Impact of tobacco control interventions on smoking initiation, cessation, and prevalence: a systematic review
Introduction
Tobacco smoking is one of the leading causes of preventable death, killing more than 8 million people a year worldwide. Currently, more than 1 billion people smoke, with over 80% living in low- and middle-income countries (1). Although tobacco control has been recognized as a top target for public health, tobacco use still remains the single largest preventable cause of disease and premature death. Every year, cigarette smoking results in estimated 443,000 premature deaths, of which about 49,400 occur in non-smokers due to the exposure to secondhand smoke (SHS) (2). Over the past 5 years, much progress has been made in reducing tobacco use in Europe and USA through effective tobacco control policies.
The Framework Convention on Tobacco Control (FCTC) is a supranational agreement that seeks to protect present and future generations from the devastating health, social, environmental and economic consequences of tobacco consumption and exposure to tobacco smoke, by enacting a set of universal standards stating the dangers of tobacco and limiting its use in all forms worldwide (3). For this purpose, the treaty’s provisions include rules that govern the production, sale, distribution, advertisement, and taxation of tobacco. However, full implementation of the treaty and most of its obligations still remain poor (4).
The implementation of the tobacco control activity in 53 countries in the WHO European Region countries has been analyzed (5). The assessment provided a mixed picture and a low implementation rate was observed for several indicators: 25 countries have increased tobacco taxes, only 14 countries have laws on smoke-free public places, only 7 countries have ban advertising, promotion and sponsorship. This highlights both the difficulty of putting international agreements into place and practice, and perhaps the pressure from the tobacco lobby to delay and postpone effective measures of tobacco control. In addiction the countries of Africa Region, where there is a tobacco epidemic for several reasons, including lack of funding to implement prevention measures, represent a cause of concern (1).
Among the proven policy interventions, the most used tobacco-control measure is to increase excise taxes on tobacco products. While the governments raise taxes, tobacco companies generally raise prices to preserve their profits, and the higher prices deter consumption. Notably, consumption decreases more in young and lower-income people, thereby potentially protecting more vulnerable groups (5). Other non-price tobacco control policies have been conducted, such as the smoking ban in the workplace, as well as spaces where people live, eat, and engage in recreational activities, with the aim to preserve also non-smokers’ health. Furthermore, to improve the knowledge, attitudes and behavior of a large proportion of the adult and young people, numerous projects have been implemented through the mass media and in the school context, as a means of delivery preventive health messages, mainly to limit the initiation and to promote the smoking cessation.
In 2013 the European Commission (6) has proposed new directives about labeling and packaging of tobacco products by introducing warning text with pictorial warning that occupies 75% of the cigarette packages. Subsequently, an increasing number of countries (France, the UK, New Zealand and Norway) have emulated Australia by legislating that tobacco products can only be in plain, standardized packs, without logos and colors, thus diminishing the appeal to consumers, including the young people (7).
In order to clarify the benefits of intervention programs and the most effective methods in Europe and USA, in this review we have analyzed the effects of tobacco control policies on smoking initiation, considering that the age of onset of tobacco use is an important predictor of life-time tobacco use. An individual who starts smoking at an early age has a higher probability of a long-term tobacco addiction (8). Also, the age of smoking cessation is very important, since Pirie et al. (9) have shown that quitting smoking before the age of 40 avoids more than 90% of the excess mortality.
In this study we present recent programmes which have contributed at supporting the tobacco control policies. The review is based on the findings of published systematic reviews, other reviews and studies available in the main search engines. To organize the wealth of information on the topic of tobacco prevention and control efforts among adults and youth, we categorized efforts into the following areas: tobacco excise taxes; tobacco control on young people; public education through mass media campaigns; introduction of smoke-free indoor environments; the recent entry in the market of electronic nicotine delivery systems (ENDS/e-cigarettes) and new heated tobacco products [heat-not-burn (HnB)] and their possible related impact on smoking cessation.
Study design and scope
We have analyzed the main smoking-prevention/cessation activities and their effectiveness, achieved in Switzerland, Europe, UK, USA, South America, New Zealand and Australia. The articles published between 2014 and 2019 and including a large sample size have been selected by using the search terms: anti-smoking advertising intervention, anti-smoking mass media intervention, tobacco intervention programme, e-cigarette and HnB tobacco products. The main sources were PubMed, EBSCOhost and Cochrane Library database. Only English-written peer-reviewed articles were considered.
We have categorized the following areas: (I) tobacco excise taxes; (II) tobacco control on young people; (III) mass media campaigns; (IV) smoke-free indoor environments; (V) the role of ENDS and HnB as possible tools helping smoke cessation.
Data extraction
Between October 1st, 2019 and December 1st, 2019, the data were extracted on the basis of study design, setting, sample size and characteristics, study length, type of intervention, and measures of effectiveness, by using the keywords described above. A formal meta-analysis of the literature was not feasible because of the differences in study population, study design and outcome measures. Hence, we used a qualitative systematic review.
Results
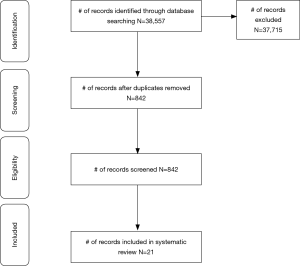
The initial search on electronic databases produced 38,557 references (Figure 1). After removing duplicates, articles not written in English, and published before 2014, 842 references were screened and analyzed by two reviewers.
