
The arterial-ligation-alone method for identifying the intersegmental plane during thoracoscopic anatomic segmentectomy
Introduction
Globally, lung cancer has the highest morbidity and mortality among malignancies (1), and thus the early diagnosis and treatment of lung cancer are of utmost importance. With the popularization of low-dose computed tomography (LDCT), it is easier to diagnose early-stage non-small cell lung cancer (NSCLC) with the image manifestations of ground-glass nodules (GGNs) (2). Stemming from the prevalence of precision medicine, many retrospective studies have been conducted and show that segmentectomy produces the same oncological outcomes as lobectomy in early-stage NSCLC with the image manifestation of GGNs (3,4). Thoracoscopic anatomic segmentectomy is thus not only an alternative choice for lung cancer with poor cardiopulmonary reserve or other advanced complications, but can also be a radical surgery for T1a and selected T1b tumors (5,6).
Accurate identification of the intersegmental plane is one of the challenges in thoracoscopic anatomic segmentectomy. The bronchial method is used to identify the intersegmental plane by acting on the pulmonary segmental bronchi, which is technically feasible and fast. However, the identification of the intersegmental planes in this method is inaccurate, due to the presence of Kohn pores, Lambert canals and direct airway anastomosis (7). The vascular method includes the arterial-ligation-only method and intravenous injection of indocyanine green (ICG), which, while being more technically complicated than the bronchial method, is also more accurate. One study indicated that the intersegmental plane could be identified when the targeted artery alone was closed, without the need to close the bronchus and the vein (8). The author explained the theoretical basis from the perspective of gas exchange: oxygen in the alveoli enters the blood through the gas exchange, and after the ligation of the targeted pulmonary arteries, oxygen in the alveoli cannot be taken away through blood flow, In this case, the targeted pulmonary segment continues to be expanded, and the other pulmonary tissues collapse, which results in the boundary between the pulmonary segments the intersegmental plane being visible. The arterial-ligation-alone method is theoretically valid, but has not yet been validated or objectively evaluated in a large case series.
Our study, therefore, through comparison with the modified inflation-deflation method, confirmed that the arterial-ligation-alone method could effectively, accurately, and inexpensively identify the intersegmental plane, and is especially suitable for those patients whose veins or bronchi are difficult to anatomize.
Methods
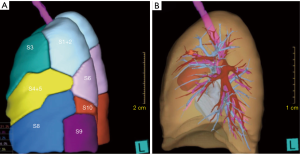
We retrospectively reviewed the records of 104 patients who were scheduled for thoracoscopic anatomic segmentectomy under the guidance of three-dimensional (3D) reconstruction between September 2017 and June 2019 by a team at the Department of Thoracic Surgery, Shandong Provincial Hospital Affiliated to Shandong University. The study was approved by ethics board of Shandong Provincial Hospital Affiliated to Shandong University (No. 2017-36) and informed consent was taken from all patients. The Hisense computer-assisted surgery system (HCAS) reconstructed the lung structure of each patient according to datum of chest thin high-resolution computed tomography examinations (layer thickness =1 mm). HCAS is a CT medical image preprocessing and segmentation software independently developed by Hisense. This system not only can divide the virtual lung into different segments according to the bronchi and distinguish them with different colors (Figure 1A), but can also present the segmental arteries, veins and bronchi separately (Figure 1B). Furthermore, HCAS supports the transparency of any pulmonary segment and rotation at any angle, which can effectively help the surgeon to estimate intersegmental planes and preoperative simulations.
