Unidirectionally progressive resection of left upper pulmonary lobe under video-assisted thoracoscopy
Introduction
Lung cancer is the leading cause of cancer related morbidity and mortality worldwide, more than 85% of which is non-small-cell lung carcinoma (NSCLC) (1). Adenocarcinoma is a common type of NSCLC, and there are big differences among different tissue subtypes in terms of clinical features, imaging results, pathology, genetics, therapies, and prognosis. In the past two decades, video-assisted thoracic surgery (VATS) is one of the most impressive new technologies in the chest surgery area. Using this technology, there would be smaller incisions, convenient operation, and less damage. Surgeons do not have to cut off rib(s), and could open up and close the chest rapidly, and patients lose less blood during operation, experiences less post-operational incision pain, and face less risk of venous thromboembolism (2). VATS has been widely applied to wedge resection of pulmonary masses, radical cure of lung cancers, mediastinal tumor resection, radical cure of esophagus cancer, removal of esophageal leiomyoma, and many other thoracic operations. National Comprehensive Cancer Network (NCCN) recommended pulmonary lobectomy with VATS as the standard procedure of lung cancer treatment in 2006. VATS pulmonary lobectomy is usually carried out through the traditional procedure or the unidirectional procedure. In 1994, Prof. Jianxing He carried out VATS pulmonary lobectomy through the traditional procedure, which is one of the early cases of radical cure of lung cancer with VATS. In the traditional procedure, the lobe is removed in the order of fissures-pulmonary artery-pulmonary vein-bronchus, and the lobe is overturned multiple times in the operation. Comparing to traditional thoracotomy, this surgical method could better handle the pulmonary hilar vessels and pulmonary bronchus and clean the lymph nodes (3).
In this operation, we advanced in a single direction from the front to the back, and we dissociated and divided in the order of the upper left pulmonary vein, the upper left lobe bronchus, the upper left lobe arterial branches and the fissures.
Case report
The case is about a 74-year-old male. Before being admitted, a nodule in the upper left lobe was detected via chest radiographs in regular physical examination, and enhanced CT of the chest was carried out then (Figure 1). The results reveal a nodule in the upper left lobe, and there is a considerable possibility of peripheral lung cancer. Past medical history: smoking for over 40 years. After being admitted to hospital, brain MRI, general ECT bone imaging, abdominal ultrasound, and other auxiliary examinations were carried out, in which distant metastasis were not found. As the nodule in the upper left lobe is ill-defined, we decided to carry out wedge resection on the upper left lobe nodule, and intraoperative frozen section pathological diagnosis on the removed nodule confirmed well differentiated mucinous adenocarcinoma. Then we decided to carry out unidirectionally progressive resection of left upper pulmonary lobe under video-assisted thoracoscopy and mediastinal lymph node dissection. During the operation, we dissociated and divided in order the upper left pulmonary vein-upper left lobe bronchus-upper left lobe arterial branches-fissures. The pathological stage of this patient was T1bN0M0, IA.
Video descriptions
General anesthesia is adopted through double-lumen endotracheal intubation, one-lung ventilation on the contralateral, and intravenous injection. Double-lumen endotracheal intubation is essential to the VATS, and lung tissue on the operated side should be collapsed completely, or the operation could not proceed smoothly.
The patient took a 90 degree decubitus on his contralateral side.
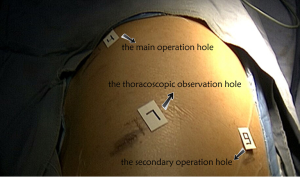
As for surgical incisions, an 1.5 cm incision is made as the thoracoscopic observation hole at the 7th intercostal space between the midaxillary line and the anterior axillary line, a second horizontal incision of 3.5 cm as the main operation hole at the 4th intercostal space between the anterior axillary line and the midclavicular line, and a third incision of 1.5 cm as the secondary operation hole at the 9th intercostal space between the axillary line and the bottom scapular line (Figure 2). The surgeons were on the ventral side of the patient, and operated with endoscope apparatus under the monitor.