Of the 842 full-text articles assessed for eligibility, 21 papers met the inclusion criteria for this review: 5 regarding tobacco excise taxes and prices; 6 studies related to tobacco control on young people; 2 about mass media intervention; 4 related to smoke-free indoor environments; 4 studies related to the role of ENDS and HnB.
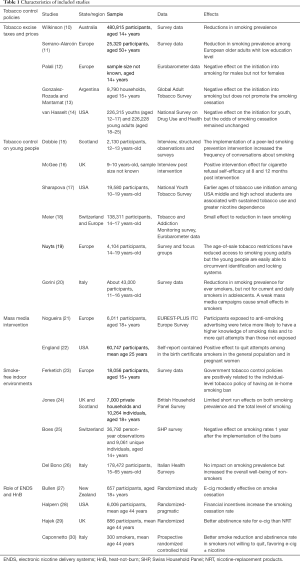
The design and results of main published studies are summarized in Table 1.
Full table
Does tobacco taxation continue to be a useful tobacco control policy on smoking initiation and cessation?
To raise excise taxes on tobacco is one of the measures to control and reduce tobacco demand suggested by the WHO in the context of the FCTC. The longitudinal studies have found high strength of evidence to quantify the impact of increase in tobacco pricing (31-35). Wilkinson and Coll. (10) have demonstrated that tobacco tax increasing prompted immediate drops in smoking prevalence, as well as ongoing reductions in smoking prevalence. These findings occurred in Australia, a country that already had high tobacco prices due to pre-existing taxes. Recent European studies also have confirmed that raising tobacco taxes and smoke-free policies are significantly related with a reduction in smoking among young and older adults and among those with lower education (11). Palali et al. highlighted that, even though real prices of tobacco have been increasing over time in Europeans countries, the increase is much steeper in countries such as Finland and UK than in other countries (12).
However, Gonzalez-Rozada and Montamat (13) examined the role of tobacco prices on smoking onset and quitting by using data from the Global Adult Tobacco Survey (36), so reporting that an increase of 10% in real cigarette prices is expected to delay smoking onset by almost 2.5 years. On the other hand, the same policy is less effective to reduce the duration of the habit because there is no meaningful relationship between the duration of the smoking habit and the actual price of cigarettes. The policy of raising cigarette excise taxes in order to increment prices seems to be more effective to delay smoking onset; conversely, the same policy is less effective to reduce the duration of the habit. In fact, several studies reported that raising cigarette prices by increased taxes is a highly effective measure to reduce smoking among youth, young adults, and people with low socio-economic status. However, there is a striking lack of evidence about the impact of increasing cigarette prices on smoking behavior in heavy/long-term smokers (37). In general, the available literature data have shown that the odds of smoking initiation decrease for youth after the tax increase but the odds of smoking cessation remain unchanged (14).
Therefore, a policy recommendation emerging from this evidence is that, for people with a developed addiction, a combination of increasing taxes and other public health policies, like cessation therapies, could be more necessary and effective.
What are the most effective tobacco prevention strategies in young people?
While the tobacco control policies have focused mainly on tobacco excise taxes, product advertising bans, and indoor/outdoor smoking bans, less attention has been paid to school tobacco control programmes and their impact on youth smoking behavior (38). Teenagers are generally more susceptible to social influences, such as peer pressure, experimentation and rebellion. These social influences are associated with a greater tendency to undertake in risk-taking behavior, such as drug taking or risky alcohol consumption, and can play a crucial role by influencing long-term health outcomes (39). Thus, the years of school attendance represent key period to implement interventions aimed to deter uptake of unhealthy behaviors.
In this report we illustrate some recent school programmes that have shown to be effective.
A Stop Smoking in Schools Trial (ASSIST) is a school-based, peer-led smoking prevention programme that encourages the diffusion of non-smoking norms among secondary school students (aged 12–13) (15). In this intervention some students (aged 12–13) were recruited as “peer supporters” and received intensive training by professional health promotion staff. The peer supporters were trained to act with their peers in everyday situations to discourage smoking. ASSIST is also an example of programme that favors the peer communication about the risks of smoking, by involving schools and spreading information on smoking harms through social networks. The results of this programme suggest that young people feel peer-led health promotion as acceptable and credible.
Other interesting programmes have promoted correct lifestyles (sports, nutrition) as cigarette antagonists (16), also in primary school. The results showed short-term positive effects on smoking attitudes among children, and cigarette refusal self-efficacy among girls.
The most recent trend is to carry out activities based on cognitive information and social skills, in particular, to teach young people the resistance skill to say “no”, to manage peer pressure and influences, that have been identified as important predictors for starting smoking. For example, since 2002 the European Commission within the Community Programme for the prevention of drug dependence implemented the “UNPLUGGED project” (for students between the ages of 12 and 14) (40). A short-term follow-up showed that the programme could reduce the use of tobacco, drugs, and intoxication drinking by 25–30% as compared to the expected trends. These results are encouraging, especially considering the high prevalence rates of tobacco use among Czech adolescents (in 2016, more than one half of students: 55.6%) (41).
