crossref] [PubMed]
- Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis 2011;8:89-99. [Crossref] [PubMed]
- Boutou AK, Tanner RJ, Lord VM, et al. An evaluation of factors associated with completion and benefit from pulmonary rehabilitation in COPD. BMJ Open Respir Res 2014;1:e000051. [Crossref] [PubMed]
- Cassidy S, Turnbull S, Gardani M, et al. Attendance at pulmonary rehabilitation classes: an exploration of demographic, physiological and psychological factors that predict completion of treatment. Chron Respir Dis 2014;11:95-102. [Crossref] [PubMed]
- Huhn M, Tardy M, Spineli LM, et al. Efficacy of pharmacotherapy and psychotherapy for adult psychiatric disorders: a systematic overview of meta-analyses. JAMA Psychiatry 2014;71:706-15. [Crossref] [PubMed]
- Tolin DF. Can Cognitive Behavioral Therapy for Anxiety and Depression Be Improved with Pharmacotherapy? A Meta-analysis. Psychiatr Clin North Am 2017;40:715-38. [Crossref] [PubMed]
- Coquart JB, Le Rouzic O, Racil G, et al. Real-life feasibility and effectiveness of home-based pulmonary rehabilitation in chronic obstructive pulmonary disease requiring medical equipment. Int J Chron Obstruct Pulmon Dis 2017;12:3549-56. [Crossref] [PubMed]



