Five-year epidemiological survey of valvular heart disease: changes in morbidity, etiological spectrum and management in a cardiovascular center of Southern China
Background
Valvular heart disease (VHD) is a common condition in clinical practice that is strongly associated with heart dysfunction and death. The prevalence of VHD is 2.5% in developed countries (1). In the last three decades, the etiology of VHD has changed in parallel with socio-economic development and an increasing aging population. In developing countries, rheumatic heart disease remains the primary cause of VHD (2). Echocardiography is one of the most effective methods for the assessment of valvular structure and function, and it is widely applied for VHD screening in clinical practice. It can provide helpful information regarding the etiology of valvular disorders. The objective of the present study is to analyze the epidemiological profile of patients with abnormal valvular structure and function and highlight the etiological spectrum and management of VHD in a single cardiovascular center of Southern China.
Methods
Patient population and criteria
The present retrospective study included 19,428 consecutive patients with abnormal valvular structure and function who were screened by transthoracic echocardiography (TTE) or transesophageal echocardiography (TEE) at the in-patient department of Guangdong General Hospital between January 2009 and December 2013. Data on baseline characteristics, potential etiology, treatment strategies and discharge outcomes were collected from electronic medical records. Under standard echocardiographic criteria (3), rheumatic VHD was diagnosed on the basis of a medical history of acute rheumatic fever and/or precordial abnormalities, including the presence of a cardiac murmur. Degenerative VHD was defined according to the echocardiographic criteria for calcific valve disease, and ischemic VHD was identified based on a medical history of ischemic heart disease. Autoimmune-mediated VHD was confirmed with a medical history of autoimmune disease. Regarding infective VHD, the Duke classification allows for standardization of its diagnosis.
Statistical methods
All continuous variables were expressed as the mean ± standard deviation. Categorical variables were expressed as percentages or ratios. Patient characteristics were compared across different years using the chi-square test for categorical variables and analysis of variance (ANOVA) for continuous variables. For highly skewed variables, presented as median and first and third quartiles, the Kruskal-Wallis nonparametric test was used. Trends in the different years were assessed using the Cochran-Armitage test. A two-tailed P value <0.05 was considered to indicate statistical significance. All statistical analyses were performed using SAS for Windows version 9.2 (Cary, NC, USA).
Results
Baseline characteristics
The survey included 19,428 patients (9,441 men and 9,987 women with a mean age of 52.03±20.50 years) hospitalized in Guangdong General Hospital. Of these, 25.5% patients had atrial fibrillation (AF), 19.7% had hypertension, and 9.5% had diabetes mellitus. Baseline characteristics are summarized in Table 1. A relatively definitive etiology for VHD was identified in 13,549 (69.7%) patients by analyzing clinical data, patient characteristics and echocardiographic information. VHD was rheumatic in 7,197 (37.0%) patients, congenital in 2,697 (13.9%), degenerative in 2,241 (11.5%), ischemic in 2,460 (12.7%), infective in 611 (3.1%), and autoimmune-mediated in 138 (0.7%). The 5-year in-hospital mortality was 577 (3.0%) patients.
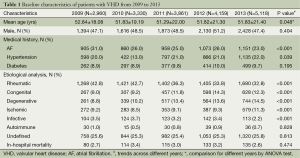
Full table
General medication was administered in 9,866 (50.8%) patients. A total of 299 (1.5%) patients underwent interventional balloon valvuloplasty. Of 9,263 (47.7%) patients who underwent cardiac valvular surgery, 472 (2.4%) received video-assisted thoracoscopic surgery (VATS) and 8,791 (45.2%) underwent classic open cardiac valvular surgery (Table 2). Coronary artery bypass graft (CABG) was performed simultaneously in 492 (2.5%) patients. The Cox maze procedure for AF ablation was performed in 947 (4.9%) patients. Tricuspid and mitral valvuloplasties were performed in 4,883 (25.1%) and 1,103 (5.7%) patients, respectively. Mitral, aortic and double valve replacements were performed in 5,331 (27.4%), 3,680 (18.9%) and 2,264 (11.7%) patients, respectively, and 5.29% of the implanted valves were bioprotheses.