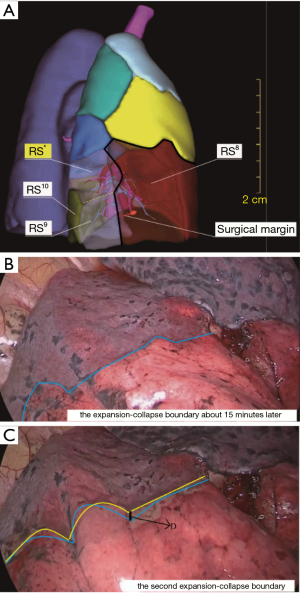
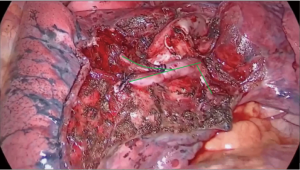
All patients underwent general anesthesia with double-lumen endotracheal intubation, while being positioned in the lateral decubitus position and being administered contralateral ventilation with pure oxygen. The surgical approach involved 2-hole access (the operating hole was about 3.0 cm in the fourth or fifth intercostal space, and the endoscopic hole was about 0.7 cm in the seventh intercostal space). According to preoperative 3D reconstruction (Figure 2A), we first dissociated targeted pulmonary vessels and bronchi and ligated the targeted pulmonary arteries. Next, bilateral pulmonary ventilation was used to fully inflate the entirety pulmonary lobes with pure oxygen (8,9). Contralateral-unilateral ventilation was performed once again, while, surgeons stopped all surgical procedures. After 5 minutes of contralateral-unilateral ventilation, the surface of the lung was observed every minute by thoracoscopy until the intersegmental plane was presented clearly as determined by 2 experienced chief thoracic surgeons who recorded the time spent waiting for the intersegmental planes as T1. The first intersegmental plane was marked by an electric coagulation hook. Next, the targeted segmental bronchi and veins were ligated, and the second intersegmental plane was obtained by using the inflation-deflation method as before (Figure 2B), the time spent waiting for the second intersegmental plane was recorded as T2. In order to evaluate the differences between the 2 intersegmental planes, we selected the margin with the most obvious difference between the 2 intersegmental planes to measure and recorded this as D (Figure 2C). According to the D value, we divided the differences between the 2 intersegmental planes into 3 levels: completely consistent, D ≤0.3 cm; basically consistent, 0.3 cm < D ≤0.5 cm; discrepant, D >0.5 cm. If there was a significant difference (D >0.5 cm) between the 2 intersegmental planes, we used an electric coagulation hook and staplers to excise the target segment along the second intersegmental plane (10,11). Some studies have shown that it is necessary to preserve intersegmental veins that run inside the intersegmental plane to mark the boundary of the pulmonary segments (12). Because the arterial-ligation-alone method does not involve the veins, the risk of damaging the intersegmental veins is dramatically reduced (Figure 3). For reference, we recorded a video of a segmentectomy of the right anterior basal segment by the arterial-ligation-alone method (Video 1).
Both the targeted segments where the lesion was located and the lymph nodes underwent intraoperative pathological examination. Thoracoscopic lobectomy was performed in patients if the intraoperative pathology of the lesion or any lymph node was invasive carcinoma. The thoracoscopic lobectomy also be performed if the surgical margin was insufficient or positive. When the intersegmental plane was still not apparent at T1 >30 minutes, or for some other reason that the intersegmental plane could not be seen, we would inform the patient's family and discussed the next surgical method: non-anatomic segmentectomy, lobectomy. In addition, due to the lack of relevant equipment in our study, the ICG method could not be used to identify the intersegmental plane. According to the preoperative 3D reconstruction, if the lesion was close to the intersegmental plane and the non-anatomic segmentectomy was more likely to lead to insufficient or positive surgical margin, thoracoscopic lobectomy was performed after obtaining the consent of the patient’s family. The family’s strong demand also leaded to thoracoscopic lobectomy. All patients were confirmed to have no air leakage or hemorrhagic spot before the chest was closed. Perioperative information was recorded for all patients, and all patients were followed up for 3 months after the operation.
Statistical analysis
Perioperative data were recorded for all cases. All P values were 2-sided 95% CI. For the study of the correlation between those factors and the time spent waiting for the appearance of the intersegmental plane, the univariable and multivariable correlation analysis was used. All statistical analyses were performed using SPSS 2.0 (IBM, SPSS Statistics, Chicago, IL, USA).
Results
A total of 104 patients were enrolled in the trial, and the arterial-ligation-alone method successfully obtained clear intersegmental planes in 99 (95.2%) of these patients. For the 5 (4.8%) remaining patients, in whom intersegmental planes were not obtained with the arterial-ligation-alone method, 2 patients had the intersegmental planes covered by serious anthracosis, and 3 patients had the T1 >30 minutes. Patient characteristics and differences between those who obtained intersegmental planes with the arterial-ligation-alone method and those who did not are shown in Table 1. For all patients, the lesions were located in the right upper lobe (24 cases, 23.1%), right lower lobe (25 cases, 24.0%) the left upper lobe (40 cases, 38.5%), and the left lower lobe (15 cases, 14.4%). No lesion was located in the right middle lobe. For the 99 patients who obtained clear intersegmental planes, the intraoperative pathological examination diagnosis revealed: benign lesion (3 cases, 3.0%), atypical adenomatous hyperplasia (4 cases, 4.0%), adenocarcinoma in situ (58 cases, 58.6%), minimally invasive adenocarcinoma (20 cases, 20.2%), and invasive adenocarcinoma (14 cases, 14.1%). None of the lymph nodes were metastatic, and the results of postoperative and intraoperative pathological diagnoses were completely consistent. The thoracoscopic lobectomy was performed on the 5 patients in whom the intersegmental planes were not obtained. In total 85 (81.7%) patients underwent thoracoscopic anatomic segmentectomy, 19 (18.3%) patients underwent thoracoscopic lobectomy finally.
