|
Original Article
Changing trend of antimicrobial resistance among pathogens isolated from lower respiratory tract at a university-affiliated hospital of China, 2006-2010
1Department of Laboratory Medicine, the First Affiliated Hospital of Nanjing Medical University, Nanjing 210029, China; 2National Key Clinical Department of Laboratory Medicine, Nanjing 210029, China; 3Department of Respiratory Medicine, the First Affiliated Hospital of Nanjing Medical University, Nanjing 210029, China
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract
Objective: To investigate the distribution and the antimicrobial resistance of pathogens in lower respiratory tract infection from 2006 to 2010. Methods: The sputum specimens from inpatients with lower respiratory tract infection in the First Affiliated Hospital of Nanjing Medical University during the past five years were cultured and identified; the antimicrobial resistance was analyzed by the software WHONET 5.4. Results: A total of 12,191 isolates were characterized in sputum samples: 73.5% were Gram-negative bacteria, 13.7% were Gram-positive bacteria, and 12.8% were fungi. The isolation rate of Acinetobacter was significantly increasing from 12.8% in 2006 to 26.4% in 2010. The Gram-negative bacterial resistance rate to the second and third generation cephalosporin increased year by year. Decreasing trend, 78.7% in 2006 decreased to 63.5% in 2010 (R2=0.93 and P<0.01), in resistance to clindamycin against Staphylococcus aureus was observed. Worth noting is the drug resistance of Acinetobacter and Klebsiella pneumoniae to carbapenem significantly increased (R2>0.3 and P≤0.05). Conclusions: The antimicrobial resistance of pathogens in lower respiratory tract infection increased in recent years. The hospitals and government departments should strengthen management of the use of some antibiotics, such as the second/third generation cephalosporin and carbapenem, in order to enhance the effectiveness of medication. Key words
Antimicrobial resistance; Acinetobacter; Staphylococcus aureus; lower respiratory tract; carbapenem
J Thorac Dis 2012;4(3):284-291. DOI: 10.3978/j.issn.2072-1439.2012.02.04 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Introduction
Lower respiratory tract infections (LRTI) are common bacterial infections among patients in hospital and result in high overall mortality (1,2). It is reported that LRTI account for 3% to 5% of deaths in adults, especially over the age of 60 years, most common pathogens of LRTI are Pseudomonas, Acinetobacter, Klebsiella, Citrobacter, and Escherichia coli (3-5). At present, therapy for community-acquired lower respiratory tract infections (LRTI) is often empirical, and how to choose an effective antimicrobial agent is a new challenge to the clinicians, as the composition and the resistance to antimicrobial agents of infection pathogens was changing frequently. The knowledge of likely prevalent strains along with their antimicrobial resistance pattern will help in better management of patients and framing the antibiotic policy.
The present study, the pathogens profile and their antimicrobial resistance in lower respiratory tract infection from January 2006 to December 2010 in the First Affiliated Hospital of Nanjing Medical University was retrospectively reviewed in order to provide evidence for clinical therapy. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Materials and methods
Patients
Patients with lower respiratory tract infections (LRTI) were enrolled from January 2006 to December 2010 in the First Affiliated Hospital of Nanjing Medical University (6). The sputum
specimens of only new patients who were enrolled for the first
time were included in the study. Single or mixed growth from
one patient and consecutive samples from the new patients were
included in the study. If the repeat sample was received from the
same patient who was already enrolled, it was not included in the
study. Acquisition and inoculation of the sputum samples were all
accorded to standard operating procedures, following Clinical and
Laboratory Standards Institute guidelines (CLSI) (7).
Bacterial identification and antimicrobial susceptibility testing
The bacterial isolates were identified and performed antimicrobial
susceptibility testing predominantly through disk susceptibility
testing, supplemented by the Vitek 2 system, following Clinical
and Laboratory Standards Institute guidelines (CLSI) (7).