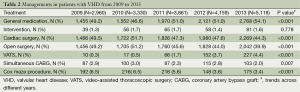
Full table
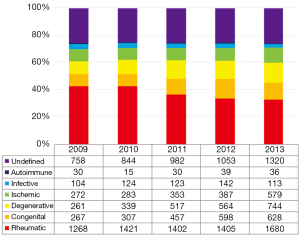
Shifts in the prevalence of different etiologies from 2009 to 2013
Further analysis of the baseline characteristics in different years revealed a shift in the distribution of etiologies for VHD from 2009 to 2013 (Figure 1), with significant decrease in the prevalence of rheumatic VHD (from 42.8% to 32.8%, P<0.001) and infective VHD (from 3.5% to 2.2%, P<0.001), and an increase in congenital VHD (from 9.0% to 12.3%, P<0.001), ischemic VHD (from 9.2% to 11.3%, P=0.003) and degenerative VHD (from 8.8% to 14.5%, P<0.001). The prevalence of autoimmune-mediated VHD remained stable from 2009 to 2013, with a slight fluctuation from 1.0% to 0.7% (P=0.158).
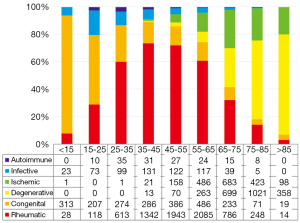
Distribution of etiologies for VHD among different age groups
Patients were divided into groups according to age, and the prevalence of each VHD type was analyzed in the different groups (Figure 2). Congenital VHD accounted for 85.8% of all patients younger than 15 years of age and its prevalence decreased with age. Degenerative and ischemic etiologies were rarely present in the <35 group. The prevalence of rheumatic VHD increased progressively before the age of 35 (from 7.7% to 73.6%), and then reached a plateau (from 71.8% to 73.6%) in the 35-45 and 45-55 groups, subsequently decreasing after the age of 55 (from 71.8% to 2.9%). The prevalence of ischemic VHD increased after the age of 45, similar to that of degenerative VHD, which increasingly predominant after the age of 65 (from 28.5% to 73.2%).
Changes in the management of VHD from 2009 to 2013
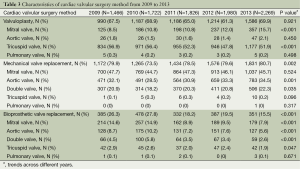
From 2009 to 2013, the proportion of patients with VHD undergoing open cardiac valvular surgery decreased (from 49.5% to 44.3%, P<0.001) and that of patients treated with general medication increased (from 49.2% to 54.1%, P<0.001). The number of patients treated by VATS increased significantly in this period (from 0.3% to 4.4%, P<0.001). As alternative methods to open cardiac valvular surgery, interventional balloon valvuloplasty and VATS were performed in patients with mild/moderate VHD. In-hospital mortality decreased progressively from 2009 to 2013. Further analysis of the methods of cardiac valvular surgery showed an increasing tendency in aortic mechanical valve replacement (from 32.1% to 34.5%, P=0.001) and double mechanical valve replacement (from 20.9% to 22.3%, P=0.035), especially in mitral valvuloplasty (MVP) (from 8.5% to 15.7%, P<0.001). However, the proportion of patients undergoing bioprosthetic valve replacement decreased from 2009 to 2013 (from 26.3% to 15.5%, P<0.001).
Discussion
Main findings
The main findings of the present study were as follows: (I) although the prevalence of rheumatic VHD decreased significantly from 2009 to 2013, it remained the leading etiology for VHD in Southern China, especially in VHD patients aged 35 to 55 years; (II) from 2009 to 2013, the prevalence of degenerative and ischemic VHD increased significantly whereas that of rheumatic VHD decreased. The prevalence of degenerative VHD increasingly predominant after the age of 65; (III) cardiac valvular surgery was the main treatment for VHD besides general medication. The proportion of patients undergoing VATS increased significantly from 2009 to 2013. Mechanical valve replacement (in particular aortic valve and double valve replacement) and mitral valvuloplasty showed a significant increasing tendency during this period.
