The pure distal left main bronchial sleeve resection with total lung parenchymal preservation: report of two cases and literature review
Introduction
The treatment of distal left main bronchial carcinoma usually requires a very complex surgical procedure, because of frequently involving the opening of upper and lower lobe bronchus, the vast majority of cases have to be performed sleeve lobectomy or pneumonectomy. However, under special conditions, the cases can also be strictly selected to do the pure bronchial sleeve resection with total lung parenchymal preservation (the second carina reconstruction). Compared with the right side, dependent on relationships of anatomic location, the second carina reconstruction on the left side is much more complex and difficult (1). Generally, the main indications for this surgical method include trachea-bronchial low malignant tumors (such as typical carcinoid, mucoepidermoid carcinoma and adenoid cystic carcinoma), parts of benign diseases and occasionally non-small cell lung cancer (2-4). We present the surgical results in two patients with distal left main bronchus adenoid cystic carcinoma in whom this surgical procedure were performed, and get a satisfactory therapeutic effect.
Case reports
Case 1
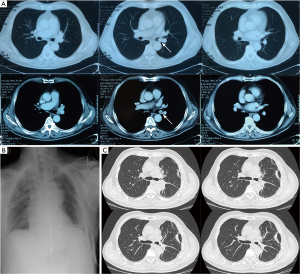
A 64-year-old man was referred to our hospital with irritating cough in September 2014. Chest CT scan showed a lesion in the terminal left main bronchus, bronchoscopy saw submucosal tumor at the end of the left main bronchus, from the carina 2.5 cm (seven cartilaginous rings), was pushed through to bronchial cavity and narrow the lumen. The opening of upper and lower lobe bronchus was observed free from involvement (Figure 1A). The diagnosis of adenoid cystic carcinoma was made on the basis of pathological findings by bronchoscopy biopsy. Surgical procedure: we used posterolateral incision through the 5th intercostal chest, breaking the 5th rib and free intercostal muscle pedicle flap. In the operative view, we first release the hilar dissect mediastinal and hilar lymph nodes. Then we fully free pulmonary vein and pulmonary artery, respectively, setting on a leash, and totally release the left main bronchus and lobar bronchus. When removing the truncus intermedius, intraoperative frozen pathological examination of tumor proximal, distal transection of the left main bronchus, and lobe bronchus showed negative. Surgical reconstruction of the second carina was performed on continuous suture upper and lower lobe bronchus side-to-side like ‘B’ type, and then make the left main bronchus anastomosis end-to-end with 3-0 Prolene. Intercostal muscle pedicle flap was surrounded the anastomosis and suture fixation at last (Figure 1B,C). Since the results of a final pathological examination showed the upper lober margin was positive, the postoperative adjuvant radiotherapy was performed 6 weeks later.
Case 2
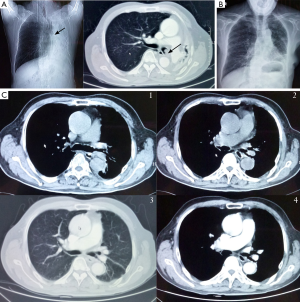
A 67-year-old man was admitted to our hospital in July 2012 complaining of hemosputum and chest pain. The patient accepted intravenous chemotherapy 4 times with paclitaxel and cisplatin before treatment in our clinic, and without any improvement in symptoms. Chest CT scan showed an intraluminal mass at the left main bronchus, the whole left lung was atelectasis (Figure 2A). Endobronchoscopy examination showed a papillary neoplasm bulge at the middle left main bronchial cavity in about 1 cm diameter, completely blocking the lumen. Biopsy revealed low-grade malignancy, tendency to adenoid cystic carcinoma. The basic surgical procedures in this patient were same as the first case, and the two-step anastomosis was performed between the left main bronchus and the ends of the left upper and lower bronchi, using 3-0 Vicryl sutured. The anastomosis was wrapped with the intercostal muscle pedicle flap at last. The unique procedure was that we had repeated lung lavage several times before anastomosis was performed, in order to identify the lung parenchymal was not infringed by lung abscesses and could be recruited during ventilation. The postoperative follow-up was over 2 years without recurrence of the tumor (Figure 2B,C).
