
The use of prefilled adrenaline syringes improves cardiopulmonary resuscitation quality—high-fidelity simulator-based study
Introduction
Sudden cardiac arrest (SCA) affects from 350,000 to 700,000 people per year in Europe and over 380,000 in the United States. The importance of following steps of survival chain such as fast notifying of the rescue system, performing cardiopulmonary resuscitation (CPR) by accident witnesses, using an automated external defibrillator (AED) and introducing an integrated post-resuscitation is frequently emphasized. They may have direct impact on the survival rate following out-of-hospital SCA. In addition, it is essential that paramedics undertake advanced life support (ALS) procedures that aim at the return of spontaneous circulation (ROSC). Continuous improvement of each of the chain links is crucial for improvement of the survival rate of SCA patients (1,2).
Performing ALS procedures needs to focus on prioritizing the tasks. It mainly concerns the short-handed rescue teams. The Polish law on the National Medical Emergency Services states that rescue teams must consist of at least 2 paramedics (3). However, there are many reports that have proven it impossible for the two-paramedics teams to satisfy the requirements of restrictive protocols, described by European Resuscitation Council (ERC), including the time criteria (4).
It is significant in such cases to apply the newest therapeutic solutions, which will facilitate the prioritizing process as well as the time reduction of certain procedures. All of the current guidelines of procedural algorithm in SCA, indicate the necessity of routine adrenaline (epinephrine) administration, regardless of SCA mechanism. Notwithstanding, those recommendations concentrate on defining the frequency and route of drug administration rather than on the method of its preparation. It is extremely important, especially for the short-handed teams, to search for simplification of the procedures, which will enable paramedics to focus on their priorities (5).
The aim of the research was to test the effect of various adrenaline preparation methods on the quality of CPR during SCA.
Methods
Study group
To conduct the study, the authors designed a randomized simulative cross-study attended by 100 randomly assigned two-person teams, consisting of professionally active paramedics. Their age range varied from 28 to 54 years. All study group members have had an experience in emergency departments of minimum 5 years.
The study has been approved by a local bioethics committee (KB 1075/19). All of the participants have given their consent to take part in the simulation. No additional financial support has been searched to carry on the study.
Simulator
The study was based on a high-fidelity simulator Resusci Anne QCPR (Laerdal - Stavanger, Norway). The mannequin records chest compressions (CC) and ventilation parameters. Moreover, the mannequin’s respiratory tracts enable intubations, insertion of supraglottic airway device (SAD) and ventilation with a use of a bag valve mask followed by a visible chest movement. Its arms have been filed with artificial blood with the aim of verifying proper venipuncture performed by paramedics. The mannequin also simulates the carotid artery and single peripheral artery pulse.
Equipment and medicines
Two simulation rooms were arranged identically and were equipped with the same devices. The study group was well-versed with the room itself, available equipment and medicines as well. Before the scenario, a prebriefing session was conducted in order to familiarize paramedics with simulator features and equipment distribution across the room. The study group had at their disposal a previously-known defibrillator ZOLL M-Series and two sets of medicines. The former was equipped with glass ampoules with adrenaline 1 mg in 1 mL (adrenaline; WZF, Warsaw, Poland), factory packed in a plastic packaging. The latter was equipped with prefilled syringes with adrenaline 1 mg in 10 mL 1:10,000 (adrenaline; Aguettant Ltd, Bristol, United Kingdom) in an aluminum packaging. It is the only drug in a prefilled syringe on the Polish market, which is approved to be administered for SCA patients. Furthermore, each team had at their disposal physiological saline in 500 mL containers with a mini spike to dilute the liquid. All the medicines used in the study exceeded the expiration date and were donated by a local hospital pharmacy.
Scenario
Each team took part in two 10-minute scenarios featuring SCA. The heart rhythm visible on the monitor was the same during each analysis [pulseless electrical activity (PEA)]. In the first scenario only traditional ampoules with adrenaline (1 mg in 1 mL) were available (group ST). Paramedics needed to aspirate medicines from ampoules and dilute them according to specification in order to administer them intravenously. In the second scenario the teams were provided with prefilled syringes with adrenaline (1 mg diluted to 10 mL) (group AMPS). In between scenarios the teams had a break of 15 minutes, during which the facilitators did not sum up their performance. The order of scenarios was random.