It is noteworthy that the most effective prevention activities are aimed at promoting social skills especially in younger people. van Ours (8) reported that the age of onset of tobacco use is an important predictor of life-time tobacco use. Also, Sharapova et al. (17) showed that earlier tobacco use initiation among USA middle and high school students correlates with protracted tobacco use and stronger nicotine addiction.
Meier et al. (18) investigated the effects of the ban on the sales of tobacco to teens in Switzerland and in the European Union, showing less than 1% point reduction in teen smoking, below the projected objective, probably because teens can circumvent the restrictions by getting cigarettes from other sources, such as their peers, instead of from stores (18).
Finally, to contrast the sales of cigarettes to minors, the cigarettes sales by retailers to individuals under age 18 have been prohibited by law in the majority of countries. Enforcement actions should involve compliance checks, penalties, publicity, and bans on self-service displays or vending machines. Overall, the available data provide little evidence that youth access policies are effective in terms of reducing smoking prevalence; indeed, an Italian study observed an increase in daily smokers between 15 and 16 years old (19,20).
It is important to implement prevention and information to children about cigarette smoking when they are still young and particularly receptive and able to set behaviors and approaches that persist into adulthood.
Do mass media campaigns and anti-smoking advertising impact on initiation, cessation, and prevalence of smokers?
The FCTC requires to promote and strengthen education and public awareness of the tobacco harms. Among the anti-smoking mass media campaigns directed to large audiences with anti-smoking messaging via outdoor channels, such as billboards and posters, printed media like newspapers and magazines, social media and the internet, the most commonly used channels are television and radio. In these platforms, the message is communicated more quickly and efficiently to wide audiences during a defined period, with relatively low cost per person.
Nogueira et al. (21), through EUREST-PLUS project, showed that in Europe mass media campaigns are differently implemented. By comparing the anti-smoking advertising in six European countries, this study evidenced that the exposure to anti-smoking advertising is related to knowledge of smoking health risks and quit attempts, with consideration of socio demographic variables (country, sex, age, education, household income, level of urbanization, and smoking status). A high proportion of participants reported being exposed to anti-smoking advertising mostly by television. Young adults and those with higher education levels had significantly higher exposition to anti-smoking advertising on the internet and social media than older people and those with lower education level. No association was found by sex, income, and urbanization. These project findings confirm that there is an association between high exposure to mass media anti-smoking campaigns and increased knowledge of smoking health harms.
The association between high exposure to mass media anti-smoking campaigns and increased knowledge of smoke-related harms is evident, provided that these campaigns are prolonged over time.
A recent study (22) investigated the specific impact of the TIPS campaign (aired for 12 weeks in USA that reached about 80% of cigarette smokers) on pregnant smokers. It emerged that the exposure to this national anti-smoking campaign for a general audience was correlated with smoking cessation in pregnant women. Cessation rates were statistically significantly higher in exposed versus unexposed women for almost all subpopulations examined. This result highlights the need to study and create specific anti-smoking advertisements for subgroups of subjects instead of targeting the general population.
In Italy the tobacco control policies by mass media campaigns are weak, so over the past 20 years the rate of ever smokers slightly reduced, but did not decrease the rate of current smokers in the age group between 15–16 years, underscoring the need for stronger tobacco control measures in adolescents (20). The authors pointed out that in Italy the price of tobacco is substantially lower than in other European countries (although some proposals for price increases have been made); no reduction in tobacco sales of stores or vending machines has been reported after the introduction in 2013 of tighter rules on youth tobacco access. The authors conclude that, in this scenario, stronger tobacco control measures are urgently needed to determine a steeper decline in smoking prevalence in adults and adolescents, such as drastic rise in tobacco taxes, as well as well-designed mass media anti-tobacco campaigns, that are lacking since many years, and finally the introduction of plain package, which demonstrated positive results even in closer countries, such as France.
Do smoking ban in public places influence on initiation, cessation, and prevalence of smokers?
The smoking ban in public places represents a recent remarkable high-profile public health intervention. Currently, 17 European countries have comprehensive smoke-free laws in place. Among these, Italy, Ireland, the UK, Greece, Bulgaria, Malta, Spain and Hungary have the highest smoke-free provisions with a complete ban on smoking in closed public places, on public transport and in workplaces, with only limited exceptions. Despite the primary aim of these bans was to protect nonsmokers from SHS, another aim of this prevention measure was to reduce the consumption of cigarettes and encourage to quit smoking. A recent study evaluated national tobacco control policies regarding the choice not to smoke even at home (23). A higher rate of complete in-home smoking ban has been reported in the western European countries (>80% in Finland and Sweden), as compared with the eastern European countries (<50% Croatia, Greece, Bulgaria and Poland). In addition, among 16 European Union Member States, strong national-level, comprehensive tobacco control policies, measured by the Tobacco Control Scale, were correlated to higher rate of voluntary in-home smoking bans. Whereas some studies have found a reduction in tobacco consumption due to smoke-free laws, other reports didn’t show substantial changes. In Spain, the introduction of smoke-free laws reduced by 2% the proportion of households containing smokers although did not cause reductions in households’ expenditures on restaurant services or on bars and cafeteria services (42).
Jones et al. (24) evaluated the impact of smoking bans on active smoking from the British Household Panel Survey, showing limited short-run effects on both smoking prevalence and the total level of smoking, indicating that the smoking ban didn’t have significant impact on smoking prevalence in Scotland and England.