Discussion
Pure bronchial sleeve resection and reconstruction is a type of rare thoracic surgery, especially for the second carina reconstruction on the left side, needs more exquisite surgical techniques, and patient selection to such surgery often requires rigorous screening.
Surgical indications and selection of cases
According to the literature, the same as other trachea-bronchial surgery, the indications of the pure distal main bronchial sleeve resection are the following three diseases: bronchial benign diseases (including bronchial luminal stenosis caused by inflammation, trauma and benign bronchial lesion), bronchial low-grade malignant tumor (including typical carcinoid, mucoepidermoid carcinoma and adenoid cystic carcinoma) and rare non-small cell lung cancer (1,4-6).
For bronchial stenosis caused by tuberculosis infections, whether the infection is in the active stage must be identified prior to surgery (7). The current view is that patients with active tuberculosis infection must accept anti-tuberculosis therapy for more than 6 months before surgery, and need to exclude the damage of lung parenchyma. For the rare cases of bronchial benign lesion, the growing maturity of endobronchial treatment techniques can usually replace surgery with much more invasive (8-10).
Recently, a tracheobronchial plasty mainly uses for low-grade malignant tumor. Such tumors originate in the tracheobronchial epithelium or glands, often limit in the tracheobronchial lumen, and grow slowly, few lymph node metastasis and distant metastasis are happened. Our two cases of the second carina reconstruction on the left side were both distal left main bronchial adenoid cystic carcinoma. There are literatures show that, compared to typical carcinoid and mucoepidermoid carcinoma, adenoid cystic carcinoma often grows along with submucosal, even further involves tracheal rings and violates surrounding tissues and organs outside the tracheal lumen (11). So with the highest degree of malignancy, the 5-year survival rate of ACC is only about 73% (12). The recurrence rate of endobronchial therapies is higher than 1/3 because of cartilage ring and surrounding tissue involvement. Surgical treatment can resect the tumor radically (R0 resection) and obtain a satisfactory therapeutic effect. It has been reported that even the positive bronchial margin (R1 resection), the patient can also get a long survival (13).
And pure bronchial resection is used pretty rare in the treatment of patients with non-small cell lung cancer. Previous literature points out that it must be confined to the exclusion of lung parenchyma involvement, and preoperative pathological diagnosis is required to identify no lung and mediastinal lymph node metastasis (14).
The points and difficulties of surgical techniques
Compared to the right bronchial sleeve resection, the second carina reconstruction on the left side is much more complex and difficulties. First of all, because of the aortic arch and thoracic aorta around the hilum, the relative positions are deeper when not only free of the left main bronchus and pulmonary artery, but also the reconstruction process of stitching. It has to be released more to expose enough anastomosis space, sometimes even need to free and suspend low trachea to lift stitching position. Secondly, compared to the right bronchus located at the rear side of the pulmonary artery, left pulmonary artery is through the top of the left main bronchus, across the rear of left upper lobe bronchus and traveling in the rear side of the lower lobe bronchus, the formation of ‘pulmonary arch’. So when reconstructing the second carina on the left side, the anastomosis of upper-lower lobe bronchus and the left main bronchus is often hidden in the rear of the left pulmonary artery. Surgeons need to be fully free and hanging the pulmonary artery in order to successfully completing this operation. In addition, because the left main bronchus resectable length is often longer than the right side, it sometimes needs to release the hilum and even open the pericardium to avoid anastomotic tension.
Discussion of lymph node dissection (skeletonized or not)
Classic points of tracheal surgery believe the best free length for trachea-bronchial should be controlled within a distance 0.5 cm from the margin in order to avoiding weak anastomotic blood supply. But in the light of oncological surgery, we need systematic dissection of lymph nodes around bronchus, and make it ‘skeletonized’. This is a contradiction. Our view is that, it should be possible to dissect the bronchial lymph node, one in favor of radical resection of the tumor, on the other hand it can help to bronchial completely release, more fully expose the surgical field. For the worry of anastomotic blood supply, we used to retain the intercostal muscle pedicle flap and surround the bronchial anastomosis to reduce tension while also promote the growth of new blood vessels to reduce bronchial fistula occurrence. In fact, the above two cases of patients were treated with this method and did not meet bronchial fistula caused by anastomotic poor blood supply.