Unidirectionally progressive resection under video-assisted thoracoscopy is adopted in the operation, i.e., operate right below the operation hole, and dissect the tissue to be removed from the surface. Follow a single direction to advance, and expose, dissociate, and divide in the order of upper left pulmonary vein-upper left lobe bronchus-upper left pulmonary artery and branches-fissures. Use mainly the coagulation hook to dissociate tissues, with the support of suction apparatus. Endoscopic linear cutters and hem-o-lok clip applicator are used to deal with blood vessels, bronchus, and pulmonary parenchyma
Procedure of key surgical positions:
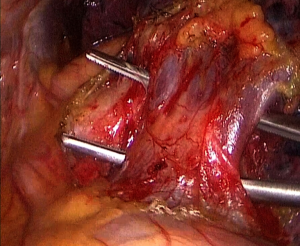
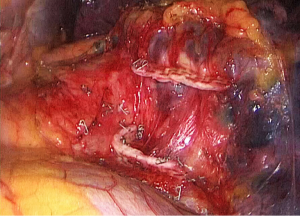
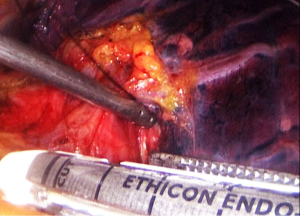
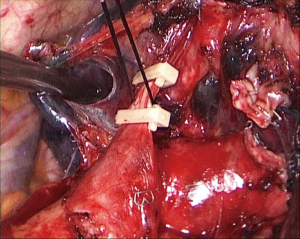
- Step 1: amputate the upper left pulmonary vein (Figures 3-5). Draw the upper left lobe rightward and outward to expose the upper left pulmonary vein, which is below the left pulmonary trunk and front of the upper left pulmonary bronchus. Dissociate and expose the upper left pulmonary vein with a coagulation hook, draw it with No. 7 silk suture, and divide it with an endoscopic linear cutter.
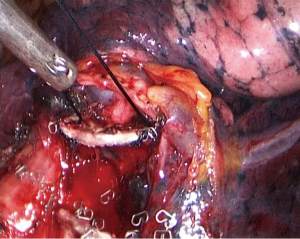
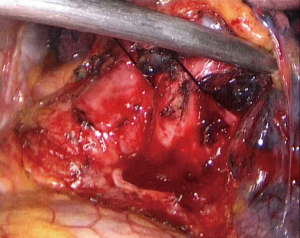
- Step 2: amputate the upper left lobe bronchus (Figure 6,7). The upper left lobe bronchus would be exposed when the upper left pulmonary vein is divided. Dissociate and divide the bronchus exposed.
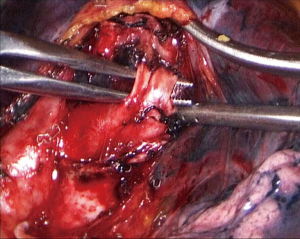
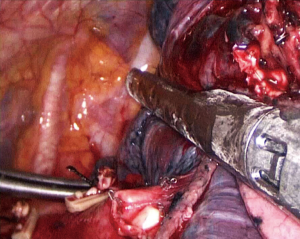
- Step 3: amputate the upper left pulmonary artery (Figure 8,10). Cut the upper left lobe bronchus and the upper left pulmonary arteries will be exposed. Dissociate the superior lingular segment and the inferior lingular segment, draw them with a No. 7 silk suture, and divide them with an endoscopic linear cutter. Then dissociate arteries in the apical segment and the apicoposterior segment of the upper left lobe in order. Use absorbable clip to close both ends of the arteries and ligate them with No. 7 silk suture before dividing.
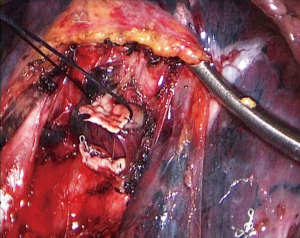
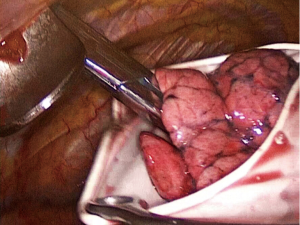
- Step 4: resect the interlobar fissure of the left pulmonary (Figure 11). Use an endoscopic linear cutter to clip the fissure tissue, and ventilate to see if the lower left lobe upswells. If yes, divide the fissure. Put the removed upper left lobe in a size 8 sterile glove and take it out (Figure 12).
