Impact of automatic chest compression devices in out-of-hospital cardiac arrest
Introduction
The history of cardiopulmonary resuscitation (CPR) is dated back to the middle of the last century. It has been proven that sudden cardiac arrest (SCA) survival rate is dependent on many factors. These include, among others: first analyzed hearth rhythm, resuscitation performed by bystanders, and immediate defibrillation before ambulance arrival. Even though one-third of patients achieve the return of spontaneous circulation (ROSC), the survival rate is about 8%. This rate also varies between countries (1). In the last years, considerable progress in knowledge has been made. Technologies such as extracorporeal CPR (ECPR), intra-arrest therapeutic hypothermia, and coronary angiography are being implemented more and more widely. Stub and colleagues reported that their use allows increasing survival with a good neurological outcome to 54% (2).
Chest compressions (CCs) are an essential part of efficient cardiopulmonary resuscitation. Hands-only bystander resuscitation is strongly recommended. CCs of good quality should ensure proper flow in the coronary arteries (3). It was shown that optimal blood flow (e.g., assessed on the base diastolic flow velocity) and cerebral perfusion had a direct and marked impact on the patient›s survival and neurological outcome (4). The CC quality criteria include proper rate and adequate depth of CCs, full chest recoil, and minimal interruptions during CCs (5).
Manual CC can be performed by the bystander, immediately after SCA before the arrival of the ambulance. However, during patient transport, it is difficult to perform good quality manual CCs. Moreover, it is very exhausting for a rescuer. Very often only the first minutes of CCs are of optimal quality (6). This time is obviously too short time to restore adequate perfusion through vital organs. On the other hand, the automatic chest compression devices (ACCD) can function even up to one hour, when disconnected from power supply. Furthermore, it is able to provide CC with constant depth and strength (7). However, its application features some drawbacks. We know from our daily practice it usually takes time to install them around the thorax. Additionally, they cannot be used in children and extremely obese people, and they are relatively expensive medical devices.
Currently, two technologies are available on the market. The first one is a piston-type device that presses directly on the sternum (8). The second technology is the load-distribution band (9). The chest band shortens its length and thus reduces the volume of the entire thorax. Each technique has its advantages and disadvantages, and so far, none of them has been proven to be superior in both out-of- and in-hospital cardiac arrest patients (10,11). At the moment, no investigations are indicating unambiguously an increase in survival among patients treated with ACCD compared to manual CCs (12). Although some studies showed the superiority of ACCD (6,13), the others, including also randomized assessments and a recently released meta-analysis, did not find any improvement in clinical outcomes in out of hospital cardiac arrest patients (14,15). Moreover, there are reports suggesting that these devices can cause more internal injuries than during manual CCs (11,16).
Striving to reduced employment in medical rescue teams due to both a lack of well-educated paramedics and cost-effective policy in Emergency Medical Services (EMS) resulted in a fact that for a few years, two-man teams have been sent to out-of-hospital cardiac arrest (OHCA) patients in many cities in Poland.
This study aimed to estimate if availability of ACCDs for two-man rescue teams had any impact on CPR effectiveness defined as ROSC followed by successful transport of patients after OHCA to the emergency departments.
Methods
Study design
The study was designed as a retrospective cohort study. The research tool was the analysis of obligatory medical reports such as dispatch cards and medical procedures records used in EMS in one million agglomeration in Poland. This study involved only ambulances that were sent to OHCA patients between January and December 2018. Among 24 ambulances, half of them were equipped with ACCD. OHCA individuals were divided retrospectively into two sets with respect to the applied method of CCs, group ACCD when mechanical (n=181), and group MCC-manual compressions (n=303) were carried out. Additionally, to assess the impact of age on CPR effectiveness, Moreover, having in mind the possibility of ECPR utilization we split all OHCA individuals into other two subgroups, younger (subgroup Y; n=194) with age below 65 years old suitable for ECPR and the elderly (subgroup E; n=290).