In Switzerland the bans were introduced in different regions at different times; Boes et al. (25), by using a difference-in-difference approach, have found a reduction of smoking rates but only 1 year after the bans implementation. According to the authors’ opinion, this lag could reflect the time needed to modify addictive behavior such as smoking and suggest minimal net welfare change attributable to smoking bans in Switzerland.
A recent article has investigated the impact of the public smoking ban, implemented in 2005 in Italy, on tobacco control and individual well-being. In this study, by adopting a difference-in-difference approach (that is a method to estimate causal effects of interventions), the Authors showed that the smoking bans only had an impact on some subgroups of smokers (single, low-educated, young), but improved the overall well-being of non-smokers (26). Also, this research showed that the previous studies, focusing on a before-after comparison, could have overestimated the effects of the ban.
Is there a role for new products (ENDS, HnB) in smoking cessation programmes?
ENDS and HnB products have been marketed and presented as healthier than traditional cigarettes; these new products have been also proposed as tools helping smokers to quit (43,44).
In the last few years, several studies have investigated about the ENDS use as a help to quit smoking. Although the ENDS use is associated with increased rates of attempting to stop smoking and reducing smoking, the reports are not homogeneous and the results are controversial, so the issue is still debated (27,28,45-53). A web-based survey conducted in Great Britain by Brose and Coll. (47) showed that the daily use of e-cigarettes while smoking appears to be associated with subsequent increases in rates of attempting to stop smoking and reducing smoking, but not with smoking cessation. In addition, data about long-term safety of ENDS are lacking (50,51,54-56).
In the randomized study by Bullen and Coll. (27), the abstinence rate was higher for e-cigarettes containing nicotine as compared with nicotine patches and placebo e-cigarettes.
Similarly, in the Cochrane review published in 2016 by Hartmann-Boyce and Coll., e-cigarettes with nicotine have shown better efficacy for long-term smoke cessation than nicotine-free e-cigarettes (56).
Recently, the American College of Preventive Medicine’s Practice Statement by Livingston and Coll. (57) included seven systematic reviews (56,58-63), with only limited evidence supporting the short-term efficacy of exclusive use of nicotine-containing ENDS in some randomized clinical trials (RCTs) as compared with observational studies. Also considering the heterogeneity of study arms, the efficacy of ENDS with respect to established evidence-based treatments is not yet clearly demonstrated.
A recent randomized trial added important data about the use of ENDS as possible aid to smoke cessation as compared to nicotine-replacement products (NRT); the study, conducted in UK on 886 subjects and with the expert guidance on the free choice of the fully available NRT, showed that e-cigarettes are more useful for smoke cessation than NRT. The 1-year abstinence rate was 18% and 9.9%, respectively, favoring the e-cigarette group [relative risk (RR): 1.83, 95% CI: 1.30 to 2.58; P<0.001] (29).
The stronger efficacy, almost twice as effective tool in helping smokers to quit, especially in comparison with previous studies (27,28,30), has been attributed to multiple factors, including the behavioral support for both subgroups, the use of refillable devices generally more efficient to nicotine delivery, and the population of subjects highly motivated to quit smoking.
As previously reported (27), the TEC study by Hajek and Coll. has confirmed the better control of tobacco withdrawal symptoms by e-cigarettes, as compared to NRT; furthermore, the rate of mouth and throat irritation and nausea, more frequent in e-cigarettes group and NRT group, respectively, was described (29).
A remarkable characteristic of this study is to focus on the behavioral support that seem to be crucial in this setting; in fact, as compared with the widely approved NRT, e-cigarettes seem to be more useful only if associated to behavioral interventions; this topic needs to be further investigated especially aiming to plan interventions in the future smoking cessation policies, better focusing public health messages about counseling cessation programs (29).
Despite the interest and the potential application in real world interventions of the results deriving by this trial, some critical issues remain unresolved, mainly about the largely unknown long-term health risk of ENDS and the well-known brain damages by nicotine as well as its carcinogen effect (64); moreover, further studies have to address also how to select the subjects according to the previous quit attempts by traditional available NRT and convinced motivation to quit, as well as the optimal duration of treatments to compare, as highlighted by Zhang (65).
The dual use in a not negligible rate of subjects in the TEC trial (29) has been also underscored as a meaningful health issue by Stein (66), due to the lack of information about this matter.
Among e-cigarette users, a large proportion wish to stop smoking or reduce the smoke-related harms (47,67); nevertheless, a subgroup of them continue to smoke cigarettes as “dual” use.
These subjects are characterized by the high number of failed quitting attempts, therefore by a particular resistance to smoking cessation programs (68).
A recent experience (69) explored the dual users’ interest in stop-smoking treatment by medications such as varenicline, and its impact on smoking and vaping behavior as well as on nicotine intake. Despite the study was not randomized, the findings suggest that varenicline offered to dual users is likely to promote successful abstinence from both smoking and vaping.
Finally, Selya and Coll. (70) have highlighted also a very important topic, regarding the need to accurately assess the amount of nicotine dependence when planning interventions using e-cigarettes as cessation tool, due to the possibly different contribution of nicotine’s dependence to the e-cigarettes effectiveness in this setting.
In HnB products, unlike conventional cigarettes, the tobacco is heated at lower temperatures (350 °C compared to over 600 °C), so these products have been marketed as “at lower-risk” due to the expected lower exposition to toxics and carcinogens.