Storing and processing data
All data regarding the quality of CC was recorded with the use of Laerdal PC SkillReporting System 2.0. (Laerdal Medical, Stavanger, Norway). The analyses and simulations were conducted by qualified medical simulation instructors. The following parameters of CC quality such as chest compression fraction (CCF), average no flow time, proper hands position, total number of CC, average CC depth, percentage of CC with a proper depth, average CC rate, percentage of CC with a proper rate and percentage of CC with a proper chest relaxation (chest recoil) were recorded and then analyzed.
Additionally, independent timekeepers measured the time of the following steps: adrenaline administration, performing a venipuncture and airways support with SAD.
Data processing and statistical analysis
Regarding continuous data, they were checked for normality with the use of the Shapiro-Wilk W test. These satisfying the criteria of normal distribution were expressed as the mean with standard deviation (SD) and unpaired t-test was applied to estimate differences between groups. The categorical variables were presented as the numbers (n) with percentage (%) and then they were compared between subgroups with the use of the Yates corrected χ2 test. Correlations between selected variables describing action of paramedics (i.e., adrenaline preparation or administration) and indices of cardio-pulmonary resuscitation (i.e., CCF or no flow time) were assessed by means of either parametric Pearson correlation coefficient or non-parametric Spearman rank correlation test. A P value below 0.05 was considered of statistical significance. All the data was inserted into an excel file whereas the statistical analysis was performed with the use of Statistica 10.0 for Windows (StatSoft, Inc., Tulsa, OK, USA).
Results
Time of adrenaline preparation and injection
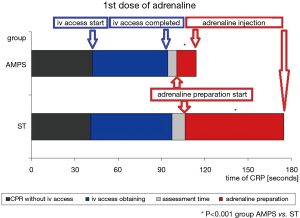
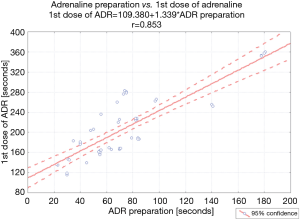
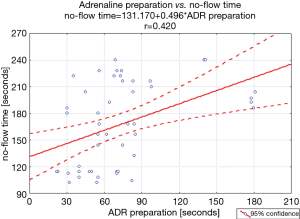
The first dose of adrenaline was injected intravenously after 114.2±28.3 seconds of CRP initiation in group AMPST and after 178.1±62.6 seconds in group ST (P<0.001). Since the time of obtaining venous vascular access [either start (42.3±15.8 vs. 41.0±22.8 seconds of CPR) or completion (94.5±17.0 vs. 100.5±38.0 seconds of CPR) of this action; in group AMPS and ST, respectively] did not differ between groups, an aforementioned delay in the first drug dose administration in AMPS patients resulted exclusively from significant difference in drug preparation time (13.4±6.9 vs. 68.6±38.7 seconds, in group AMPS and ST, respectively). To clarify this difference, time-flow charts with the absolute times of the consecutive stages of CPR expressed in seconds until the first dose of adrenaline are presented in the Figure 1. Moreover, in group ST, drug preparation time correlated significantly with the time-point of the first dose of adrenaline administration (Figure 2).
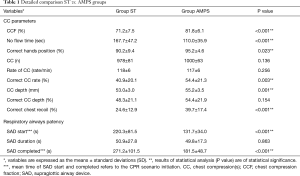
Comparison of cardio-pulmonary resuscitation quality
The most important variables that characterize quality of resuscitation differed significantly between groups. The indices of CPR favored group that received adrenaline with prefilled syringes. Among others, CCF, mean depth of CC, rate of optimal chest recoil after CC, appropriate rate were higher in this group. Moreover, no flow time as well as supraglottic airway device introduction to make respiratory airways open were significantly shorter when compared to group with adrenaline in standard ampoules. The detailed values of these parameters are outlined in Table 1.