Antimicrobial agents tracked include: penicillins (penicillin G),
cephalosporins (cefazolin, cefuroxime, ceftriaxone, ceftazidime,
and cefepime), monobactams (aztreonam), cephamycins
(cefoxitin), carbapenems (imipenem and meropenem),
compound agents (amoxicillin/clavulanate, ampicillin/
sulbactam, piperacillin/tazobactam, cefoperazone/sulbactam),
aminoglycosides (amoxicillin), fluoroquinolones (ciprofloxacin
and levofloxacin), sulfonamides (cotrimoxazole), macrolides
(erythromycin), lincomycins (clindamycin), glycopeptides
(vancomycin and teicoplanin). Microbiologic data were
extracted from the laboratory information system and converted
centrally into a standard format using WHONET 5.4 (WHO,
Geneva, Switzerland), with duplicates eliminated according to
the guidelines of the CLSI. The following controls strains were
included: Escherichia coli ATCC 25922, Pseudomonas aeruginosa
ATCC 27853, Staphylococcus aureus ATCC 25923.
Statistical analysis
WHONET 5.4 microbiology laboratory data management
software World Health Organization recommended was used for
statistical analysis. Changing trends in this use were analyzed by
linear regression (R2>0.3 and P≤0.05) (8). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Results
Pathogens distribution
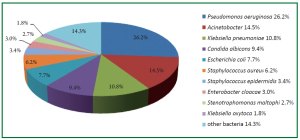
During the study period, a total of 12,191 isolates were
characterized in sputum samples from all patients with LRTI.
Of these pathogens, 73.5% (8956/12191) were Gram-negative
bacteria, 13.7% (1671/12191) were Gram-positive bacteria and
12.8% (1555/12191) were fungi. The top 10 frequently isolated
pathogens were Pseudomonas aeruginosa (26.2%), Acinetobacter
(14.5%), Klebsiella pneumoniae (10.8%), Candida albicans
(9.4%), Escherichia coli (7.7%), Staphylococcus aureus (6.2%),
Staphylococcus epidermidis (3.4%), Enterobacter cloacae (3.0%),
Stenotrophomonas maltophi (2.7%) and Klebsiella oxytoca (1.8%)
(Figure 1). These 10 species accounted for 85.7% of the total
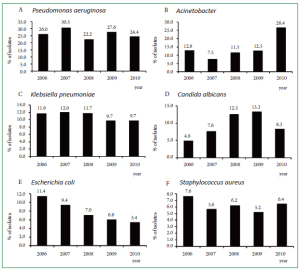
number of isolates. Figure 2 (A-F) showed the changing trend of
the top 6 pathogens from 2006 to 2010. Pseudomonas aeruginosa
accounted for top 1 from 2006 to 2009. The isolation rate of
Acinetobacter was significantly increased from 12.8% in 2006 to
26.4% in 2010, more than Pseudomonas aeruginosa (24.4%) in
2010.
Antimicrobial resistance of Gram-negative bacteria
With regard to to Gram-negative bacteria (GNB), the resistance rate of all GNB to cephalosporins showed the increasing
trend although not all showed significantly. Among GNB, the
resistance rates were more than 90% in 2010 of Escherichia coli
to all cephalosporins, a significant increase in the resistance
rate with time was found for cefuroxime (R2=0.86 and P=0.02)
and ceftriaxone (R2=0.78 and P=0.04) (Table 1). Klebsiella
pneumonia had a more than 80% resistance rate in 2010 to
all cephalosporins and significant increasing trends were
observed to ceftazidime (R2=0.91 and P=0.01) and ceftriaxone
(R2=0.95 and P<0.01) (Table 2). Acinetobacter resistance rate
to all cephalosporins were more than 85% in 2010, significant
increased against cefepime (R2=0.78 and P=0.05) (Table 3).
