Caution for acute submassive pulmonary embolism with syncope as initial symptom: a case report
Introduction
Pulmonary embolism (PE) may escape prompt diagnosis since clinical symptoms and signs are nonspecific. It is estimated that approximately 650,000 cases occur annually in the United States (1). Clinically, PE mainly manifests as chest pain, shock and hypotension, and only about 10% of patients have syncope as the initial symptom (2,3). Syncope as the presenting symptom of PE has proven to be a difficult clinical correlation to make. We report on the diagnosis and treatment of a patient with PE with syncope as the initial symptom.
Case report
A 62-year-old woman with no history of disease was admitted to emergency department of Affiliated Hospital of Xi’an Medical University after she had a syncopal episode in her home. The patient kept her right upper limb inactive for 1 week because of right clavicle’s fracture until she suddenly collapsed while standing and lost consciousness for approximately ten minutes. She recovered spontaneously but was extremely weak and dyspneic. She was also diaphoretic and tachypneic, but denied any associated chest pain or palpitations. No seizures were witnessed, and she experienced no incontinence.
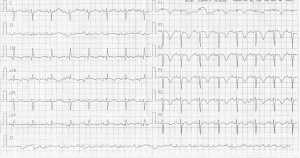
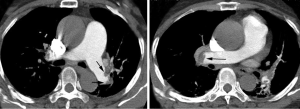
On admission to Pulmonary Department, physical examination revealed a diaphoretic and dyspneic patient without focal neurologic findings. Her heart rate was regular at 96 beats per minute, her blood pressure was 131/82 mmHg without orthostatic changes, and her respiratory rate was 32 breaths per minute. The room air oxygen saturation was 86-90%, and arterial blood gas analysis in room air revealed hypoxemia (PO2 =47 mmHg) with an elevated alveoli-arterial oxygen gradient (A-a O2 gradient). Examination of her head and neck was normal. The results of chest wall examination revealed normal breath sounds bilaterally. The findings of heart, abdominal and central nervous system examinations were unremarkable. There were no edemas in lower extremities. Levels of serum electrolytes, glucose, blood urea and creatinine, and complete blood counts were normal. Results of a computed tomographic scan of her head were negative for bleeding, aneurysm or an embolic event. A Doppler scan of the legs was normal. An electrocardiogram showed a regular rhythm consistent with sinus rhythm; there were Q and T waves in lead III and an S wave in lead I, T wave inversion in lead V1-V6 (Figure 1). Because PE cannot be excluded and anticoagulant with low molecular weight heparin was performed immediately. A transthoracic echocardiogram revealed normal left ventricle function without a patent foramen ovale, an atrial septal defect or a ventricular septal defect and normal right ventricle function. The level of D-dimer was 1.5 mg/L (normal value 0-1 mg/L). The value of BNP was 170 pg/mL (normal level 0-100 pg/mL) and troponin was 0.1 mL (normal level 0-0.04 mL). An enhanced chest computed tomography (CT) scan revealed filling defects in the right main pulmonary and left inferior pulmonary arteries (Figure 2).
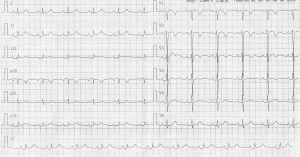
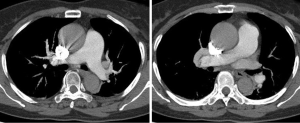
With a diagnosis of acute submassive PE (4), the patient underwent thrombolytic therapy with urokinase 1,000,000 IU over a 2-hour period, which brought about immediate improvement in the patient’s condition. Anticoagulant with low molecular weight heparin and an oral anticoagulant were continued when APTT decreased within two times of normal value. The following days, the electrocardiograms showed Q and T waves in lead III and an S wave in lead I were improved, T wave in lead V5-V6 were normal (Figure 3). Her symptoms improved dramatically, her respiratory rate decreased and her O2 saturation rose from 85% to 95%. An enhanced chest CT scan reexamination showed filling defects in the right main pulmonary and left inferior pulmonary arteries were remarkably improved after 12 days (Figure 4). After a 16-day course of hospital treatment, she was discharged on oral warfarin therapy. The patient’s long-term follow-up was performed by Pulmonary Department, and we learned that the patient was well for four months after that episode without any evidence of recurrent syncope or PE.
Discussion
The diagnosis of acute PE is amongst the most challenging problems encountered in clinical practice. Clinical assessment is necessary to estimate a pre-test probability of PE and determine what (if any) diagnostic testing is required. The most common symptoms of PE are dyspnea (82%), pleuritic chest pain (49%), and cough (20%) (5). Syncope is an uncommon presentation of PE, occurring in only 10% of patients. However, no clinical features can be used to rule in or rule out PE without further testing (6). There are several possible reasons why cause syncope: (I) acute right heart failure and damaged pulmonary blood perfusion causing decreased filling of the left ventricle, with resulting hypotension, bradycardia and cerebral circulation disturbance (7); (II) reflex syncope caused by bradycardia due to vagal stimulation and by peripheral vascular distention due to suppression of sympathetic nerves (8); and (III) syncope caused by an atrioventricular block induced by MPE (9).
Embolus of PE can be from superior vena cava or inferior vena cava. However, ~79% of patients who present with PE have evidence of deep venous thrombosis in their legs, if deep venous thrombosis is not detected in such patients, it is likely that the whole thrombus has already detached (10). The exact number of the symptoms and signs of deep vein thrombosis in patients with a diagnosis of PE is not clear, but one study reported deep vein thrombosis in 62% of patients with PE (11). The patient lacked activities for one week because of right clavicle’s fracture, it is possible embolus existed in inferior vena cava and whole thrombus detached from blood vessel, so it was not detected by ultrasound.