The survey protocol has been approved by the Institutional Review Board of Poznan University of Medical Sciences (No: KB764/19). Access to medical records was granted by the Poznan EMS Authorities.
Protocol
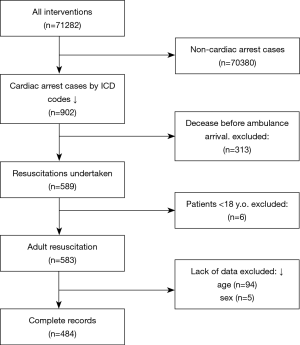
From all the interventions, records coded with ICD-10 codes: I46 (cardiac arrest), I46.0 (Cardiac arrest with successful resuscitation), I46.1 (Sudden cardiac death, so described), or I46.9 (Cardiac arrest, unspecified) were chosen. After deleting the duplicate records, the final number of cardiac arrest cases were determined. In the next stage, the cases whose death was diagnosed prior to ambulance arrival were discarded from further analysis. The records with incomplete data, as well as regarding pediatric cases were then deleted. Eventually, the extracted data were analyzed. The flowchart of the study is presented in Figure 1.
The following variables such as gender (male/female), age, area of intervention (city/countryside), ROSC and successful transport to hospital were compared between subgroups.
Data management and statistical analysis
The continuous variables are presented as the mean with standard deviation as they satisfied the criteria of normal distribution (confirmed in the Wilk-Shapiro W test). They were compared between the groups by means of unpaired Student T test. The categorical variables were expressed as the numbers (n) with percentages (%). For statistical analysis χ2 test and Yeats corrected χ2 test were used as appropriate. A P value less than 0.05 was considered as significant. The analysis was performed using the Statistica 12 software (Tibco Inc., Tulsa, OK, USA).
Results
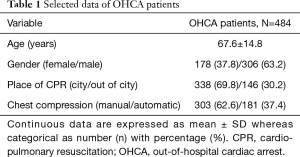
The study included 71,282 medical charts of Poznan EMS. After considering the inclusion and exclusion criteria, only 484 OHCA subjects were qualified for the final analysis. The mean age was 67.6±14.8 years (ranged from 18 to 96). The majority of them were male. SCA was detected more often in the city area. The selected data of individuals are outlined in Table 1.
Full table
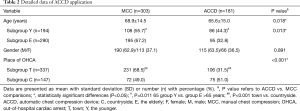
Application of ACCD by paramedics
Generally, in spite of the fact that half of ambulances were equipped in ACCD, only in 181 individuals (37.4%) these devices were used. Interestingly, the rate of ACCD applications was significantly higher at the countryside/suburban area than in the town center. The mean age of these patients was lower, and more subjects received treatment with ACCD in the younger group. The detailed data regarding the use of ACCD are presented in Table 2.
Full table
Association between ACCD use and quality of CPR
The most important finding was that ACCD significantly improved quality and effectiveness of CPR expressed as a number of the subjects with ROSC. ROSC rate for ACCD patients was 63.5% whereas below 50% in group MCC (P=0.003) (Figure 2).
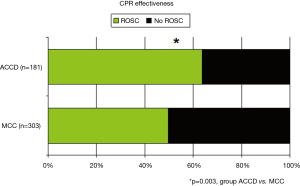
More detailed analysis in the subgroups with respect to age of patients and place of OHCA revealed that in younger OHCA individuals defined as at the age of equal or below 65, the rate of ROSC was higher if ACCD was applied (P<0.05 vs. MCC). Additionally, more ROSC patients were noted if ACCD was used within town borders. No differences in CPR effectiveness (defined as ROSC) with respect to the method of chest compression (ACCD vs. MCC) were seen if CPR was carried out on the elderly subject and if OHCA had place in the countryside. The detailed numbers are presented in Table 3.