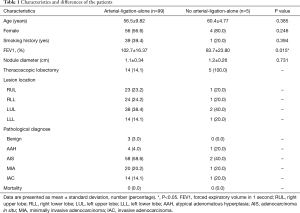
Full table
In this study, 99 (95.2%) patients had clear intersegmental planes clearly, and the consistency between 2 intersegmental planes are described in Table 2. We found that the maximum difference between the 2 intersegmental planes was no more than 0.5 cm, with most not being more than 0.3 cm, so we believe that the intersegmental plane obtained by the arterial-ligation-alone method was accurate. For the time spent waiting for the intersegmental plane to appear, the mean T1 was 13.6±2.7 minutes (range, 8–25 minutes), while the mean T2 was 13.0±2.6 minutes (range, 8–23 minutes) (P=0.100).

Full table
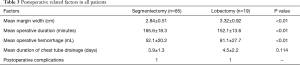
Table 3 shows the related postoperative factors in all patients. In the 85 patients who underwent thoracoscopic anatomic segmentectomy, the mean margin width was 2.84±0.51 cm; mean operative duration was 165.6±18.3 minutes, the mean operative hemorrhage was 52.1±20.2 mL, and the mean duration of chest tube drainage was 3.9±1.3 days. Postoperative complications related to operative procedures occurred in 2 cases.
Full table
Discussion
In 1995, the results of the Lung Cancer Study Group’s randomized trial comparing lobectomy with limited resection (including wedge resection and segmentectomy) suggested that limited resection was associated with higher death rate and locoregional recurrence rate (13). Lobectomy has since been considered the preferred procedure and standard of surgical treatment for patients with peripheral T1N0 NSCLC. With the popularization of health examination with LDCT, more and more lung nodules and GGNs are being detected. Thus, more rigorously designed clinical trials and studies comparing the short-term outcomes and long-term outcomes are being reported. Compared with wedge resection, segmentectomy is preferred because of its sufficient surgical margin, its evaluation of lymph nodes, and its superiority oncological outcomes (14,15). As a lung-sparing procedure, segmentectomy was shown to achieve equal short-term surgical results and long-term oncological outcomes compared with lobectomy (16,17). However, most of these studies were retrospective, and some results are contradictory (18) There are 2 on-going prospective randomized controlled clinical trials regarding segmentectomy, whose long-term outcome data are not yet available (19,20). The short-term outcomes, however, have confirmed the noninferiority of segmentectomy to lobectomy in terms of intraoperative and postoperative complications, with the exception that more air leakage was observed in the segmentectomy. Thoracoscopic anatomic segmentectomy will be a standard treatment in physically and functionally fit patients with clinical T1aN0 NSCLC if the superiority in postoperative pulmonary function and the non-inferiority in overall survival are confirmed.
For patients with surgical indications of thoracoscopic anatomic segmentectomy, preoperative planning to obtain sufficient resection margins is the most important step before surgery. Segmentectomy should achieve parenchymal resection margins ≥2 cm or ≥ the size of the nodule (12). Only sufficient resection margins can ensure the non-inferiority of segmentectomy to lobectomy in long-term prognosis. In all patients in our study who underwent thoracoscopic anatomic segmentectomy by the arterial-ligation-alone method, the resection margins were greater than 2 cm. Furthermore, the identification of the intersegmental plane is the key intraoperative procedure during segmentectomy. The intersegmental plane is directly related to sufficient resection margins and fewer postoperative complications, especially air leakage. Failure to accurately identify the intersegmental plane during segmentectomy may result in insufficient resection margins, the residue of the targeted segment or nodule, excessive resection of the parenchyma, iatrogenic injury of the intersegmental vein, and postoperative complications such as air leakage, atelectasis, hemoptysis, postoperative re-insertion of chest tube, etc. (19). In our study, the thoracoscopic lobectomy was performed on the 5 patients in whom the intersegmental planes were not obtained. Two patients had the intersegmental planes covered by serious anthracosis, unfortunately, the lesions in these 2 patients were too close to the intersegmental planes, and non-anatomic segmentectomy was likely to result in insufficient or positive surgical margins. Three patients because the targeted pulmonary lobes were still inflating when T1 >30 minutes, the ICG method could not be performed and other traditional bronchial methods we had tried were useless, meanwhile, patients’ families also tend to perform lobectomy, so thoracoscopic lobectomy was performed with the consent of the patient’s family. We guess that there are several possible cause of pulmonary lobe inflating, such as the contralateral-ventilation was incomplete, and the diffuse function of the affect lung was seriously impaired.