Full table
Association of drug preparation time with parameters of CPR quality
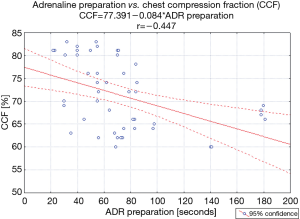
Drug preparation time was proved to have significant impact on the quality of CPR. Longer preparation, although checked only in AMPS scenario, negatively influenced some parameters of CC and maintenance of respiratory airways patency. Delay in adrenaline injections in group ST resulted predominantly from longer preparation of this medication (r=0.85; P<0.001; Figure 2). In this group, longer preparation of adrenaline resulted in worse quality of resuscitation. It correlated significantly and negatively with CCF (r=−0.45; P=0.001, Figure 3) and positively with no flow time (r=0.42; P=0.002; Figure 4). Moreover, negative impact of delayed adrenaline injection on rate of CC (r=−0.52; P<0.001) and appropriate chest recoil (r=−0.38; P=0.006) were also noted. Additionally, statistical analysis revealed significant and positive correlation (r=0.48; P<0.001) time of adrenaline preparation and the period of SAD introduction (as the difference between SAD completed and SAD start).
Discussion
The research on optimization of SCA treatment has been conducted for many years. We hope the findings of our study will expand our knowledge in this area of interest. Several scientific studies have contributed to the creation of specialized organizations, which scrutinize recent reports that may increase patients’ chances of survival. Since 2010 both American Heart Association (AHA) and ERC have been advocating a use of adrenaline in each of circulatory arrest mechanism in a dose of 1 mg every 3 to 5 minutes (2,5). The guidelines emphasize that it is substantial to carry out more extensive research on the effectiveness of adrenaline administration (6). Although injection of adrenaline remains one of the most common actions in ALS procedures, scientists are still inconsistent about the effectiveness of its administration in SCA patients. Retrospective observational studies that involved 6,033 patients (data received from National Cardiopulmonary Resuscitation Registry) have shown that administration of adrenaline within the in-hospital treatment resulted not only in the lower rate of ROSC but also in a 30-day survival (7). There are many animal tests which have shown a positive impact of adrenaline on perfusion of the most important organs, but simultaneously it might compromise microcirculation (8). Moreover, impact of adrenaline administration on long-term outcomes in SCA patients is unknown (9). Numerous clinical observations together with retrospective medical records analyses and meta-analyses have demonstrated a deterioration of patients’ long-term results after adrenaline administration (6). On the other side, other reports have shown considerable improvement of neurological results after discharge (10). Thus, it is essential to lead clinical studies in order to resolve the remaining doubts.
Medical Rescue Teams differ depending on specific regulations provided by health care system in each country. The distinctions encompass composition and competences of team members together with types of patients to be assisted. AHA have introduced a concept of work dynamics of a resuscitation team (11). According to their guidelines, regardless of the number of team members, there are 6 roles to be played during CPR. These include: (I) team leader, (II) person performing CC, (III) person performing ventilation, (IV) person operating a cardiac monitor, (V) person preparing and administering medicines and (VI) time-keeper. Medical Rescue Team is the most effective with 6 members on board, each of whom takes responsibility for the specific role. The fewer members in a team, the more roles are to be performed by one person simultaneously. This precludes paramedics from focusing on a priority action of high-quality CC (11). Unfortunately, in Polish health-care system paramedics usually work on SCA pair-wise. Each of them needs to perform 3 roles in order to ensure proper effectiveness of CPR. The teams adopt a sort of a medical compromise, which eliminates certain steps towards those of a higher priority. In the initial phase one of the paramedics performs basic life support (BLS) procedures, whereas their partner prepares for implementation of advanced routines.
Our study has proven that introducing prefilled syringes accelerated the time of first adrenaline administration. It also confirms findings in the previously published studies that compared administration time of drugs in prefilled syringes versus traditional ampoules (12,13). Prefilled syringes have significantly reduced drug preparation time. Subhi et al. showed additionally that this method has eliminated most of the preparation phase steps such as disinfection of an ampoule, application and removal of a needle for aspiration, and dilution of a drug to a desired amount (13). Moreover, a risk of contamination has decreased. Reducing the preparation time enables the paramedics to focus on other priorities (13). In another study, Ornato et al. explored an effect of errors committed during CPR on a patient survival rate on a huge number of in-hospital cardiac arrest (IHCA) cases (more than 118,000) (14). The most frequent lapses consisted in a delay of drug administration—even over 5 minutes since diagnosis. Eventually, it has contributed to a decrease in a survival rate of IHCA individuals (14). A use of prefilled syringes not only reduces the administration time, but it also substantially increases patients’ safety (15). In the authors’ study, most team members responsible for preparing the medicines omitted certain steps when using traditional ampoules. Hardly ever did they use a separate needle, but aspirated adrenaline directly to a syringe instead.