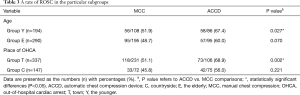
Full table
Comparison of ROSC and no-ROSC subject
Comparing parameters between ROSC and no-ROSC subjects that could have an impact on the effect of CPR performed by two-man rescue teams, we found that ROSC subjects were significantly younger, and ACCD was applied markedly more often than MCC. Interestingly, other variables, particularly initial rhythm and witnessed OHCA, did not differ between ROSC and no-ROCS cases. The results are summarized in Table 4.
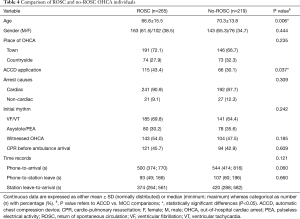
Full table
Discussion
The authors attempted to answer the question of whether the presence of ACCD in ambulance increases the number of patients transported to emergency departments.
The role of ACCD has not been fully clarified. Currently, routine use is not recommended (17). However, it is suggested to consider their use in cases where high-quality compressions are not achievable. These are CPR during transport, prolonged CPR due to for instance hypothermia, simultaneous performance of medical procedures such as primary coronary intervention, poisoning, thrombolysis in a patient with pulmonary embolism, or limited space. Although the guidelines do not indicate this, ACCD can also be useful in two-paramedic staffed ambulances. In such teams, it seems impossible to adequately perform ALS following the protocol (18).
The results of the meta-analysis performed by Kahn et al. showed that manual compressions were comparable or even more effective than LUCAS and AutoPulse in improving survival within 30 days of discharge from hospital and neurological recovery (11). Wroe et al. describe cases of malfunction of the ACCD. At the same time, he points the needs for proper training in using ACCD, which may reduce the number of errors (19).
The cost-effectiveness analysis performed by Marti et al. showed that routine use of mechanical CPR devices in the out-of-hospital setting was not satisfactory when compared to standard manual chest compression (20). In the United States, the total cost of OHCA treatment has been estimated at $33 billion per year (21). The costs were higher for non-survivors. Therefore, the use of ACCD increases the number of admissions to a hospital without improving long-term outcomes. This may become a challenge for intensive care units.
On the other hand, ACCD offers the possibility of using opportunities not yet available in prehospital care. One of them is ECPR with the use of extracorporeal perfusion devices. In this form of resuscitation, a type of cardiopulmonary bypass [extracorporeal membrane oxygenation (ECMO)] is introduced, maintaining circulation until the effective cardiac output is reestablished. This technique improves coronary perfusion and keeps the heart and brain perfusion, increasing the chance of ROSC (22). The inflow of oxygenated blood to the brain and vital organs reduces organ dysfunction and improves the probability of survival with good neurological outcome. One of the conditions for implementing the ECPR program in prehospital care is that compressions should be performed automatically. The use of ECPR may be a solution to the problem of overloading of intensive care units described above. However, this requires proper preparation and organization on one side of the health care system. Another challenge is using ACCD to maintain perfusion of organs for transplantation in patients with irreversible cardiac arrest. This strategy, in combination with ECMO, significantly increases donation activity (23).
According to the results presented in this paper, ACCD was used more often in the group of patients aged 18–65 years than in the elderly. This result creates a picture of the potential group of ECPR recipients. The question remains whether it is possible to perform automatic compression in pediatric patients. Individual cases are described in the literature (24). Animal model studies have also been conducted, which have not shown any difference (25). However, there are no clear recommendations on this subject so far.
Data analysis revealed that ROSC was more common if ACCD was used. The survival of a patient with SCA is most affected by high-quality CPR and automatic defibrillation undertaken by witnesses to the event. The benefits of advanced life support (ALS) procedures such as medication and advanced airway management are still uncertain (26). However, even ALS must be conducted without compromising the quality of basic life support (BLS) like chest compressions. A higher incidence of ROSC may be influenced by the fact that ambulances equipped with ACCD were staffed by two-paramedic. A team consisting of two rescuers may not be able to perform all the actions according to the ALS algorithm (18). In such situations, the highest priority should be given to the most important procedures, and a medical compromise should be reached. Implementation of ACCD to two-paramedic teams may, therefore, improve the quality of resuscitation, but additional investigations are needed in this field.