Significant increasing trends were also observed in Citrobacter
to ceftazidime (R2=0.80 and P=0.04) and ceftriaxone (R2=0.82
and P=0.03) and Pseudomonas aeruginosa to ceftazidime
(R2=0.81 and P=0.04) (Table 4, Table 5). The same increasing
trend was also found in GNB against aztreonam. Citrobacter,
Pseudomonas aeruginosa and Acinetobacter resistance rate were
all significant increased to aztreonam (R2>0.3 and P≤0.05)
and were all more than 60% in 2010 (Table 3, Table 4, Table
5). Worth noting is the drug resistance to carbapenem
including imipenem and meropenem has become increasingly
serious. Significant increasing trends were found to imipenem
(R2=0.78 and P=0.05, R2=0.79 and P=0.04, respectively)
and meropenem (R2=0.81 and P=0.04, R2=0.80 and P=0.04,
respectively) of Klebsiella pneumoniae and Acinetobacter (Table 2,3).
Most GNB resistance rate increased to compound agents
including ampicillin/sulbactam, piperacillin/tazobactam, cefoperazone/sulbactam except Pseudomonas aeruginosa
remained stable. Among them, Citrobacter to ampicillin/
sulbactam and piperacillin/tazobactam and Acinetobacter
to piperacillin/tazobactam and cefoperazone/sulbactam
showed significant increasing trends (R2>0.3 and
P≤0.05) (Table 3,4). The only decreasing trend among
GNB was observed in resistance to amoxicillin against
Escherichia coli (R2=0.88 and P=0.01) while increasing trends
against Pseudomonas aeruginosa (R2=0.82 and P=0.03) and
Acinetobacter (R2=0.84 and P=0.03) (Table 1, 3, 5).
Antimicrobial resistance of Gram-positive bacteria
With regard to Gram-positive bacteria (GPB), vancomycin
was extremely effective against the most common bacteria
(Staphylococcus aureus). No vancomycin-resistant isolate of
Staphylococcus aureus was found. Few GPB was found resistant to
teicoplanin. The GPB resistance rate remained high to penicillins,
cephalosporins, piperacillin/tazobactam, levofloxacin and
erythromycin and was more than 70% in 2010. The decreasing
trend occurred in resistance rate to clindamycin (R2=0.93 and
P<0.01) against Staphylococcus aureus (Table 6).
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Discussion
In this study, Gram-negative bacteria were the predominant
pathogens causing LRTI. During the study period of the
5 years, the proportion of Gram-negative bacteria changed little.
Candida infections had significantly increased while Grampositive
bacteria decreased. Opportunistic pathogens (such as
Candida albicans) ratio gradually increased, which caused by
dysbacteria because of long-term use of antibiotics. Pseudomonas
aeruginosa remained the most common pathogen (26.5-30.5%)
from 2006 to 2009. Wang et al. (8) also reported Pseudomonas
aeruginosa was the most common pathogens causing hospitalacquired
lower respiratory tract infections in North China and
as found in a study in North America (9). The rate of isolation
of Acinetobacter increased from 7.5% (2007) to 26.4% (2010)
becoming the most common isolate in 2010 in this study. As
opportunistic pathogen, Acinetobacter baumannii-infected
patients are mainly immunocompromised critically ill patients,
the elderly or the patients using immunosuppressive drugs. In
this study, Most of Acinetobacter baumannii infection patients
came from department of respiratory medicine, neurology, and
intensive care units (ICU), because the patients in these sections
were all in critical condition, tracheostomy, long hospital stay,
lower immune defense, or suffering from a variety of disease, the
bacteria was easy to cross-infection in the form of droplets or
aerosols. And the severe resistance of Acinetobacter baumannii
resulted in the hospital stay of patients who infected with
Acinetobacter baumannii prolonged resulting in increased crossinfection,
so that the isolation rate increased.
The resistance rate of GNB to most antibiotics showed the
increasing trend especially for cephalosporins and carbapenems.
Escherichia coli, Klebsiella pneumonia and Acinetobacter had high
resistance rates to cephalosporins, which were all more than
70% in 2010. This is probably related to the irrational use of
cephalosporins in our hospital in recent years. GNB resistant
to cephalosporins had been very serious in China, which is
different in Europe and America (10-12). Carbapenems was
considered as the most effective antibiotic agent against Gramnegative
bacteria in the past. But now, the resistance rates of
GNB to carbapenems were increasing gradually. In this study,
Klebsiella pneumonia resistance rate significant increased, which
was more than 25% in 2010, possibly related to the prevalence
of KPC carbapenemase (13). As more and more multi-resistant
Pseudomonas aeruginosa, the study found that the efflux pump on
the cell membrane of Pseudomonas aeruginosa is one of the main
reasons of its multi-drug resistance, the outer membrane protein
OprM is the most common among six efflux pumps (14).
