Pneumomediastinum
Definition
Pneumomediastinum is the term which defines the presence of air in the mediastinum. It has also been described as mediastinal emphysema (1-3).
Classification
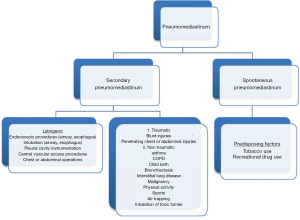
Spontaneous pneumomediastinum (SPM) (Figure 1) refers to the presence of air into the mediastinum in otherwise healthy subjects without an obvious causative factor such as an operation, air following a viscous perforation, presence of infection or trauma (1).
In cases with no mechanical ventilation applied or where no Valsalva maneuver is performed, air in the mediastinum is also considered as spontaneously appeared (4). This entity is observed in a significant percent of patients, in whom no factor to justify the origin of the pneumomediastinum can be identified (5).
The presence of air in the mediastinum is considered as secondary pneumomediastinum when a causative factor is identified (1-3).
Respiratory diseases may lead to pneumomediastinum, especially at periods of exacerbation with excessive coughing i.e., in asthma or respiratory infections (6-8). Usual inducing factors include asthma, interstitial lung disease, COPD, bronchiectasis, lung cysts, lung malignancy, excessive vomiting, and trauma (including iatrogenic).
Lately, the use of recreational drugs, such as cocaine, marijuana, methamphetamine, have been considered an additional factor that can cause pneumomediastinum (9,10). Other conditions leading to pneumomediastinum are the performance of vigorous Valsalva maneuver, childbirth, rapid ascent of scuba-divers, presence of foreign bodies in the airway with air trapping, anorexia neurosum, sporting activities and inhalation of toxic fumes (1).
However, It must be noted, that in several reports, the wider term SPM has been allowed even when a possible causative factor is identified (1).
The lack of such clarification has sparkled discussions amongst authors, as it is obvious that SPM has a more favorable outcome compared to secondary pneumomediastinum
Pathophysiology
The entity was firstly described by Laenek in 1827 (1-3). Hamman in 1939 described a post-partum patient with subcutaneous emphysema and pneumomediastinum, a case known in current times as Hamman’s syndrome (11). Macklin and Macklin in 1944 provided a sound explanation for pneumomediastinum, based on experiments conducted on cats: the increase of alveolar pressure causes them to rupture, therefore releasing air which in turn migrates through the peribronchial and perivascular sheaths to the mediastinum (12).
Another possible explanation for pneumomediastinum is the abnormal increase of pressure in the mediastinum, which like the pleural cavity is subjected to low and negative pressure, causing air to dissect in between the mediastinal structures, which support the mediastinal organs. A dramatic decrease in intravascular pressure also can create a relative pressure gradient in the perivascular spaces (1). The air may then dissect to the neck, upper abdomen or the skin via the loose alveolar fat tissue (subcutaneous emphysema) (7). Air can also pass the pleura resulting in pneumothorax or the peritoneum resulting in pneumoperitoneum (13).
Incidence
The pneumomediastinum is a rare entity, diagnosed in 1/44,500 of accident and emergency attendances or 1/100,000 of natural births, being more frequent in children (1/800-1/15,500) (7). Others, report an incidence of 1/25,000 in ages between 5-34 years (14). The majority of patients are males accounting for 76% of cases (1).
However, many authors believe that the occurrence of pneumomediastinum is more frequent than initially believed due to underdiagnosis (3,4), with many patients refraining from medical help. Infrequently the pathology may not be indentified on the chest radiograph and consequently related symptoms may be attributed to musculoskeletal pain or other insignificant causes (15).