There are many methods available for the identification of the intersegmental plane. The intersegmental veins and natural intersegmental fissure can also be directly recognized as anatomical landmarks, and all methods are based on the precise dissection of the targeted artery, bronchus, and vein. Mistaken dissection of the segmental artery, bronchus, or vein will lead to a false intersegmental plane. Fortunately, 3D reconstruction aids significantly in the preoperative simulation and intraoperative navigation of thoracoscopic anatomic segmentectomy. Besides the anatomic variation and localization of pulmonary nodules, 3D reconstruction can simulate the intersegmental plane (21-23). After a comprehensive review of the relevant literature, we believe that the methods for identification of the intersegmental plane can currently be divided into two categories: the bronchial methods and the vascular methods. The bronchial methods include the preserved segment inflation method after targeted segmental bronchus is severed, the resected segment method using a butterfly needle (24) or via bronchofiberoptic jet (25), bronchial ligation with the slip-knot method (26,27), and transbronchial injection of dye (28). The vascular methods can also be called perfusion-based methods, meaning that the blood perfusion of the targeted segment should be severed beforehand, and includes the arterial-ligation-alone method or the intravenous injection of ICG (29). Each method has its own advantages and disadvantages. As we have mentioned, the bronchial method is technically easier and faster, but the intersegmental planes of this method are inaccurate, because of the presence of Kohn pores, Lambert canals, and direct airway anastomosis. The intravenous injection of ICG is time-saving, and only a few seconds elapse before the appearance of the intersegmental plane under near-infrared real-time fluorescence-merged imaging. Although the staining time may be prolonged by nearly 5 minutes through the temporary clamping of the pulmonary vein of the entire lobe at the risk of possible clot formation (30,31), this still is not practicable for image-guided parenchymal dissection, and involves expensive devices that are financially burdensome to patients. In contrast to the above-mentioned ICG method, the long duration of the expansion-collapse boundary via the arterial-ligation-alone method allows for image-guided dissection along the intersegmental plane not only on the visceral pleura but also within parenchyma. The main limitation of the arterial-ligation-alone method is the long time spent waiting for the appearance of the intersegmental plane. In the operative procedure of the traditional modified inflation-deflation methods, the targeted segmental arteries, bronchi, and intersegmental veins need to be cut before the administration of pure oxygen. In clinical practice, the dissection of targeted segmental arteries is much easier and safer than that of the bronchi and veins in most segments.
Based on an abundance of clinical data, we proved that the intersegmental plane via arterial-ligation-alone method is comparable to the traditional modified inflation-deflation method which is the globally accepted method for identifying the intersegmental plane, in other words, the arterial-ligation-alone method for identifying the intersegmental plane during thoracoscopic anatomic segmentectomy is feasible and effective. Although there was a statistically significant difference in the waiting time needed to visualize the intersegmental plane between the arterial-ligation-alone method and the traditional modified inflation-deflation method, it was negligible in practice. Above all, compared with the traditional modified inflation-deflation method, the arterial-ligation-alone method is helpful for avoiding the mistaken dissection of preserved bronchus and intersegmental veins in the subsequent procedures. Identifying the targeted bronchus and intersegmental veins can be done more easily and confidently when the correct intersegmental plane is dissected along with the expansion-collapse boundary. This is the most significant advantage of the arterial-ligation-alone method for thoracoscopic anatomical segmentectomy that we have developed.
As mentioned above, the main limitation of the traditional modified inflation-deflation method and our arterial-ligation-alone method is the extensive time spent waiting for the appearance of the intersegmental plane. In order to shorten the waiting time and to explore the possibility of a time-saving procedure, we conducted a univariate and multivariate analysis related to the waiting time. We think that the waiting time is related to the diffusion rate through the blood-air barrier of gas within the preserved segments, and some other gases with a faster diffusion rate than pure oxygen, such as nitrous oxide and carbon dioxide. However, the current study did not investigate this matter in depth.
