Video-assisted thoracoscopic left upper lobe apical trisegmentectomy with the Harmonic scalpel
Introduction
Segmental resection is a useful procedure to preserve respiratory function. During the past decade, thoracoscopic lobectomy for lung cancer has been widely accepted, but video-assisted thoracoscopic surgery (VATS) segmentectomies are usually more complex procedures than lobectomies. With the gained experience in the field of thoracoscopic surgery, A few thoracic surgeons have progressively adopted VATS segmentectomy to preserve lung parenchyma. Several papers have reported the benefits of thoracoscopic segmentectomy compared with open segmentectomy. Multiple studies of the Harmonic scalpel scalpel have shown it to be safe and to minimize blood loss in various surgeries, such as vaginal hysterectomies and laparoscopic nephrectomies. The purpose of this video was to show our institution’s techniques and experience with the Harmonic scalpel scalpel during VATS segmentectomy (Figure 1).
The technique of VATS segmentectomy described here is that which is currently employed in the unit of thoracic surgery at The First People’s Hospital of Yunnan Province, Kunming University of Science and Technology.
Clinical summary other section
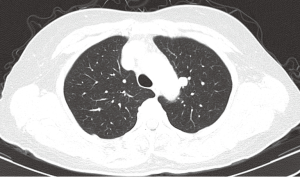
A 56-year-old woman felt chest pain with tenderness before half a year. She presented with a finding of a left upper lobe lesion on CT scanning. Past medical history included a high blood pressure 4 years. CT imaging revealed a 9.7 mm AP × 9.3 mm TR, lesion in the left upper lobe (LUL) which may be adherent to the aorto (Figures 2,3). Bronchoscopy and brushings did not show any bronchial abnormal. Lung function was assessed via formal spirometry with a FEV1 of 1.97 (89% predicted), a FVC of 2.04 (81% predicted) and an FEV1/FVC ratio of 96.5%. The patient was proposed for VATS. She was performed video-assisted thoracoscopic left upper lobe apical trisegmentectomy. The frozen pathological examination revealed a hamartoma during opration. The surgical time was 70 min. Postoperative hospital stay was 4 days.
Technique other section
Positioning and incisions
The patient is placed in the right lateral decubitus position with a slight posterior tilt under single-lung ventilation. The surgeon stands on the anterior side of the patient. The 10-mm camera port is made at the seventh intercostal space between the anterior and mid-axillary line. The utility incision (3.0 cm in length) is placed at the third intercostal space in the anterior axillary line. The utility incision is located directly over the superior pulmonary vein for a left upper lobe apical trisegmentectomy. An additional 10-mm posterior port is made at the ninth intercostal space left below the tip of the scapula.
The first step in the procedure is to confirm resectability and identify invasion of the chest wall, pleurae and hilar structures including the aorta, pulmonary artery and bronchus.
The order of the steps of the operation is as follows: posterior, anterior, and superior pleurae over the hilum; upper division vein; anterior trunk; posterior artery; bronchus; and the fissure.
Step 1: tumor palpation
Exposure: move the lung toward the access port with a ringed forceps placed through the posterior port.
Place the thoracoscope in the camera port with the side arm straight up.
Carefully palpate and examine the tumor to be certain a sublobar resection constitutes optimal cancer treatment. This is done by corroborating the tumor size and confirming that tumor is far enough away from the lingula so that the margins will be adequate if a trisegmentectomy is performed.
Step 2: takedown inferior pulmonary ligament and posterior mediastinal pleura
Exposure: hold the left lower lobe superiorly with a ring clamp through the posterior incision.
The thoracoscope is aimed anteriorly with the 30-degree lens pointed posteriorly. The suction catheter introduced from the utility incision. Transect the inferior pulmonary ligament with Harmonic scalpel, which is brought through the posterior incision. The tip of the suction catheter should be held close to the Harmonic scalpel tip to aid in blunt dissection and remove the smoke created. Harmonic scalpel transects the ligament up to the level of the right inferior pulmonary vein. Retract the left lower lobe lung anteriorly to show posterior mediastinal pleura. Continue opening the pleural superiorly until the apical hilum.
Step 3: open anterior hilum and aortopulmonary window
Exposure: retract the left upper lobe posteriorly with a ring clamp through the posterior port.
Place the thoracoscope in the camera port with the side arm to the left to look at anterior hilar structures. Aim the thoracoscope slightly anteromedially and the lens slightly posteriorly. Open the mediastinal pleura over the anterior hilum with the Harmonic scalpel and the suction catheter. This defines the venous drainage from the upper division of the left upper lobe (LUL). Dissect superiorly to the level of the aortopulmonary window. Removal of the level 5 nodes facilitates exposure of the vessels and prepares the superior and posterior aspect of the anterior trunk for subsequent transection.
Step 4: upper division pulmonary vein division
Exposure: retract the left upper lobe posteriorly with a ring clamp through the posterior port.
The thoracoscope is aimed anteriorly and slightly medially, and the lens is pointed toward the mediastinum and slightly posteriorly.