Clinical presentation
It is generally agreed that pneumomediastinum usually occurs in young patients (2,5,7). One possible explanation is the fact that in young subjects the mediastinal tissues are loose and flaccid, whereas in the elderly group the planes and sheaths are fibrosed, making air migration more difficult to occur. Additionally, it is more prevalent in males (7/10 cases) (2,7) and in patients with pre existing asthma or other respiratory diseases (2,4,5). In many occasions the patients present with spontaneous pneumothorax (2,10). A tall, lean, male body habitus is generally considered as the most probable to be presented with pneumomediastinum; however, obese patients are not spared from this pathology (16).
The main presenting symptom is chest pain (kobashi), usually retrosternal, radiating to the neck or the back. It has been reported to be between 60-100% (1,5,6). The onset of the pain is sudden and acute, or follows exacerbations of underlying pathology such as asthma. Some authors suggest that when no obvious causative factor can be identified, clinicians should retain a high suspicion of pneumomediastinum, especially in cases of young adults presenting with acute chest pain (5). Other frequent symptoms include dyspnea (75%), coughing spells (80%), neck pain (36%), emesis or dysphagia, which however may be attributed to the possible underlying disease. In cases of SPM no complain is usually reported (21-51%) and no inducing factor may be found (5,6).
Subcutaneous emphysema can be detected in 70% of patients with diagnosed pneumomediastinum (6,7,9,10). Other presenting signs include rhinolalia (nasally sounding voice, which occurs because of dissection of air into the soft palate), hoarseness and neck swelling, depending on underlying pathology (7). Clinical evaluation may also identify tachycardia, tachypnea or anxiety with most patients however appearing generally well. A specific sign with an infrequent appearance (6,9,10) should be sought for, known as the Hamman’s sign; it is the presence of mediastinal crunch or click present on auscultation over the cardiac apex and the left sternal border synchronous with the heart beat (2).
Malignant pneumomediastinum is considered the accumulation of a significant amount of air in the mediastinum, causing vessel or tracheal obstruction and inducing respective symptoms and signs of tamponade and decreased venous return. Only few cases of this adverse appearance have been described and on this occurrence may be considered rare.
As mentioned earlier, pneumothorax might be the main presenting sign, with an incidence of 40% in some studies (10). Again, only few cases of tension pneumothorax have been reported.
Diagnosis
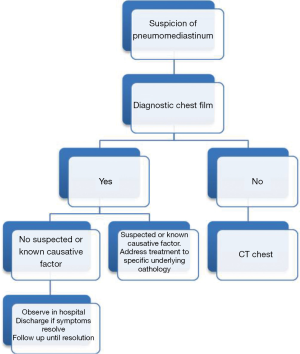
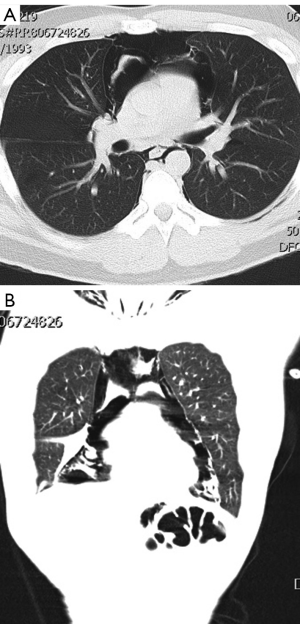
The diagnosis is usually established with a plain anterior chest film, showing lucent streaks, bubbles of air outlining mediastinal structures and visible mediastinal pleura (Figures 1-3). This investigation can yield a diagnosis in almost 90% of reported series (6,9,10). A lateral chest film is rarely required.

Recent series consider a chest CT scan as a routine diagnostic modality to assess the extent of the pneumomediastinum, (i.e., mild, moderate or severe) confirm the diagnosis in suspicious cases with an inconclusive chest X-ray and identify causative factors or pathologies (Figure 4). Additionally, it is needed in order to differentiate between pneumomediastinum and pneumopericardium (air within the pericardium and not on the prepericardial fat) which may have a less favorable course and might require treatment. The presence of a pneumothorax missed on a plain chest X-ray in cases with severe subcutaneous emphysema may also be confirmed with a CT scan.