There are several limitations to our method that should be addressed. First, temporary bilateral ventilation with pure oxygen is required to ensure the complete expansion of the affected lobe, followed by contralateral one-lung ventilation. The method requires cooperation with an anesthesiologist, which is not under the control of the surgeon. Second, in patients with severe chronic obstructive pulmonary disease and carbon deposition, the expansion-collapse boundary may not be clear. Third, this is a single-center, retrospective study with small sample size, and thus the results may be limited in their application to more complicated perioperative conditions.
Conclusions
Compared with the traditional modified inflation-deflation method, the arterial-ligation-alone method can also accurately identify the intersegmental plane during thoracoscopic anatomical segmentectomy precisely. Our method may simplify not only the operative procedures but also facilitate the identification of the targeted bronchus and intersegmental veins with dissection along the intersegmental plane, which can reduce unnecessary damage to the trachea and veins. In addition, whether the target bronchus is ligated has no effect on the intersegmental plane.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.03.83). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by ethics board of Shandong Provincial Hospital Affiliated to Shandong University (No. 2017-36) and informed consent was taken from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Okada M, Nishio W, Sakamoto T, et al. Correlation between computed tomographic findings, bronchioloalveolar carcinoma component, and biologic behavior of small-sized lung adenocarcinomas. J Thorac Cardiovasc Surg 2004;127:857-61. [Crossref] [PubMed]
- Yamashita S, Tokuishi K, Anami K, et al. Thoracoscopic segmentectomy for T1 classification of non-small cell lung cancer: a single center experience. Eur J Cardiothorac Surg 2012;42:83-8. [Crossref] [PubMed]
- Landreneau RJ, Normolle DP, Christie NA, et al. Recurrence and survival outcomes after anatomic segmentectomy versus lobectomy for clinical stage I non-small-cell lung cancer: a propensity-matched analysis. J Clin Oncol 2014;32:2449-55. [Crossref] [PubMed]
- Aokage K, Yoshida J, Hishida T, et al. Limited resection for early-stage non-small cell lung cancer as function-preserving radical surgery: a review. Jpn J Clin Oncol 2017;47:7-11. [Crossref] [PubMed]
- Sihoe AD, Van Schil P. Non-small cell lung cancer: when to offer sublobar resection. Lung Cancer 2014;86:115-20. [Crossref] [PubMed]
- Mun M, Nakao M, Matsuura Y, et al. Novel techniques for video-assisted thoracoscopic surgery segmentectomy. J Thorac Dis 2018;10:S1671-6. [Crossref] [PubMed]
- Iwata H, Shirahashi K, Mizuno Y, et al. Surgical technique of lung segmental resection with two intersegmental planes. Interact Cardiovasc Thorac Surg 2013;16:423-5. [Crossref] [PubMed]
- Endoh M, Oizumi H, Kato H, et al. How to demarcate intersegmental plane with resected-segments inflation method using the slip knot technique in thoracoscopic anatomic segmentectomy. J Vis Surg 2017;3:100. [Crossref] [PubMed]
- Matsumoto M, Shirahashi K, Yamamoto H, et al. Division of the intersegmental plane using electrocautery for segmentectomy in clinical stage I non-small cell lung cancer. J Thorac Dis 2018;10:S1215-21. [Crossref] [PubMed]
- Asakura K, Izumi Y, Kohno M, et al. Effect of cutting technique at the intersegmental plane during segmentectomy on expansion of the preserved segment: comparison between staplers and scissors in ex vivo pig lung. Eur J Cardiothorac Surg 2011;40:e34-8. [Crossref] [PubMed]
- Wu WB, Xia Y, Pan XL, et al. Three-dimensional navigation-guided thoracoscopic combined subsegmentectomy for intersegmental pulmonary nodules. Thorac Cancer 2019;10:41-6. [Crossref] [PubMed]
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [Crossref] [PubMed]