However, this characteristic of least harmful potential has not been definitively ascertained; a growing number of studies in the last few years have evidenced toxic effects on epithelium and smooth muscle cells of airway, including oxidative stress and release of cytokines (71).
Although inferior to traditional cigarettes, HnB products emit high levels of carbonyls, free radicals, aldehydes and other substances deserving further investigations (72-76), so playing a possible role in the smoke-related respiratory diseases including cancer (77).
The data about these harms are already partially available, but still not enough about the effects deriving from long-term exposure or dual use of HnB plus traditional cigarettes, due to the risk of increased nicotine assumption, likely with already happened with e-cigarettes (78,79).
About the relationship between HnB products and smoke addiction, it is noteworthy that a large part of non-smokers and young people acquire a smoke addiction through these new products (80); the use of these products with the aim of smoking cessation is still very controversial especially outside of dedicated and medical-assisted programs.
The nicotine intake of HnB and cigarettes is comparable, meeting the need of nicotine during the cessation programs of smokers, but keeping the physical dependence unchanged, although by reducing the harms related to the exposure to the combustion compounds (81); however, although the smoking modalities with these devices seem to reduce the desire for the traditional cigarettes, there is a lack of long-term studies assessing the efficacy of these devices in the cessation programs.
Conclusions
The main reason why tobacco products remain very popular is the aggressive marketing by tobacco industry. Tobacco brands seek to present products that convey glamour, coolness, and success. The health community and government authorities should strongly fight smoking and protecting non-smokers because smoking shortens smokers’ lives by about 12 years in males and by about 11 years in females; furthermore, over half of smokers die from a tobacco-related disease (82). In addition to tobacco price policies, many countries have introduced non-price tobacco control policies to reduce smoking, with contradictory results partially due to differences in methodology, making it challenging to attribute the effects on smoking incidence to a decrease in the uptake of smoking or an increase in quitting smoking (12). Our review tries to contribute to the knowledge about the correlation between tobacco control policies and smoking initiation and cessation. We have analyzed the overall impact of tobacco control policies and the separate components of these policies: tobacco excise taxes, tobacco control on young people; mass media campaigns and smoke-free indoor environments.
The analysis of published articles clearly shows that there is not a single instrument useful to contrast and reduce smoking prevalence, mainly by preventing smoking initiation.
The tobacco control strategies should act differently at different levels and on specific target groups (for example young people or pregnant women). In particular, the programmes against the initiation of smoking should be aimed at young people in the classrooms principally by methods to increase self-efficacy and resistance skills to deny cigarette offers. Recent studies highlighted the importance of acting during pre-adolescence (83), as the interactions among peers mostly influence the lifelong learning habits of students. It would be helpful to invest the money of tobacco excise taxes in awareness raising, informing and prevention, in a consistent manner, in all countries. For instance, incentives could be introduced for the creation of antismoking centers, the group behavior therapy, and to support the purchase of drugs and nicotine replacement therapy, so improving the anti-tobacco policies.
The policy focused on the mass media seems less effective on young people while favoring the cessation of adult smokers. Overall, the prohibitions, although not clearly favoring the smoking cessation or the reduction in prevalence, could: (I) protect non-smokers from passive smoking, (II) denormalize the cigarette consumption, (III) make smoking a less acceptable behavior while promoting a cultural change.
Moreover, regarding to ENDS and HnB as possible tools helping smoke cessation, although the current e-cigarette users should be counseled towards complete cessation of cigarettes and e-cigarettes, some data support a possible role of e-cigarettes on smoking cessation, albeit by engaging smokers in a quit attempt (84). Further investigation is ongoing and is needed mainly about the optimal selection of subjects, the study designs and cessation modalities, as well as the impact of HnB products in this scenario.
Many aspects still need to be considered in order to understand the efficacy of policies including the culture of belonging, the pressures of the tobacco multinationals, the socio-economic level of the countries. In conclusion, we have summarized the main areas of tobacco prevention and control although it remains difficult to determine which one, among tobacco control measures, will be most effective on smoking cessation or to reduce prevalence and initiation. However, only a comprehensive tobacco control intervention can impact significantly on smoking prevalence as well as modify the smoking behavior.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Alfredo Tartarone) for the Series “Improving Outcomes in Lung Cancer Through Early Diagnosis and Smoking Cessation” published in Journal of Thoracic Disease. The article was sent for external peer review organized by the Guest Editor and the editorial office.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.02.23). The series “Improving Outcomes in Lung Cancer Through Early Diagnosis and Smoking Cessation” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. Report on the global tobacco epidemic. Geneva: World Health Organization, 2019.
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [Crossref] [PubMed]
- World Health Organization. Framework convention on tobacco control. Geneva: World Health Organization, 2008.
- Joossens L, Raw M. The tobacco control scale 2013 in Europe. Brussels: Association of European Cancer Leagues, 2013.
- World Health Organization. Guidelines for implementation of Article 6 of the WHO FCTC. Geneva: World Health Organization, 2014.
- European Commission. Directive 2014/40/EU of the European Parliament and of the Council of 3 April 2014 on the approximation of the laws, regulations and administrative provisions of the Member States concerning the manufacture, presentation and sale of tobacco and related products and repealing Directive 2001/37/EC. Off J Eur Union 2014;127:1-38.