Bronchoscopy, esophagoscopy or esophagography are not routinely required, in SPM; unless an underlying pathology is suspected or confirmed by presentation and past medical history. A detailed information of the patient’s previous health status and events is of paramount importance and cannot be emphasized enough.
Ultrasound of the mediastinum is lately applied in the accident and emergency department, in an effort to identify pneumomediastinum in cases of high urgency.
Many patterns of air outlining intrathoracic structures have been described in the literature, either based on chest X-ray or CT findings; thymic sail (elevation of thymus due to air, mainly seen in pediatric population), ring sign (caused by air surrounding the pulmonary artery or either of its main branches), double bronchial wall, continuous diaphragm sign, or air adjacent to hemidiaphragm or spine (1,15,17,18).
Inconclusive laboratory findings include rising white blood cells or C-reactive protein. ECG abnormalities have also been described without significant clinical importance (1,19).
Some authors, based on high suspicion and increased incidence of pulmonary disease, have suggested that pulmonary function tests should be obtained in spontaneous cases with no obvious exacerbating factors, especially in children (4).
Management
Pneumomediastinum is generally considered a benign entity of little clinical importance with good prognosis. After the diagnostic approach has excluded significant pathology, the pneumomediastinum treatment is directed towards symptom relief (1,20).
Following diagnosis patients are usually hospitalized for at least 24 hours merely for observation. Physical activity should be discouraged and bed rest must be ensured. Pain is controlled with analgesics, according to the Individual Unit’s protocols. Anti-anxiety drugs should also be administered. Coughing should be suppressed with relative antitussives. Administration of O2 may increase gas absorption by six fold and should therefore be considered (Figure 2).
Any underlying exacerbation of a pre-existing pathology such as asthma or COPD should be adequately attended. Most authors suggest that the control of pain and the stability of pneumomediastinum, as well as the elimination of complications, such as pneumothorax, should be considered as adequate for discharging such patients.
Rare sequllae of pneumomediastinum is the accumulation of a significant amount of air in the mediastinum in the majority of cases due to missed esophageal/pulmonary trauma which cause important air leak. In these cases, although rare, the simple pneumomediastinum may progress to a malignant one, leading to tamponade and airway compression. In such cases VATS or even thoracotomy may be essential for decompression (9). The development of pneumopericardium may very rarely cause tamponade which might requiresurgical evacuation by subxiphoid incision or VATS (5) (Figures 3-6).

Other complications of pneumomediastinum include extensive subcutaneous emphysema or pneumothorax, which usually require minor interventions, such as skin incisions and chest tube drainage. Air can also dissect in the retropharyngeal and retroperitoneal space causing discomfort and respiratory compromise. In rare situations air can dissect between the mediastinum and the upper spine causing pneumorrhachis (free air in the spinal canal) (21).
Outcome
Recurrences have been reported and therefore follow up is advisable. Spontaneous pneumodediastinum usually resolves by itself, but prolonged cases have also been reported (>2 months) (6). In general, few recurrences of pneumomediastinum have been reported enforcing its benign entity (22). In cases of recurrence, additional diagnostic evaluation should be conducted in an effort to identify any missed underlying pathologies, such as pulmonary or esophageal pathology. As stated before some authors have suggested performing i.e., lung function tests, in an effort to detect missed pulmonary underlying diseases.