Bring the suction catheter through the utility incision while passing the Harmonic scalpel through the posterior incision. With the Harmonic scalpel and suction catheter, dissect the inferior border of the Superior pulmonary vein. Carefully identify and preserve the lingular veins. Mobilize the upper division pulmonary vein. Extension between the vein and the bronchus with right-angle clamp farther than the anvil is performed, since this approach ensures that the stapler completely crosses the vein before stapling. Divide the upper division pulmonary vein using an endovascular stapler placed through the posterior port while retracting the lung with a ring forceps placed through the utility incision. The stapler is closed and fired. After transecting the vein, the left upper lobe bronchus and anterior trunk can be seen.
Step 5: anterior trunk
Exposure: the lung is retracted laterally and inferiorly through the posterior incision.
The thoracoscope is aimed anteriorly, and the lens is pointed slightly posteriorly. After stapling the superior pulmonary vein, the anterior trunk of the pulmonary artery (PA) is readily visualized. Incise the lymphatics on the superior aspect of the LUL bronchus, and remove lymph nodes to better expose the PA. Remove the lymph node between the bifurcation of the anterior trunk and the main PA for easier isolation of the anterior trunk.
A right-angle clamp introduced through the utility incision passes around the anterior trunk of the PA. Adjust the angle of the camera to allow complete visualization of the right-angle clamp as it encircles the anterior trunk. There should be little or no resistance to the passage of the right-angle clamp after prior dissection of the superior aspect of the hilum. The right-angle clamp is spread widely to create an adequate tunnel for subsequent stapler placement.
The vascular stapler is brought through the posterior incision and placed across the anterior trunk. The anvil of the stapler should be placed in the tunnel between the PA and the anterior trunk. The anterior trunk was transected.
Step 6: posterior artery division
Exposure: a ring clamp through the posterior incision lifts the upper lobe to expose the posterior segmental artery to the left upper lobe.
The thoracoscope is positioned with the 30-degree lens pointing medially, and the lens pointing posteriorly. Begin a combination of blunt and sharp dissection on the surface of the main PA to expose the posterior segmental artery to the left upper lobe. The right-angle clamp is spread widely to create an adequate tunnel for subsequent stapler placement. Divide the posterior segmental artery with an endovascular stapler introduced through the posterior port.
Step 7: bronchus division
Exposure: retract the lung toward posteriorly with a ringed forceps through the posterior incision to gain as much length on the bronchus as possible, and put it under some mild tension in the vertical plane.
Dissect the anterior aspect of the bronchus. Identify the upper division bronchus in the fissure, and sweep all peribronchial tissue up onto the bronchus with the Harmonic scalpel and suction catheter. This helps to identify the carina between the upper division bronchus and the lingular bronchus.
Dissect the anterior aspect of the upper division bronchus. The right-angle clamp is spread widely to create an adequate tunnel. Introduce a silk thread across the upper division bronchus and pull toward the utility incision for subsequent stapler placement. Use an endobronchial stapler placed through the posterior port to divide the upper division bronchus. Reinflation of the lung after closed stapler helps to ensure that the correct bronchus is occluded and that there is no impingement on lingual bronchi. It must be ensured that there are no devices within the airway, and fire the stapler.
Step 8: complete the fissure between the upper division and the lingula
The anesthesiologist should inflate the left lung. The lingula inflates adequately. The bronchus for the upper division can be divided and the lingula ventilated to determine where to place the staples to separate the upper division. At the same time the vessels help to determine the separation between the upper division and the lingual. Divide the lung anteriorly between the stump of the upper division vein and lingular vein by placing the stapler through the utility incision while retracting the lung toward the anterior chest wall with a ring forceps placed through the posterior port. Finish the fissure between the upper division and the lingual from anterior to posterior with staplers through the utility incision.
Step 9: specimen retrieval
The left upper lobe apical trisegmentectomy is placed into an open bag for removal through the utility incision.
Comments
VATS segmentectomy is safe and feasible procedure in experienced VATS centres. The difficulty of thoracoscopic segmentectomies is mainly based on the division of the segmental plane and the distal dissection of hilar structures. Our technique is dissection of hilar structures go forward one by one from anterior to posterior. We found the procedure was performed smoothly and easily. With Harmonic scalpel dissection, blood loss is minimal and this speeds patient recovery. The technique of VATS lobectomy with Harmonic scalpel is outlined in a previously published report (2). It does not leave behind foreign materials, such as sutures or clips, and there is therefore more rapid wound healing and less chance of delayed complications.
Acknowledgements
Funding: The Fund of Application Basis Research of Yunnan Province (2010ZC216).
Disclosure: The authors declare no conflict of interest.
References
- Peng J, Chen XL, Mao X, et al. VATS segmentectomy: the First People’s Hospital of Yunnan Province, Kunming University of Science and Technology. Asvide 2014;1:363. Available online: http://www.asvide.com/articles/397
- Peng J, Chen XL, Mao X, et al. Video-assisted thoracoscopic right lower lobectomy for lung cancer using the Harmonic scalpel. J Thorac Dis 2013;5:864-7. [PubMed]