- Moodie C, Hoek J, Scheffels J, et al. Plain packaging: legislative differences in Australia, France, the UK, New Zealand and Norway, and options for strengthening regulations. Tob Control 2019;28:485-92. [Crossref] [PubMed]
- van Ours JC. Dynamics in the use of drugs. Health Econ 2006;15:1283-94. [Crossref] [PubMed]
- Pirie K, Peto R, Reeves GK, et al. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet 2013;381:133-41. [Crossref] [PubMed]
- Wilkinson AL, Scollo MM, Wakefield MA, et al. Smoking prevalence following tobacco tax increases in Australia between 2001 and 2017: an interrupted time-series analysis. Lancet Public Health 2019;4:e618-27. [Crossref] [PubMed]
- Serrano-Alarcón M, Kunst AE, Bosdriesz JR, et al. Tobacco control policies and smoking among older adults: a longitudinal analysis of 10 European countries. Addiction 2019;114:1076-85. [Crossref] [PubMed]
- Palali A, van Ours JC. The impact of tobacco control policies on smoking initiation in eleven European countries. Eur J Health Econ 2019;20:1287-301. [Crossref] [PubMed]
- Gonzalez-Rozada M, Montamat G. How raising tobacco prices affects the decision to start and quit smoking: evidence from Argentina. Int J Environ Res Public Health 2019. [Crossref] [PubMed]
- van Hasselt M, Kruger J, Han B, et al. The relation between tobacco taxes and youth and young adult smoking: what happened following the 2009 U.S. federal tax increase on cigarettes? Addict Behav 2015;45:104-9. [Crossref] [PubMed]
- Dobbie F, Purves R, McKell J, et al. Implementation of a peer-led school based smoking prevention programme: a mixed methods process evaluation. BMC Public Health 2019;19:742. [Crossref] [PubMed]
- McGee CE, Trigwell J, Faircloug SJ, et al. Effect of a sport-for-health intervention (SmokeFree Sports) on smoking-related intentions and cognitions among 9-10 year old primary school children: a controlled trial. BMC Public Health 2016;16:445. [Crossref] [PubMed]
- Sharapova S, Reyes-Guzman C, Singh T, et al. Age of tobacco use initiation and association with current use and nicotine dependence among US middle and high school students, 2014-2016. Tob Control 2020;29:49-54. [Crossref] [PubMed]
- Meier A, Odermatt R, Stutzer A: Tobacco sales prohibition and teen smoking. IZA Discussion 2019:No. 12231.
- Nuyts PAW, Hewer RMF, Kuipers MAG, et al. Youth access to cigarettes across seven European countries: a mixed-methods study. Nicotine Tob Res 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Gorini G, Gallus S, Carreras G, et al. A long way to go: 20-year trends from multiple surveillance systems show a still huge use of tobacco in minors in Italy. Eur J Public Health 2019;29:164-9. [Crossref] [PubMed]
- Nogueira SO, McNeill A, Fu M, et al. Impact of anti-smoking advertising on health-risk knowledge and quit attempts across 6 European countries from the EUREST-PLUS ITC Europe Survey. Tob Induc Dis 2018;16:A5. [Crossref] [PubMed]
- England L, Tong VT, Rockhill K, et al. Evaluation of a federally funded mass media campaign and smoking cessation in pregnant women: a population-based study in three states. BMJ Open 2017;7:e016826. [Crossref] [PubMed]
- Ferketich AK, Lugo A, La Vecchia C, et al. Relation between national-level tobacco control policies and individual-level voluntary home smoking bans in Europe. Tob Control 2016;25:60-5. [PubMed]
- Jones AM, Laporte A, Rice N, et al. Do public smoking bans have an impact on active smoking? Evidence from the UK. Health Econ 2015;24:175-92. [Crossref] [PubMed]
- Boes S, Marti J, Maclean JC. The impact of smoking bans on smoking and consumer behavior: quasi-experimental evidence from Switzerland. Health Econ 2015;24:1502-16. [Crossref] [PubMed]
- Del Bono E, Vuri D. Smoking behaviour and individual wellbeing: a fresh look at the effects of the 2005 public smoking ban in Italy. Oxford Econ Pap 2017;70:741-62. [Crossref]
- Bullen C, Howe C, Laugesen M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet 2013;382:1629-37. [Crossref] [PubMed]
- Halpern SD, Harhay MO, Saulsgiver K, et al. A pragmatic trial of e-cigarettes, incentives, and drugs for smoking cessation. N Engl J Med 2018;378:2302-10. [Crossref] [PubMed]
- Hajek P, Phillips Waller A, Przulj D, et al. A randomized trial of e-cigarettes versus nicotine-replacement therapy. N Engl J Med 2019;380:629-37. [Crossref] [PubMed]
- Caponnetto P, Campagna D, Cibella F, et al. Efficiency and safety of an electronic cigarette (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One 2013;8:e66317. [Crossref] [PubMed]
- Nonnemaker JM, Farrelly MC. Smoking initiation among youth: the role of cigarette excise taxes and prices by race/ethnicity and gender. J Health Econ 2011;30:560-7. [Crossref] [PubMed]
- Sen A, Wirjanto T. Estimating the impacts of cigarette taxes on youth smoking participation, initiation, and persistence: empirical evidence from Canada. Health Econ 2010;19:1264-80. [Crossref] [PubMed]
- Cawley J, Markowitz S, Tauras J. Lighting up and slimming down: the effects of body weight and cigarette prices on adolescent smoking initiation. J Health Econ 2004;23:293-311. [Crossref] [PubMed]
- Tauras JA. Can public policy deter smoking escalation among young adults? J Policy Anal Manage 2005;24:771-84. [Crossref] [PubMed]
- DeCicca P, Kenkel D, Mathios A. Putting out the fires: will higher taxes reduce the onset of youth smoking? Econ Polit 2002;110:144-69. [Crossref]
- World Health Organization. Global Adult Tobacco Survey (Gats) Czech Republic Country Report. Geneva: World Health Organization, 2012.