- Dai C, Shen J, Ren Y, et al. Choice of Surgical Procedure for Patients With Non-Small-Cell Lung Cancer ≤ 1 cm or > 1 to 2 cm Among Lobectomy, Segmentectomy, and Wedge Resection: A Population-Based Study. J Clin Oncol 2016;34:3175-82. [Crossref] [PubMed]
- Paoletti L, Pastis N, Denlinger C, et al. A decade of advances in treatment of early-stage lung cancer. Clin Chest Med 2011;32:827-38. [Crossref] [PubMed]
- Ren M, Meng Q, Zhou W, et al. Comparison of short-term effect of thoracoscopic segmentectomy and thoracoscopic lobectomy for the solitary pulmonary nodule and early-stage lung cancer. Onco Targets Ther 2014;7:1343-7. [PubMed]
- Lin Y, Zheng W, Zhu Y, et al. Comparison of treatment outcomes between single-port video-assisted thoracoscopic anatomic segmentectomy and lobectomy for non-small cell lung cancer of early-stage: a retrospective observational study. J Thorac Dis 2016;8:1290-6. [Crossref] [PubMed]
- Okada M, Mimae T, Tsutani Y, et al. Segmentectomy versus lobectomy for clinical stage IA lung adenocarcinoma. Ann Cardiothorac Surg 2014;3:153-9. [PubMed]
- Altorki NK, Wang X, Wigle D, et al. Perioperative mortality and morbidity after sublobar versus lobar resection for early-stage non-small-cell lung cancer: post-hoc analysis of an international, randomised, phase 3 trial (CALGB/Alliance 140503). Lancet Respir Med 2018;6:915-24. [Crossref] [PubMed]
- Nakamura K, Saji H, Nakajima R, et al. A phase III randomized trial of lobectomy versus limited resection for small-sized peripheral non-small cell lung cancer (JCOG0802/WJOG4607L). Jpn J Clin Oncol 2010;40:271-4. [Crossref] [PubMed]
- Iwano S, Yokoi K, Taniguchi T, et al. Planning of segmentectomy using three-dimensional computed tomography angiography with a virtual safety margin: technique and initial experience. Lung Cancer 2013;81:410-5. [Crossref] [PubMed]
- Oizumi H, Kanauchi N, Kato H, et al. Anatomic thoracoscopic pulmonary segmentectomy under 3-dimensional multidetector computed tomography simulation: a report of 52 consecutive cases. J Thorac Cardiovasc Surg 2011;141:678-82. [Crossref] [PubMed]
- Chan EG, Landreneau JR, Schuchert MJ, et al. Preoperative (3-dimensional) computed tomography lung reconstruction before anatomic segmentectomy or lobectomy for stage I non-small cell lung cancer. J Thorac Cardiovasc Surg 2015;150:523-8. [Crossref] [PubMed]
- Kamiyoshihara M, Kakegawa S, Ibe T, et al. Butterfly-needle video-assisted thoracoscopic segmentectomy: a retrospective review and technique in detail. Innovations 2009;4:326-30. [Crossref] [PubMed]
- Okada M, Mimura T, Ikegaki J, et al. A novel video-assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberoptic jet followed by cautery cutting. J Thorac Cardiovasc Surg 2007;133:753-8. [Crossref] [PubMed]
- Oizumi H, Kato H, Endoh M, et al. Slip knot bronchial ligation method for thoracoscopic lung segmentectomy. Ann Thorac Surg 2014;97:1456-8. [Crossref] [PubMed]
- Endoh M, Oizumi H, Kato H, et al. Determination of the intersegmental plane using the slip-knot method. J Thorac Dis 2018;10:S1222-8. [Crossref] [PubMed]
- Sekine Y, Ko E, Oishi H, et al. A simple and effective technique for identification of intersegmental planes by infrared thoracoscopy after transbronchial injection of indocyanine green. J Thorac Cardiovasc Surg 2012;143:1330-5. [Crossref] [PubMed]
- Andolfi M, Potenza R, Seguin-Givelet A, et al. Identification of the intersegmental plane during thoracoscopic segmentectomy: state of the art. Interact Cardiovasc Thorac Surg 2020;30:329-36. [Crossref] [PubMed]
- Ito A, Takao M, Shimamoto A, et al. Prolonged intravenous indocyanine green visualization by temporary pulmonary vein clamping: real-time intraoperative fluorescence image guide for thoracoscopic anatomical segmentectomy. Eur J Cardiothorac Surg 2017;52:1225-6. [Crossref] [PubMed]
- Misaki N, Chang S, Gotoh M, et al. A novel method for determining adjacent lung segments with infrared thoracoscopy. J Thorac Cardiovasc Surg 2009;138:613-8. [Crossref] [PubMed]