It is suggested however, that due to the scarcity of recurrent incidents, no long term follow up is required, unless otherwise indicated (1,20).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Agut A, Talavera J, Buendia A, et al. Imaging diagnosis-spontaneous pneumomediastinum secondary to primary pulmonary pathology in a dalmatian dog. Vet Radiol Ultrasound 2014. [Epub ahead of print]. [PubMed]
- Kobashi Y, Okimoto N, Matsushima T, et al. Comparative study of mediastinal emphysema as determined by etiology. Intern Med 2002;41:277-82. [PubMed]
- Sahni S, Verma S, Grullon J, et al. Spontaneous pneumomediastinum: time for consensus. N Am J Med Sci 2013;5:460-4. [PubMed]
- Chiu CY, Wong KS, Yao TC, et al. Asthmatic versus non-asthmatic spontaneous pneumomediastinum in children. Asian Pac J Allergy Immunol 2005;23:19-22. [PubMed]
- Macia I, Moya J, Ramos R, et al. Spontaneous pneumomediastinum: 41 cases. Eur J Cardiothorac Surg 2007;31:1110-4. [PubMed]
- Caceres M, Ali SZ, Braud R, et al. Spontaneous pneumomediastinum: a comparative study and review of the literature. Ann Thorac Surg 2008;86:962-6. [PubMed]
- Russo A, Del Vecchio C, Zaottini A, et al. Role of emergency thoracic ultrasonography in spontaneous pneumomediastinum. Two case report. G Chir 2012;33:285-96. [PubMed]
- Chu CM, Leung YY, Hui JY, et al. Spontaneous pneumomediastinum in patients with severe acute respiratory syndrome. Eur Respir J 2004;23:802-4. [PubMed]
- Perna V, Vilà E, Guelbenzu JJ, et al. Pneumomediastinum: is this really a benign entity? When it can be considered as spontaneous? Our experience in 47 adult patients. Eur J Cardiothorac Surg 2010;37:573-5. [PubMed]
- Iyer VN, Joshi AY, Ryu JH. Spontaneous pneumomediastinum: analysis of 62 consecutive adult patients. Mayo Clin Proc 2009;84:417-21. [PubMed]
- Hamman L. Spontaneous mediastinal emphysema. Bull Johns Hopkins Hosp 1939;64:1-21.
- Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: an interpretation of the clinical literature in the light of laboratory experiment. Medicine 1944;23:281-358.
- Pooyan P, Puruckherr M, Summers JA, et al. Pneumomediastinum, pneumopericardium, and epidural pneumatosis in DKA. J Diabetes Complications 2004;18:242-7. [PubMed]
- Jougon JB, Ballester M, Delcambre F, et al. Assessment of spontaneous pneumomediastinum: experience with 12 patients. Ann Thorac Surg 2003;75:1711-4. [PubMed]
- Kaneki T, Kubo K, Kawashima A, et al. Spontaneous pneumomediastinum in 33 patients: yield of chest computed tomography for the diagnosis of the mild type. Respiration 2000;67:408-11. [PubMed]
- Mondello B, Pavia R, Ruggeri P, et al. Spontaneous pneumomediastinum: experience in 18 adult patients. Lung 2007;185:9-14. [PubMed]
- Moseley JE. Loculated pneumomediastinum in the newborn. A thymic "spinnaker sail" sign. Radiology 1960;75:788-90. [PubMed]
- Hammond DI. The "ring-around-the-artery" sign in pneumomediastinum. J Can Assoc Radiol 1984;35:88-9. [PubMed]
- Takada K, Matsumoto S, Hiramatsu T, et al. Management of spontaneous pneumomediastinum based on clinical experience of 25 cases. Respir Med 2008;102:1329-34. [PubMed]
- Koullias GJ, Korkolis DP, Wang XJ, et al. Current assessment and management of spontaneous pneumomediastinum: experience in 24 adult patients. Eur J Cardiothorac Surg 2004;25:852-5. [PubMed]
- Al-Mufarrej F, Gharagozloo F, Tempesta B, et al. Spontaneous cervicothoracolumbar pneumorrhachis, pneumomediastinum and pneumoperitoneum. Clin Respir J 2009;3:239-43. [PubMed]
- Gerazounis M, Athanassiadi K, Kalantzi N, et al. Spontaneous pneumomediastinum: a rare benign entity. J Thorac Cardiovasc Surg 2003;126:774-6. [PubMed]