Surgical treatment of infective endocarditis in the era of minimally invasive cardiac surgery and transcatheter approach: an editorial
Infective endocarditis (IE) is a common life-threatening disease with high in-hospital mortality of nearly 20% (1). In the early stage of IE, conservative anti-infective therapy is possible. Advanced untreated IE leads to significant valve destructure. This group of patients requires timely radical surgical treatment that involves the removal of the infected valve, followed by valve prosthesis implantation. Since large floating vegetations on the valve surface have developed, emergent surgical treatment is indicated (2).
Kubota et al. recently reported a successful clinical application of the infrared coagulator “Kyo-co” for treating a patient with aortic valve IE and aortic annular abscess (3). The “Ky-co” coagulator enables the prolonged and repeated application of infrared energy to tissue in order to create deep lesions in the myocardium. The maximum temperature rise to 97.9±2.1 °C for a total of 28 sec was demonstrated, which is higher and longer compared to other available ablation systems, according to the authors. A 62-year-old male patient was operated on using the “Kyo-co.” After two large abscess orifices were identified, a careful debridement was performed. Thereafter, the infrared ablation was applied to the surrounding tissue of the abscess cavities. Then, replacement of the aortic valve using a mechanical prosthesis and of the ascending aorta (due to aneurysm) was performed. The postoperative course and the follow-up period of 5 years were without complications.
In this editorial, we discuss currently available strategies for the surgical treatment of IE. We describe different surgical options for patients with the advanced aortic and mitral valve, as well as so-called right-sided IE. Special attention is paid to the safety and feasibility of minimally invasive surgery (MIS) in the treatment of IE patients. We also reflect on the possible role of the developing transcatheter approach in the treatment of IE.
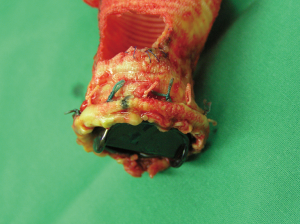
Surgical treatment of IE is associated with satisfactory early, midterm, and long-term results (4). In patients with aortic valve IE, valve replacement is often the only option. The choice of valve prosthesis is carried out according to current guidelines (5). We showed that an extensive surgical approach combined with aggressive postoperative antibiotic therapy could reduce high mortality. Sutureless aortic valve replacement was seen as an appropriate alternative for high-risk IE patients, even in degenerated bioroots, with limited postoperative morbidity and satisfied echocardiographic performance (6). In this scenario, the modified Perceval implantation technique—the so-called “snugger method”—can be applied. This technique involves the use of snuggers for proper placement of the prosthesis and eases the implantation process, thus leading to excellent outcomes (7,8). Stentless xenografts are another viable alternative for the treatment of valve/root and prosthetic endocarditis with appropriate postoperative performance and low rate of reinfection (Figure 1) (9,10).
In the case of severe annulus destruction without the possibility of valve anchoring, the new technique of off-label implantation of a sutureless valve in the mitral position has been reported (11). This technique allows a shortening of the cross-clamp time and ensures precise and safe implantation of the prosthesis in the destructured mitral ring.
MIS has been increasingly applied for IE in recent years. This approach is feasible for all common IE localizations. The aortic valve replacement for IE could be successfully performed via both upper partial sternotomy (12) and right-sided anterior minithoracotomy in the second intercostal space (13). MIS for mitral valve IE via right lateral minithoracotomy in the fourth intercostal space is also feasible and safe (14,15).
Despite the broad application of transcatheter valve interventions nowadays, this approach could not be used for IE. Treatment of IE requires a radical debridement of infected valves and surrounding tissue, which cannot be achieved due to percutaneous manipulations. On the other hand, IE after transcatheter valve implantation became a new challenge for cardiac surgeons, which can nevertheless be treated surgically and as an MIS approach (Figure 2) (13,16).

In conclusion, there are various options and equipment for the surgical treatment of IE. The new approach described by Kubota and colleagues (3), in combination with the available surgical techniques, should be helpful for further development in this field. Timely decision and careful choice of the appropriate surgical strategy combined with antimicrobial therapy are the keys to success for patients suffering from advanced IE.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: DW serves as the unpaid editorial board member of Journal of Thoracic Disease from Feb 2018 to Apr 2020. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Slipczuk L, Codolosa JN, Davila CD, et al. Infective endocarditis epidemiology over five decades: a systematic review. PLoS One 2013;8:e82665. [Crossref] [PubMed]
- Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European. Eur Heart J 2015;36:3075-128. [Crossref] [PubMed]
- Kubota H, Endo H, Ishii H, et al. An infrared coagulator to assist surgical treatment of infective endocarditis. J Thorac Dis 2019;11:4364-70. [Crossref] [PubMed]
- Farag M, Borst T, Sabashnikov A, et al. Surgery for Infective Endocarditis: Outcomes and Predictors of Mortality in 360 Consecutive Patients. Med Sci Monit 2017;23:3617-26. [Crossref] [PubMed]
- Falk V, Baumgartner H, Bax JJ, et al. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg 2017;52:616-64. [Crossref] [PubMed]
- Weymann A, Konertz J, Laule M, et al. Are Sutureless Aortic Valves Suitable for Severe High-Risk Patients Suffering from Active Infective Aortic Valve Endocarditis? Med Sci Monit 2017;23:2782-7. [Crossref] [PubMed]
- Mashhour A, Zhigalov K, Szczechowicz M, et al. Snugger method - The Oldenburg modification of perceval implantation technique. World J Cardiol 2018;10:119-22. [Crossref] [PubMed]
- Mashhour A, Zhigalov K, Mkalaluh S, et al. Outcome of a Modified Perceval Implantation Technique. Thorac Cardiovasc Surg 2019. [Epub ahead of print]. [PubMed]
- Easo J, Szczechowicz M, Hoelzl P, et al. Use of the Medtronic Freestyle for aortic valve infection: A retrospective propensity score matched analysis. J Card Surg 2019;34:957-64. [Crossref] [PubMed]
- Easo J, Weymann A, Hölzl P, et al. Hospital Results of a Single Center Database for Stentless Xenograft Use in a Full Root Technique in Over 970 Patients. Sci Rep 2019;9:4371. [Crossref] [PubMed]
- Szczechowicz M, Mashhour A, Chaduneli O, et al. Implantation of Perceval valve in mitral position: A new technique. J Thorac Cardiovasc Surg 2019;157:225-8. [Crossref] [PubMed]
- Konertz J, Zhigalov K, Weymann A, et al. Initial experience with aortic valve replacement via a minimally invasive approach: A comparison of stented, stentless and sutureless valves. Med Sci Monit 2017;23:1645-54. [Crossref] [PubMed]
- Zhigalov K, Khokhlunov M, Szczechowicz M, et al. Right Anterior Minithoracotomy for Endocarditis After Transcatheter Aortic Valve Replacement. Ann Thorac Surg 2020;109:e17-9. [Crossref] [PubMed]
- Mkalaluh S, Szczechowicz M, Dib B, et al. Early and long-term results of minimally invasive mitral valve surgery through a right mini-thoracotomy approach: a retrospective propensity-score matched analysis. PeerJ 2018;6:e4810. [Crossref] [PubMed]
- Fleißner F, Salman J, Naqizadah J, et al. Minimally Invasive Surgery in Mitral Valve Endocarditis. Thorac Cardiovasc Surg 2019;67:637-43. [Crossref] [PubMed]
- Zhigalov K, Weymann A. Rescue aortic root replacement for endocarditis after TAVR Ann Thorac Surg 2019. (Reply). [Crossref] [PubMed]