Conclusions
VATS is one of the most impressive new technologies in the field of thoracic surgery and was recommended as the standard procedure for lung cancer treatment by NCCN (1). Thoracoscopic resection of lung cancer just makes small incisions, which are only 3-4 cm wide, thus avoid big cuttings into the chest flesh and damage on tissue caused by the chest opening apparatus. Comparing to the traditional thoracotomy and video assisted minithoracotomy, this approach causes less post-operative pain, and reduces the possibilities of intraoperative bleeding and postoperative complications significantly. The unidirectionally progressive resection under video-assisted thoracoscopy was first adopted by Prof. Liu et al. in China. During this resection, surgeries do not need to turn over the lobe back and forth or up and down, nor dissect the pulmonary lobe blood vessel and bronchus among underdeveloped fissures (4), so the damage to the lung tissue could be avoided even more.
From the technical perspective, resection of the left upper pulmonary lobe is considered as the most difficult pulmonary lobectomy because of the different kinds of anatomic variations of the left upper lobe artery (Figure 13). There are 4-7 branches of the left upper lobe artery generally, which may cause massive bleeding by an incorrect operation (6). By video-assisted thoracoscopy surgery, the risk of bleeding occurs when handling the pulmonary hilar vessels and bronchus could be reduced, which is the most common reason why a traditional thoracoscopic pulmonary lobectomy is changed into an opening chest operation (7).

Unidirectionally progressive resection of pulmonary lobectomy has its special incision and operating procedure which has been adopted in different pulmonary lobectomy resection successfully (8,9). We would suggest that the very kind of surgery be worth of applying in pulmonary lobectomy and other minimally invasive lung surgeries.
Acknowledgements
Funding: Sub-subject of nationally supportive subject—Research and Application of Appropriate Technology in Control and Prevention of Common Diseases in Xinjiang Autonomous Region (No. 2013BAI05B02); “Twelfth Five Year” major drug discovery projects of China (No. 2012zx09101103).
Disclosure: The authors declare no conflict of interest.
References
- NCCN clinical practice guidelines in oncology: non-small cell lung cancer. 3th edition. Fort Washington, PA: NCCN, 2014.
- Pu JT, Dai TY, Tang XJ, et al. VATS Thoracic Small Incision and Conventional Surgery for Lung Cancer: Comparison of Therapy Effect and Impact on Blood Coagulation. Chinese Modern Doctor 2010;48:5-7.
- Zhou HY, Ye X, Chen G, et al. Primary outcome of completely thoracoscopic pneumonectomy for non-smaU cell lung cancer. Chinese Journal of Thoracic and Cardiovascular Surgery 2013;29:1-3.
- Liu LX, Che WG, Pu Q, et al. Single-direction VATS lobectomy. Chinese Journal of Clinical Thoracic and Cardiovascular Surgery 2008;24:156-8.
- Cai K, Zhao H, Wu H, et al. Unidirectionally progressive resection of left upper pulmonary lobe under video-assisted thoracoscopy. Asvide 2014;1:369. Available online: http://www.asvide.com/articles/403
- Zhang GL. eds. Practical Chest Surgery. Beijing: Chinese Medical Science and Technology Press, 2007:1317.
- Sugi K, Sudoh M, Hirazawa K, et al. Intrathoracic bleeding during video-assisted thoracoscopic lobectomy and segmentectomy. Kyobu Geka 2003;56:928-31. [PubMed]
- Cai K, Ren P, Feng S, et al. Unidirectionally progressive left pneumonectomy & mediastinal lymph node dissection. J Thorac Dis 2013;5:886-91. [PubMed]
- Cai K, Wu H, Ren P, et al. Unidirectionally progressive resection of lower right lung cancer under video-assisted thoracoscopy. J Thorac Dis 2013;5:S310-4. [PubMed]