Potential reasons for shifts in morbidity and etiological spectrum of VHD
These findings might be mainly relevant considering the socioeconomic development and improvements in quality of life, as well as an increasing aging population. In developing countries, a rheumatic etiology of VHD is prevalent (2), whereas in developed countries, degenerative VHD predominates and is found in 63% of patients (4). The prevalence of rheumatic VHD was reported at 72% in 2006-2007 in a South African center (5). In a recent survey in Turkey that included 1,300 patients hospitalized in 42 centers in 2009, rheumatic VHD accounted for 46% of all VHD patients with mean age of 57 (6). However, rheumatic VHD as second cause of VHD was present in only 22% of patients according to an European epidemiological survey (7). Risk factors for rheumatic etiology are largely associated with a sustained incidence of acute rheumatic fever and socioeconomic status, including the influence of famine, overcrowding, an unhealthy living environment, other communicable diseases, and even war (8). Due to the superior social and economic status and favorable living environment found in Guangdong compared to the rest of China, the prevalence of rheumatic VHD is decreasing progressively, although it is still present in 32.8% of patients, especially in those aged 35 to 55 years.
The surgical databases of developed countries show an increasing burden of VHD in Europe (9), the United States (10) and Canada (11), which is correlated with the predominance of an aging population and degenerative etiology. In the Euro Heart Survey, degenerative etiology was the leading cause of VHD in 63% of patients instead of rheumatic VHD (12). With the improvement of economic conditions and quality of life as well as average lifespan in Guangdong province, the prevalence of degenerative VHD increased from 8.8% in 2009 to 14.5% in 2013, and showed a marked increase after the age of 65. A similar tendency was observed in ischemic VHD, which increased from 9.2% to 11.3%, and in patients older than 45. The shift from rheumatic towards degenerative etiology accounts for the sustained prevalence of VHD and changes in patients’ characteristics; however, this shift is mainly observed in developed countries and relatively rich developing countries such as China.
Possible causes for changes in the management of VHD
VHD patients are usually elderly and often present with a high operative risk or relative/absolute contraindications for cardiac surgery, especially considering the aging population and an increasing prevalence of degenerative VHD. Therefore, most patients are ineligible for open cardiac valvular surgery. In contrast, VATS is associated with less trauma, a faster postoperative recovery and better tolerance than classic open cardiac valvular surgery. Consequently, VATS is being widely popularized in clinical practice. Currently, patients choose general medication and VATS over open cardiac valvular surgery. The baseline characteristics showed a significant shift from bioprosthetic valves to mechanical valves from 2009 to 2013. Although long-term anticoagulant treatment and elderly patients at high risk of bleeding might restrict mechanical valve implantation, increasing mechanical valves were still implanted from 2009 to 2013, especially aortic and double valves. By contrast, the limited valvular lifespan and possibility of re-operation could be associated with the decrease in bioprosthetic valve implantation from 2009 to 2013 (13). Furthermore, the high cost of repeat operations increases the economic burden for patients. In the present study, valvuloplasty mainly included the mitral and tricuspid valves, and mitral valve valvuloplasty was performed at an increasing rate from 2009 to 2013. According to the 2014 AHA/ACC guidelines for the management of patients with VHD, MVP is recommended with IIa class in asymptomatic patients with chronic severe primary mitral regurgitation with preserved left ventricular function (14). The shift of MVP is consistent with the current guidelines (Table 3).
Full table
The prevalence of valvular interventional therapy did not change significantly between 2009 and 2013. Although transcatheter aortic valve implantation (TAVI) and percutaneous edge-to-edge repair as new interventional techniques have expanded the range of valvular interventions, their application is confined to patients who are ineligible or at high risk for cardiac surgery and who were likely to be denied cardiac surgery (15,16). However, the development of interventional techniques will likely result in an expansion in the indications for valvular interventional therapy.