Preoperative evaluation and intraoperative treatment of atelectasis
We concerned that in the treatment of the second patient, the preoperative examination revealed full atelectasis of left lung. Such cases require the surgeon more adequate preoperative preparation and evaluation. Patients in the preoperative diagnosis are often difficult due to atelectasis full ventilatory defect formed after bronchial obstruction, or because of lung destruction caused by chronic inflammation of the lung. So those who plan to do the procedure need the preparation of lobectomy or pneumonectomy, while operation must clean out bronchial secretions to confirm the lung whether to recruitment or not. When we performed the pure bronchial resection, we repeated lung lavage several times and confirmed that no purulent discharge flowing out from distal lung tissue and totally recruitment the lung before reconstruction. The surgeon must not blindly reserved distal lung tissue, while ignoring the possibility of lung destruction.
Conclusions
Pure bronchial sleeve resection is better to protect lung function, and is a useful supplement to conventional surgery for some selected patients, but it can not replace the sleeve lobectomy and pneumonectomy. The second carina reconstruction needs for strict screening and preoperative evaluation of patients and also depend on higher requirements on the surgeon’s surgical techniques.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Ragusa M, Vannucci J, Cagini L, et al. Left main bronchus resection and reconstruction. A single institution experience. J Cardiothorac Surg 2012;7:29. [PubMed]
- Bagan P, Le Pimpec-Barthes F, Badia A, et al. Bronchial sleeve resections: lung function resurrecting procedure. Eur J Cardiothorac Surg 2008;34:484-7. [PubMed]
- Cerfolio RJ, Deschamps C, Allen MS, et al. Mainstem bronchial sleeve resection with pulmonary preservation. Ann Thorac Surg 1996;61:1458-62; discussion 1462-3. [PubMed]
- Bölükbas S, Schirren J. Parenchyma-sparing bronchial sleeve resections in trauma, benign and malign diseases. Thorac Cardiovasc Surg 2010;58:32-7. [PubMed]
- Frist WH, Mathisen DJ, Hilgenberg AD, et al. Bronchial sleeve resection with and without pulmonary resection. J Thorac Cardiovasc Surg 1987;93:350-7. [PubMed]
- Jiang X, Dong X, Zhao X, et al. Bronchial sleeve resection distal to the main bronchus with complete pulmonary preservation for benign or low-grade malignant tumors. Ann Thorac Surg 2007;84:e19-21. [PubMed]
- Lei Y, Tian-Hui Z, Ming H, et al. Analysis of the surgical treatment of endobronchial tuberculosis (EBTB). Surg Today 2014;44:1434-7. [PubMed]
- Dambara T. Endoscopic laser treatment of mucous gland adenoma arising in the trachea. Intern Med 1996;35:841. [PubMed]
- Aggarwal A, Tewari S, Mehta AC. Successful management of adenoid cystic carcinoma of the trachea by laser and irradiation. Chest 1999;116:269-70. [PubMed]
- Díaz-Jiménez JP, Canela-Cardona M, Maestre-Alcacer J. Nd:YAG laser photoresection of low-grade malignant tumors of the tracheobronchial tree. Chest 1990;97:920-2. [PubMed]
- Kanematsu T, Yohena T, Uehara T, et al. Treatment outcome of resected and nonresected primary adenoid cystic carcinoma of the lung. Ann Thorac Cardiovasc Surg 2002;8:74-7. [PubMed]
- Regnard JF, Fourquier P, Levasseur P. Results and prognostic factors in resections of primary tracheal tumors: a multicenter retrospective study. The French Society of Cardiovascular Surgery. J Thorac Cardiovasc Surg 1996;111:808-13. [PubMed]
- Maziak DE, Todd TR, Keshavjee SH, et al. Adenoid cystic carcinoma of the airway: thirty-two-year experience. J Thorac Cardiovasc Surg 1996;112:1522-31; discussion 1531-2. [PubMed]
- Ohta Y, Yachi T, Oda M, et al. Bronchial sleeve resection with complete preservation of the lung for carcinoma. Respiration 2001;68:528-32. [PubMed]