- Bader P, Boisclair D, Ferrence R. Effects of tobacco taxation and pricing on smoking behavior inhigh risk populations: a knowledge synthesis. Int J Environ Res Public Health 2011;8:4118-39. [Crossref] [PubMed]
- Jayawardhana J, Bolton HE, Gaughan M. The association between school tobacco control policies and youth smoking behavior. Int J Behav Med 2019;26:658-64. [Crossref] [PubMed]
- Moreno MA, Whitehill JM. Influence of social media on alcohol use in adolescents and young adults. Alcohol Res 2014;36:91-100. [PubMed]
- Thomas R, Perera R. School-based programmes for preventing smoking. Cochrane Database Syst Rev 2006.CD001293. [PubMed]
- World Health Organization. Global Youth Tobacco Survey (Gyts) Czech Republic Country Report. Geneva: World Health Organization, 2016.
- García-Altés A, Pinilla J, Marí-Dell’Olmo M, et al. Economic impact of smoke-free legislation: did the Spanish tobacco control law affect the economic activity of bars and restaurants? Nicotine Tob Res 2015;17:1397-400. [Crossref] [PubMed]
- Kandra KL, Ranney LM, Lee JG, et al. Physicians' attitudes and use of e-cigarettes as cessation devices, North Carolina, 2013. PLoS One 2014;9:e103462. [Crossref] [PubMed]
- Kitzen JM, McConaha JL, Bookser ML, et al. E Cigarettes for smoking cessation: Do they deliver? J Clin Pharm Ther 2019;44:650-5. [PubMed]
- McRobbie H, Bullen C, Hartmann-Boyce J, et al. Electronic cigarettes for smoking cessation and reduction. Cochrane Database Syst Rev 2014.CD010216. [PubMed]
- Adriaens K, Van Gucht D, Declerck P, et al. Effectiveness of the electronic cigarette: an eight-week Flemish study with six-month follow-up on smoking reduction, craving and experienced benefits and complaints. Int J Environ Res Public Health 2014;11:11220-48. [Crossref] [PubMed]
- Brose LS, Hitchman SC, Brown J, et al. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction 2015;110:1160-8. [Crossref] [PubMed]
- Biener L, Hargraves JL. A longitudinal study of electronic cigarette use among a population-based sample of adult smokers: association with smoking cessation and motivation to quit. Nicotine Tob Res 2015;17:127-33. [Crossref] [PubMed]
- Tseng TY, Ostroff JS, Campo A, et al. A randomized trial comparing the effect of nicotine versus placebo electronic cigarettes on smoking reduction among young adult smokers. Nicotine Tob Res 2016;18:1937-43. [Crossref] [PubMed]
- Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation 2014;129:1972-86. [Crossref] [PubMed]
- Harrell PT, Simmons VN, Correa JB, et al. Electronic nicotine delivery systems (“E-cigarettes”) review of safety and smoking cessation efficacy. Otolaryngol Head Neck Surg 2014;151:381-93. [Crossref] [PubMed]
- Vickerman KA, Beebe LA, Schauer GL, et al. Electronic nicotine delivery system (ENDS) use during smoking cessation: a qualitative study of 40 Oklahoma quitline callers. BMJ Open 2017;7:e013079. [Crossref] [PubMed]
- Erku DA, Gartner CE, Do JT, et al. Electronic nicotine delivery systems (e-cigarettes) as a smoking cessation aid: a survey among pharmacy staff in Queensland, Australia. Addict Behav 2019;91:227-33. [Crossref] [PubMed]
- Brandon TH, Goniewicz ML, Hanna NH, et al. Electronic nicotine delivery systems: a policy statement from the American association for cancer research and the American society of clinical oncology. J Clin Oncol 2015;33:952-63. [Crossref] [PubMed]
- Grana RA, Popova L, Ling PM. A longitudinal analysis of electronic cigarette use and smoking cessation if only electronic cigarettes were effective smoking cessation devices. JAMA Intern Med 2014;174:812-3. [Crossref] [PubMed]
- Hartmann-Boyce J, McRobbie H, Bullen C, et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev 2016;9:CD010216. [PubMed]
- Livingston CJ, Freeman RJ, Costales VC, et al. Electronic nicotine delivery systems or e-cigarettes: American college of preventive medicine’s practice statement. Am J Prev Med 2019;56:167-78. [Crossref] [PubMed]
- Glasser AM, Collins L, Pearson JL, et al. Overview of electronic nicotine delivery systems: a systematic review. Am J Prev Med 2017;52:e33-66. [Crossref] [PubMed]
- El Dib R, Suzumura EA, Akl EA, et al. Electronic nicotine delivery systems and/or electronic non-nicotine delivery systems for tobacco smoking cessation or reduction: a systematic review and meta-analysis. BMJ Open 2017;7:e012680. [Crossref] [PubMed]