Due to the wide application of broad-spectrum antibiotics,
the resistance rates of Acinetobacter to most antibiotics have
continually increased during recent decades, resistance to
carbapenems is most concerning (15). The MYSTIC program
of 2007 demonstrated that 74.1% of isolates were susceptible to
meropenem and 78.9% were susceptible to imipenem in Europe,
compared with much lower susceptibilities of 51.3% and 52.0%
in several Asian countries in the SENTRY program of 2006-2007
(16,17). The emergence of carbapenem-resistant Acinetobacter
has been described as the sentinel event of antimicrobial
resistance. In this study, more than 85% resistance rate was
observed in Acinetobacter against carbapenems resulting in the
isolates rate of multidrug-resistant Acinetobacter increased year
by year. The results were similar with the Chinese Meropenem
Surveillance Study (CMSS), which took place from 2003 to
2008, defined a serious carbapenem resistance problem in
Acinetobacter. The major mechanism of carbapenem resistance in Acinetobacter is production of OXA β-lactamases, primarily
OXA-23, OXA-66 and OXA-58 (13).
No vancomycin-resistant isolate of Staphylococcus aureus
was found in this 5-year study. Decreasing trend in resistance to
clindamycin against Staphylococcus aureus was observed. This
may related to strengthen the clindamycin-induced experimental
in our hospital.
Although antimicrobial agents are an important therapeutic
weapon in infectious disease (18), the selective pressure, which
may lead to antibiotics resistance, was imposed at the same
time. In general, new resistances would be detected soon after
introduction of new antimicrobial agents. To cope with resistant
bacteria, new antibiotics must be developed, however, it became
increasingly difficult to develop new ones (19). To prolong the
effectiveness of currently available antimicrobial agents, it is
essential to know the pathogen distribution and their antibiotic
resistance patterns (20). The pathogen profile and their
antibiotic resistance patterns was identified by the present study,
it would be help the clinicians to facilitate decision-making.
Our investigation showed that Gram-negative bacteria
were the predominant pathogens and that antimicrobial
resistance is severe in our hospital, which may be related to
illegitimate antibiotic use. The treatment of patients with
bacterial LRTI is, therefore, becoming more complicated.
In particular, the emergence of resistance to commonly
prescribed antimicrobial agent by respiratory tract pathogens
has compounded the problem. These results highlight the
need for systematic interventions to ensure more consistent
application of recommended guidelines for antimicrobial use,
especially for the second/third generation cephalosporin and
carbapenem. The researchers from our hospital found that
the total annual consumption of carbapenem has markedly
increased. It increased 192 times in 2009 compared with 2001.
The consumption of imipenem/cilastatin, meropenem, and
total carbapenem is associated with Acinetobacter resistance to
piperacillin-tazobactam, ceftazidime, cefepime, amikacin, and
levofloxacin (21). The good news is our hospital had formulated
the related policy that only the specified senior doctors have the
prescription right of above antibiotics.
This 5-year study demonstrated that antimicrobial resistance
of pathogens isolated from lower respiratory tracts has become a
serious problem with some antibiotics, the hospitals and related
government departments should strengthen management of the
use of some antibiotics in order to enhance the effectiveness of
medication. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Acknowledgements
This research was funded by the National Natural Science Foundation
of China (No. 81000754) and a grant from the Key Laboratory for
Laboratory Medicine of Jiangsu Province of China (No. XK201114). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
References
Cite this article as: Xia W, Chen Y, Mei Y, Wang T, Liu G, Gu B, Pan S.
Changing trend of antimicrobial resistance among pathogens isolated from
lower respiratory tract at a university-affiliated hospital of China, 2006-2010.
J Thorac Dis 2012;4(3):284-291. doi: 10.3978/j.issn.2072-1439. 2012.02.04
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||