The authors of this paper are aware of its limitations. First of all, it should be mentioned that either ROSC or survival depends on many components. The most important are: bystander CPR, defibrillation performed prior to the arrival of the ambulance, and the occurrence of initial shockable rhythm. This data are missing in the presented paper. All analyses of the survival of SCA patients should be based on the Utstein protocol. This protocol contains the most essential information about the process of resuscitation, the first rhythm or the suspected cause of cardiac arrest. There is no obligation to include such information in the medical records of the Polish emergency medical system. Medical records are completed with varying degrees of accuracy. The lack of legal requirements for records keeping in the aspect of resuscitation prevents a reliable analysis. The authors used the existing medical documentation for the analysis.
Another limitation of work is its outcome. Obtaining ROSC in prehospital conditions is not equivalent to patient survival. The first minutes after cardiac arrest are important for further prognosis. In some cases, however, the potentially reversible cause can only be resolved in the hospital. In the presented paper, the hospital documentation was not analyzed. A number of patients achieved ROSC, but a certain were transported during resuscitation. Moreover, not all emergency departments to which patients were transported were equipped with ACCD. Additionally, in the first phase of CPR, the compressions were performed manually. There was no data available on how long the compressions were provided manually before the ACCD and how long was no-flow time. Similarly, there are no data concerning the duration of the transport in patients in whom it was undertaken. Therefore, it is not possible to determine how long automatic compressions were performed during the entire period of resuscitation.
Conclusions
The use of ACCD may increase the number of prehospital ROSC and thus OHCA subjects admitted to hospital. Nonetheless, we found evidences suggesting that implementation of ACCD for two-paramedic teams may improve the quality of resuscitation. Moreover, it opens up the possibility of using modern resuscitation techniques like ECPR protocol, which may translate into survival. The authors believe that further intensive research should be undertaken to confirm the impact of ACCD on the quality of resuscitation in prehospital care.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.04.25). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The survey protocol has been approved by the Institutional Review Board of Poznan University of Medical Sciences (No: KB764/19).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gräsner JT, Wnent J, Herlitz J, et al. Survival after out-of-hospital cardiac arrest in Europe - results of the EuReCa TWO study. Resuscitation 2020;148:218-26. [Crossref] [PubMed]
- Stub D, Bernard S, Pellegrino V, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation 2015.88-94. [Crossref] [PubMed]
- Friess SH, Sutton RM, French B, et al. Hemodynamic directed CPR improves cerebral perfusion pressure and brain tissue oxygenation. Resuscitation 2014;85:1298-303. [Crossref] [PubMed]
- Rafi S, Tadie JM, Gacouin A, et al. Doppler sonography of cerebral blood flow for early prognostication after out-of-hospital cardiac arrest: DOTAC study. Resuscitation 2019;141:188-94. [Crossref] [PubMed]
- Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality. Circulation 2015;132:S414-35. [Crossref] [PubMed]
- McDonald CH, Heggie J, Jones CM, et al. Rescuer fatigue under the 2010 ERC guidelines, and its effect on cardiopulmonary resuscitation (CPR) performance. Emerg Med J 2013;30:623-7. [Crossref] [PubMed]
- Yuksen C, Prachanukool T, Aramvanitch K, et al. Is a mechanical-assist device better than manual chest compression? A randomized controlled trial. Open Access Emerg Med 2017;9:63-7. [Crossref] [PubMed]