- Malas M, van der Tempel J, Schwartz R, et al. Electronic cigarettes for smoking cessation: a systematic review. Nicotine Tob Res 2016;18:1926-36. [Crossref] [PubMed]
- Khoudigian S, Devji T, Lytvyn L, et al. The efficacy and short-term effects of electronic cigarettes as a method for smoking cessation: a systematic review and a meta-analysis. Int J Public Health 2016;61:257-67. [Crossref] [PubMed]
- Rahman MA, Hann N, Wilson A, et al. E-cigarettes and smoking cessation: evidence from a systematic review and meta-analysis. PLoS One 2015;10:e0122544. [Crossref] [PubMed]
- Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med 2016;4:116-28. [Crossref] [PubMed]
- Dasgupta P, Rizwani W, Pillai S, et al. Nicotine induces cell proliferation, invasion andepithelial-mesenchymal transition in a variety of human cancer cell lines. Int J Cancer 2009;124:36-45. [Crossref] [PubMed]
- Zhang Y, Upson D. E-cigarettes versus nicotine-replacement therapy for smoking cessation. N Engl J Med 2019;380:1973. [Crossref] [PubMed]
- Stein JH, Korcarz CE. E-cigarettes versus nicotine-replacement therapy for smoking cessation. N Engl J Med 2019;380:1973-4. [Crossref] [PubMed]
- Patel D, Davis KC, Cox S, et al. Reasons for current e-cigarette use among U.S. adults. Prev Med 2016;93:14-20. [Crossref] [PubMed]
- Maglia M, Caponnetto P, Di Piazza J, et al. Dual use of electronic cigarettes and classic cigarettes: a systematic review. Addict Res Theory 2018;26:330-8. [Crossref]
- Hajek P, Peerbux S, Phillips-Waller A, et al. Are ‘dual users’ who smoke and use e-cigarettes interested in using varenicline to stop smoking altogether, and can they benefit from it? A cohort study of UK vapers. BMJ Open 2019;9:e026642. [Crossref] [PubMed]
- Selya AS, Dierker L, Rose JS, et al. The role of nicotine dependence in e-cigarettes' potential for smoking reduction. Nicotine Tob Res 2018;20:1272-7. [Crossref] [PubMed]
- Sohal SS, Eapen MS, Naidu VGM, et al. IQOS exposure impairs human airway cell homeostasis: direct comparison with traditional cigarette and e-cigarette. ERJ Open Res 2019. [Crossref] [PubMed]
- Auer R, Concha-Lozano N, Jacot-Sadowski I, et al. Heat-not-burn tobacco cigarettes: smoke by any other name. JAMA Intern Med 2017;177:1050-2. [Crossref] [PubMed]
- Leigh NJ, Palumbo MN, Marino AM, et al. Tobacco-specific nitrosamines (TSNA) in heated tobacco product IQOS. Tob Control 2018;27:s37-8. [Crossref] [PubMed]
- Shein M, Jeschke G. Comparison of free radical levels in the aerosol from conventional cigarettes, electronic cigarettes, and heat-not-burn tobacco products. Chem Res Toxicol 2019;32:1289-98. [Crossref] [PubMed]
- Glantz SA. Heated tobacco products: the example of IQOS. Tob Control 2018;27:s1-6. [Crossref] [PubMed]
- De Marco C, Borgini A, Ruprecht AA, et al. Formaldehyde in electronic cigarettes and in heat-not-burn products: let's make the point. Epidemiol Prev 2018;42:351-5. [PubMed]
- Salman R, Talih S, El-Hage R, et al. Free-base and total nicotine, reactive oxygen species, and carbonyl emissions from IQOS, a heated tobacco product. Nicotine Tob Res 2019;21:1285-8. [Crossref] [PubMed]
- Moazed F, Chun L, Matthay MA, et al. Assessment of industry data on pulmonary and immunosuppressive effects of IQOS Tob Control 2018;27:s20-5. [Crossref] [PubMed]
- Dautzenberg B, Dautzenberg MD. Systematic analysis of the scientific literature on heated tobacco. Rev Mal Respir 2019;36:82-103. [Crossref] [PubMed]
- Liu X, Lugo A, Spizzichino L, et al. Heat-not-burn tobacco products: concerns from the Italian experience. Tob Control 2019;28:113-4. [PubMed]
- Farsalinos KE, Yannovits N, Sarri T, et al. Carbonyl emissions from a novel heated tobacco product (IQOS): comparison with an e-cigarette and a tobacco cigarette. Addiction 2018;113:2099-106. [Crossref] [PubMed]
- American Cancer Society, Inc. ACS Medical Content and News Staff. Available online: https://www.cancer.org/cancer/acs-medical-content-and-news-staff.html
- Bafunno D, Catino A, Lamorgese V, et al. Tobacco control in Europe: a review of campaign strategies for teenagers and adults. Crit Rev Oncol Hematol 2019;138:139-47. [Crossref] [PubMed]
- Theron AJ, Feldman C, Richards G, et al. Electronic cigarettes: where to from here? J Thorac Dis 2019;11:5572-85. [Crossref] [PubMed]