It must be pointed that routine application of drugs in the prefilled syringes has also potential disadvantages. A complex structure of such prepared medicines constitutes a real challenge for the manufacturers who need to ensure safe production and effectiveness of the medicine. Furthermore, the materials used to produce prefilled syringes must be thoroughly tested to minimize the risk of interaction between the material and the medicine stored in it. Moreover, diluted drugs ready for application may be less stable than their concentrates. At last, the complex production process and research generate high cost of prefilled syringes (16).
The study also revealed that prefilled syringes have enhanced the quality of CPR as proved by an increased proportion of time devoted to uninterrupted CC and a decrease in no flow time factor. Moreover, a use of prefilled syringes has resulted in making a faster decision about supraglottic airway devices application. This method followed by a confirmation of accurate ventilation, enabled paramedics to performed asynchronous CC. During the study all the teams provided this type of compressions, what caused an increased CCF and a decrease in no flow time factor. High-quality CC have been confirmed to be a crucial element of CPR, which have significantly improved SCA patients’ prognosis (17). AHA with ERC point out to the importance of minimalizing pauses in CC (18,19). They stressed that each pause resulted in decreasing blood flow in the coronary vessels and through the central nervous system. Thus, many experts agree that uninterrupted CC are associated with higher survival rate (18). An importance of CC quality was pointed out by AHA and some clinically useful parameters (e.g., CCF) were included in its guidelines from 2015 (20). CCF defines the period of time devoted to uninterrupted CC, which shall exceed 60%. However, the best results are accomplished with CCF exceeding 80% (17,21). To reach these values, procedures performed during CC should be simplified. Drugs administration represents one of these procedures (20). Our analysis has revealed that simplification of drug administration during CPR led to an increase in CCF accompanied by a decrease in no flow time.
Moreover, we supported a current trend to apply more extensively high-fidelity simulation to test hypothesis difficult to examine on the human beings. The simulator-based studies enable researchers to verify whether performing a certain method in a particular way has an impact on critical steps in patient treatment (22). It helps to develop a well-prospering chain of procedures devoid of errors, which allows paramedics to focus on priorities. It is of the utmost importance when patient treatment is multi-stage or when the team is short-handed. Therefore, due to the conducted analysis the authors were able to assess how the simplification of adrenaline administration affects the quality of CPR. The authors’ analysis revealed that a use of prefilled syringes during CPR impacts significantly the quality of CPR in two-person teams. The reduction of time devoted to drug administration arose from elimination of some of the preparatory steps. The authors are aware of limitations of their research. It is obvious that performing studies on mannequins even on high-fidelity simulators, has a different value than analyses of outcomes in the clinical trials. The latter, particularly randomized and double-blind involving SCA patients may raise some clinical concerns. On the other hand, high-fidelity simulation enables to examine and then standardize many, not only emergency, procedures, and to limit the factors that might influence the final outcome. It must be stressed that equipment used in our study was the same for each scenario. In reality, frequently medicine and other devices used during prehospital SCA differs in each ambulance. In the study only one type of prefilled syringes was used. However, currently numerous types of prefilled syringes of various structure and packaging are commercially available. These aforementioned differences may have an impact on preparation and administration of the medicines thus eventually on final clinical outcomes of CPR.
Conclusions
It has been proven that a simplification of adrenaline administration by a use of prefilled syringes considerably enhances the quality of CPR because it enables paramedics to focus on priorities such as CPR quality and overall accuracy of procedures.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.04.33). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study has been approved by a local bioethics committee (KB 1075/19). All of the participants have given their consent to take part in the simulation.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Perkins GD, Handleyc AJ, Koster RW, et al. Adult basic life support and automated external defibrillation. In: European Resuscitation Council Guidelines for Resuscitation 2015: Section 2. Resuscitation 2015;95:81-99. [Crossref] [PubMed]
- Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics -2012 update: a report from the American Heart Association. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2012;125:2-10.