- Gyory RA, Buchle SE, Rodgers D, et al. The Efficacy of LUCAS in Prehospital Cardiac Arrest Scenarios: A Crossover Mannequin Study. West J Emerg Med 2017;18:437-45. [Crossref] [PubMed]
- Gao C, Chen Y, Peng H, et al. Clinical evaluation of the AutoPulse automated chest compression device for out-of-hospital cardiac arrest in the northern district of Shanghai, China. Arch Med Sci 2016;12:563-70. [Crossref] [PubMed]
- Kim HT, Kim JG, Jang YS, et al. Comparison of in-hospital use of mechanical chest compression devices for out-of-hospital cardiac arrest patients: AUTOPULSE vs LUCAS. Medicine (Baltimore) 2019;98:e17881. [Crossref] [PubMed]
- Khan SU, Lone AN, Talluri S, et al. Efficacy and safety of mechanical versus manual compression in cardiac arrest - A Bayesian network meta-analysis. Resuscitation 2018;130:182-8. [Crossref] [PubMed]
- Bonnes JL, Brouer MA, Navarese EP, et al. Manual Cardiopulmonary Resuscitation Versus CPR Including a Mechanical Chest Compression Device in Out-of-Hospital Cardiac Arrest: A Comprehensive Meta-analysis From Randomized and Observational Studies. Ann Emerg Med 2016;67:349-60.e3. [Crossref] [PubMed]
- Tranberg T, Lassen JF, Kaltoft AK, et al. Quality of cardiopulmonary resuscitation in out-of-hospital cardiac arrest before and after introduction of a mechanical chest compression device, LUCAS-2; a prospective, observational study. Scand J Trauma Resusc Emerg Med 2015;23:37. [Crossref] [PubMed]
- Perkins GD, Lall R, Quinn T, et al. Mechanical versus manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled trial. Lancet 2015;385:947-55. [Crossref] [PubMed]
- Liu M, Shuai Z, Ai J, et al. Mechanical chest compression with LUCAS device does not improve clinical outcome in out-of-hospital cardiac arrest patients: A systematic review and meta-analysis. Medicine (Baltimore) 2019;98:e17550. [Crossref] [PubMed]
- Milling L, Astrup BS, Mikkelsen S. Prehospital cardiopulmonary resuscitation with manual or mechanical chest compression: A study of compression-induced injuries. Acta Anaesthesiol Scand 2019;63:789-95. [Crossref] [PubMed]
- Jasmeet S, Nolan JP, Bottiger BW, et al. European Resuscitation Concil Guidelines for Resuscitation 2015. Resuscitation 2015;95:100-47. [Crossref]
- Dabrowski M, Sip M, Dabrowska A, et al. It is impossible to follow the ERC algorithm in a two-paramedic ambulance team. Resuscitation 2017;118:43.
- Wroe PC, Clattenburg EJ, Gardner K, et al. Emergency department use of a mechanical chest compression device frequently causes unanticipated interruptions in cardiopulmonary resuscitation. Resuscitation 2018;133:e3-4. [Crossref] [PubMed]
- Marti J, Hulme C, Ferreira Z, et al. The cost-effectiveness of a mechanical compression device in out-of-hospital cardiac arrest. Resuscitation 2017;117:1-7. [Crossref] [PubMed]
- Damluji AA, Al-Damluji MS, Pomenti S, et al. Health Care Costs After Cardiac Arrest in the United States. Circ Arrhythm Electrophysiol 2018;11:e005689. [Crossref] [PubMed]
- Chen YS, Lin JW, Yu HY, et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet 2008;372:554-61. [Crossref] [PubMed]
- Kłosiewicz T, Puślecki M, Zieliński M, et al. The role of extracorporeal membrane oxygenation in patients after irreversible cardiac arrest as potential organ donors. Kardiochir Torakochirurgia Pol 2017;14:253-7. [Crossref] [PubMed]
- Sugarman L, Hedley D, Crowe S. Mechanical CPR in a child: can one size fit all? BMJ Case Rep 2017;2017.
- López J, Fernandez SN, Gonzalez R, et al. Comparison between manual and mechanical chest compressions during resuscitation in a pediatric animal model of asphyxial cardiac arrest. PLoS One 2017;12:e0188846. [Crossref] [PubMed]
- Ong MEH, Perkins GD, Cariou A. Out-of-hospital cardiac arrest: prehospital management. Lancet 2018;391:980-8. [Crossref] [PubMed]