Limitations
The main limitation of the present study is that the findings are mostly based on a regional single center database. Therefore, regional multicenter epidemiological surveys are needed to reduce selection bias and confirm these findings.
Conclusions
Despite a significant shift from rheumatic towards degenerative etiology from 2009 to 2013, rheumatic VHD remains the leading etiology in Southern China, with a significant increase in the prevalence of ischemic, congenital and degenerative VHD. General medication and cardiac valvular surgery remain the main treatment options. The proportion of VATS increased markedly from 2009 to 2013, and mechanical valve replacement and mitral valvuloplasty showed an increasing tendency.
Acknowledgements
Funding: The article was funded by National Nature Science Foundation of China (No. 81370295), Twelfth Five-Year Plan-National Key Technology Support Program (No. 2011BAI11B13), and Science and Technology Planning Project of Guangdong Province (No. 2012B031800316, 2012B061800047, 2012B031800317).
Disclosure: The authors declare no conflict of interest.
References
- Nkomo VT, Gardin JM, Skelton TN, et al. Burden of valvular heart diseases: a population-based study. Lancet 2006;368:1005-11. [PubMed]
- Marijon E, Ou P, Celermajer DS, et al. Prevalence of rheumatic heart disease detected by echocardiographic screening. N Engl J Med 2007;357:470-6. [PubMed]
- Valvular stenosis and valvular regurgitation. In: Otto CM. eds. Textbook of Clinical Echocardiography. Philadelphia: Elsevier Saunders, 2004:281-328.
- Iung B, Baron G, Butchart EG, et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 2003;24:1231-43. [PubMed]
- Sliwa K, Carrington M, Mayosi BM, et al. Incidence and characteristics of newly diagnosed rheumatic heart disease in urban African adults: insights from the heart of Soweto study. Eur Heart J 2010;31:719-27. [PubMed]
- Demirbağ R, Sade LE, Aydın M, et al. The Turkish registry of heart valve disease. Turk Kardiyol Dern Ars 2013;41:1-10. [PubMed]
- Iung B, Vahanian A. Epidemiology of acquired valvular heart disease. Can J Cardiol 2014;30:962-70. [PubMed]
- Essop MR, Nkomo VT. Rheumatic and nonrheumatic valvular heart disease: epidemiology, management, and prevention in Africa. Circulation 2005;112:3584-91. [PubMed]
- Bridgewater B, Gummert J, Walton P, et al. eds. Fourth EACTS adult cardiac surgical database report 2010. Henly-on-Thames, UK: Dendrite Clinical Systems Ltd., 2010:2010.
- The US Society of Thoracic Surgeons National Database. Available online: http://www.sts.org/sites/default/files/documents/4thHarvestExecutiveSummary.pdf
- Hassan A, Newman AM, Gong Y, et al. Use of valve surgery in Canada. Can J Cardiol 2004;20:149-54. [PubMed]
- Iung B, Baron G, Tornos P, et al. Valvular heart disease in the community: a European experience. Curr Probl Cardiol 2007;32:609-61. [PubMed]
- Jamieson WR, Burr LH, Miyagishima RT, et al. Re-operation for bioprosthetic aortic structural failure - risk assessment. Eur J Cardiothorac Surg 2003;24:873-8. [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:e57-185. [PubMed]
- Grant SW, Devbhandari MP, Grayson AD, et al. What is the impact of providing a transcatheter aortic valve implantation service on conventional aortic valve surgical activity: patient risk factors and outcomes in the first 2 years. Heart 2010;96:1633-7. [PubMed]
- Malaisrie SC, Tuday E, Lapin B, et al. Transcatheter aortic valve implantation decreases the rate of unoperated aortic stenosis. Eur J Cardiothorac Surg 2011;40:43-8. [PubMed]