- Dz.U. 2018 poz. 1115 Ustawa z dnia 10 maja 2018 r. o zmianie ustawy o Państwowym Ratownictwie Medycznym oraz niektórych innych ustaw. Dziennik Ustaw 2018poz. 1115.
- Dabrowski M, Sip M, Dabrowska A, et al. It is impossible to follow the ERC algorithm in a two-paramedics ambulance team. Resuscitation 2017;118:43. [PubMed]
- Soara J, Nolanb JP, Böttigerd BW, et al. Adult advanced life support. In: European Resuscitation Council Guidelines for Resuscitation 2015: Section 3 Resuscitation. 2015;95;100-47.
- Morales-Cané I, Del Rocío Valverde-León M, Aurora Rodríguez-Borrego M, et al. Epinephrine in cardiac arrest: systematic review and meta-analysis. Rev Lat Am Enfermagem 2016;24:e2821. [Crossref] [PubMed]
- Lundin A, Rylander C, Karlsson T, et al. Adrenaline, ROSC and survival in patients resuscitated from in-hospital cardiac arrest. Resuscitation 2019;140:64-71. [Crossref] [PubMed]
- Kornberger E, Lindner KH, Mayr VD, et al. Effects of epinephrine in a pig model of hypothermic cardiac arrest and closed-chest cardiopulmonary resuscitation combined with active rewarming. Resuscitation 2001;50:301-8. [Crossref] [PubMed]
- Gough CJR, Nolan JP. The role of adrenaline in cardiopulmonary resuscitation. Critical Care 2018;22:139. [Crossref] [PubMed]
- Cody P, Lauderdale S, Hogan DE. Comparison of Two Protocols for Pulseless Cardiopulmonary Arrest: Vasopressin Combined with Epinephrine Versus Epinephrine Alone. Prehosp Disaster Med 2010;25:420-3. [Crossref] [PubMed]
- Hunziker S, Johansson AC, Tschan F, et al. Teamwork and Leadership in Cardiopulmonary Resuscitation. J Am Coll Cardiol 2011;57:2381-8. [Crossref] [PubMed]
- Helm C, Gillett M. Adrenaline in cardiac arrest: Prefilled syringes are faster. Emerg Med Australas 2015;27:312-6. [Crossref] [PubMed]
- Subhi Y, Kjer B, Munch IC. Prefilled syringes for intravitreal injection reduce preparation time. Dan Med J 2016;63:A5214. [PubMed]
- Ornato JP, Peberdy MA, Reid RD, et al. Impact of resuscitation system errors on survival from in-hospital cardiac arrest. Resuscitation 2012;83:63-9. [Crossref] [PubMed]
- Tilleul P, Mons B, Schmitt C, et al. Intravenous drug preparation practices: a survey in a French university hospital. Pharm World Sci 2003;25:276-9. [Crossref] [PubMed]
- Makwana S, Basu B, Makasana Y, et al. Prefilled syringes: An innovation in parenteral packaging. Int J Pharm Investig 2011;1:200-6. [Crossref] [PubMed]
- Christenson J, Andrusiek D, Everson-Stewart S, et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation 2009;120:1241-7. [Crossref] [PubMed]
- Cunningham LM, Mattu A, O'Connor RE, et al. Cardiopulmonary resuscitation for cardiac arrest: the importance of uninterrupted chest compressions in cardiac arrest resuscitation. Am J Emerg Med 2012;30:1630-8. [Crossref] [PubMed]
- Callaway CW, Jasmeet S, Mayuki A, et al. International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations Part 4: Advanced Life Support. Circulation 2015;132:S84-145. [Crossref] [PubMed]
- Hazinski MF, Shuster M, Donnino MW, et al. Highlights of the 2015 American Heart Association Guidelines Update for CPR and ECC. Circulation 2015;132:7-8. [PubMed]
- Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation 2013;128:417-35. [Crossref] [PubMed]
- Puślecki M, Ligowski M, Dąbrowski M, et al. The role of simulation to support donation after circulatory death with extracorporeal membrane oxygenation (DCD-ECMO). Perfusion 2017;32:624-30. [Crossref] [PubMed]