The electrocardiograph (ECG) is still simple, easy to use and useful in the diagnosis of acute PE. Surface ECG readings are altered in about 70% of PE (12). Numerous ECG findings have been reported, with sinus tachycardia being the most common (13). Findings such as the S1Q3T3 pattern lack sensitivity and specificity, and also show no correlation with the severity of PE (13,14). Several studies have stated that T-wave inversion in lead III, aVF and precordial leads is most often associated with massive PE and/or PE with right ventricle (RV) dysfunction, ascribing a high sensitivity, specificity, positive and negative predictive value to these findings (14-17). Negative T waves in both leads III and V1 have been reported to accurately differentiate acute PE from acute coronary syndrome (15). The changes between the initial and posttreatment ECG from this patient are obvious, the role of ECG on diagnosing PE is not ignored by clinicians.
Management with anticoagulants alone is typically sufficient for low-risk patients, more aggressive treatments such as thrombolysis, embolectomy, and inferior vena cava (IVC) filters are recommended for higher-risk patients. Thrombolytic therapy should be considered in all patients with massive PE and hypotension associated with deep vein thrombosis in the popliteal area or higher (18). The main indications for thrombolytic therapy include ongoing hypoxia, respiratory distress, pulmonary hypertension, and right heart failure because thrombolytic therapy often achieves an impressive and almost an immediate clinical benefit in these clinical settings (19). Our patient had emerged ongoing hypoxia and breathlessness on admission, so she had the indications for thrombolytic therapy. In fact her symptoms were improved dramatically after thrombolysis.
In conclusion, the occurrence of syncope as the sole initial symptom in a previously healthy patient with no hemodynamic instability following admission is extremely rare. In this situation, the raised awareness of diagnosis and knowledge concerning the clinical presentation of pulmonary thromboembolism are key factors in ensuring an immediate diagnosis and adequate intervention.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Wolfe TR, Allen TL. Syncope as an emergency department presentation of pulmonary embolism. J Emerg Med 1998;16:27-31. [PubMed]
- Calvo-Romero JM, Pérez-Miranda M, Bureo-Dacal P. Syncope in acute pulmonary embolism. Eur J Emerg Med 2004;11:208-9. [PubMed]
- Blaho KE, Merigian KS, Winbery SL, et al. Foreign body ingestions in the Emergency Department: case reports and review of treatment. J Emerg Med 1998;16:21-6. [PubMed]
- Jaff MR, McMurtry MS, Archer SL, et al. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation 2011;123:1788-830. [PubMed]
- Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet 1999;353:1386-9. [PubMed]
- West J, Goodacre S, Sampson F. The value of clinical features in the diagnosis of acute pulmonary embolism: systematic review and meta-analysis. QJM 2007;100:763-9. [PubMed]
- Gossage JR. Early intervention in massive pulmonary embolism. A guide to diagnosis and triage for the critical first hour. Postgrad Med 2002;111:27-8, 33-4, 39-40 passim. [PubMed]
- Eldadah ZA, Najjar SS, Ziegelstein RC. A patient with syncope, only “vagally” related to the heart. Chest 2000;117:1801-3. [PubMed]
- Elias J, Kuniyoshi R, Moulin B, et al. Syncope and complete atrioventricular block related to pulmonary thromboembolism. Arq Bras Cardiol 2004;83:438-41; 434-7.
- Tapson VF. Acute pulmonary embolism. N Engl J Med 2008;358:1037-52. [PubMed]
- Köhn H, Mostbeck A, Bachmayr S, et al. 99mTc-DTPA aerosol for same-day post-perfusion ventilation imaging: results of a multicentre study. Eur J Nucl Med 1993;20:4-9. [PubMed]
- Kosuge M, Kimura K, Ishikawa T, et al. Electrocardiographic differentiation between acute pulmonary embolism and acute coronary syndromes on the basis of negative T waves. Am J Cardiol 2007;99:817-21. [PubMed]
- Laack TA, Goyal DG. Pulmonary embolism: an unsuspected killer. Emerg Med Clin North Am 2004;22:961-83. [PubMed]
- Cheng AS, Money-Kyrle A. Instructive ECG series in massive bilateral pulmonary embolism. Heart 2005;91:860-2. [PubMed]
- Punukollu G, Gowda RM, Vasavada BC, et al. Role of electrocardiography in identifying right ventricular dysfunction in acute pulmonary embolism. Am J Cardiol 2005;96:450-2. [PubMed]
- Sarin S, Elmi F, Nassef L. Inverted T waves on electrocardiogram: myocardial ischemia versus pulmonary embolism. J Electrocardiol 2005;38:361-3. [PubMed]
- Torbicki A, Perrier A, Stavros K, et al. Guidelines on the diagnosis and management of acute pulmonary embolism. G Ital Cardiol (Rome) 2009;10:303-47. [PubMed]
- Linn BJ, Mazza JJ, Friedenberg WR. Treatment of venous thromboembolic disease. A pragmatic approach to anticoagulation and thrombolysis. Postgrad Med 1986;79:171-80. [PubMed]
- Gallus AS. Thrombolytic therapy for venous thrombosis and pulmonary embolism. Baillieres Clin Haematol 1998;11:663-73. [PubMed]


