
Conversion method to manage surgical difficulties in non-intubated uniportal video-assisted thoracic surgery for major lung resection: simple thoracotomy without intubation
Introduction
Video-assisted thoracic surgery (VATS) has been developed to minimize surgery-inflicted tissue injury, thereby improving patient outcomes (1). Theoretically, combining VATS with the non-intubated thoracic surgical (NITS) approach, especially when spontaneous breathing is maintained throughout, induces the least potential stress on patients; hence, it could be most beneficial for patients undergoing lung resection (2). The VATS-NITS method for major lung resections is used mainly in dedicated centers, and its widespread use is mainly inhibited by a doubt: “Is this procedure safe enough for patients, and how could we perform a quick conversion if needed?” Currently, in the case of unexpected complications during NITS, the recommended solution is the conversion to open thoracotomy that is preceded by muscle relaxation, the insertion of a double-lumen endotracheal tube and controlled mechanical ventilation has been the gold standard and routine for several decades (3,4). Complications during NITS may be due to anesthesiologic and surgical reasons alike. In cases of surgical complications, which are mainly technical difficulties, intubation and conversion to thoracotomy is the recommended method (4), but intubation can sometimes be very difficult and even planned endotracheal intubation with a double-lumen tube has a significant complication rate (5).
Here we report our practice of managing surgical difficulties during uniportal VATS-NITS major lung resection.
Methods
Patients
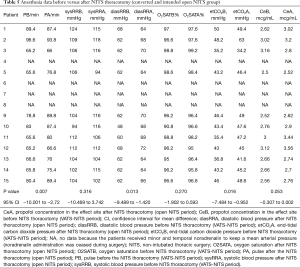
Between January 26, 2017 and November 30, 2018, 166 thoracic surgical procedures were performed using the uniportal VATS-NITS method. Patient characteristics are summarized in Table 1. Six of the 166 patients required intubation during surgery: 1 had serious diaphragm and mediastinal movements, 2 had blood in the airways (anesthesiologic indications for conversion), and 3 had severe adhesions (surgical indication for conversion) requiring isolation with a double-lumen tube. The conversion rate to intubation with anesthesiologic indication and the following thoracotomy was 1.8% (3/166). In 160 cases, the NITS procedure was completed. In 145 NITS-VATS cases, the uniportal procedure was performed; however, 15 cases required conversion to open NITS (NITS with thoracotomy). The characteristics of these 15 open NITS patients are shown in Tables 2 and 3. For each patient, the NITS procedure was explained and the risks were detailed. If the patients agreed with this method, written informed consent was obtained from all patients.
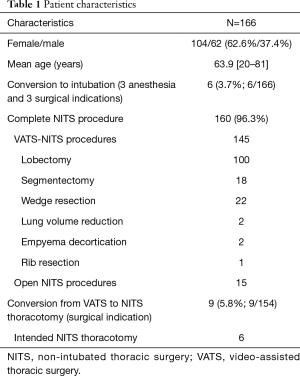
Full table
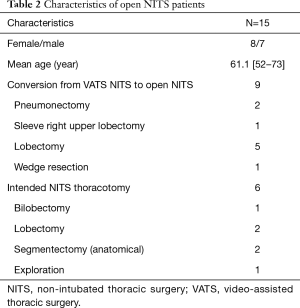
Full table
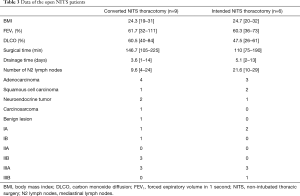
Full table
Surgical selection criteria for VATS-NITS procedure
Because the surgical technique of the VATS-NITS procedure is the same as in intubated cases, the indications are also similar. According to the recommendations of a recent consensus meeting, patients mainly with lung cancer less than 7 cm, N0 and N1 cases are scheduled for VATS in our practice as well (1). Regarding the NITS itself, patients who are otherwise planned to undergo the VATS procedure with a body mass index (BMI) less than 30 without other exclusion criterias are indicated for NITS operation (Table 4).
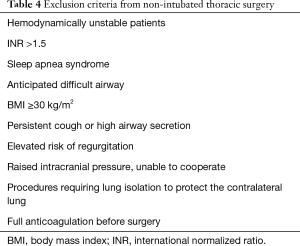
Full table
Surgical procedure
We performed the same VATS uniportal method during the NITS procedures as was mentioned in the literature (6); in our uniportal practice, we follow the recommendation and work of Gonzales-Rivas (7,8). The “uniportal” terminology is debated in the literature due to the size of the incision (9).
Due to the NITS, at the incision site in the 5th intercostal space in the middle axillary line, 2% lidocaine (5 mg/kg) skin and subcutaneous infiltration is administered. A few minutes later, the incision is performed. The size of the utility incision depends on the patient’s BMI. If the chest wall is 3–6 cm wide due to the fat, the incision is about 6 cm, but in a thin patient, the incision can be 4 cm. Thus, incision size is unrelated to uniportal VATS if a single incision is made without rib retraction. After entering the thoracic cavity, the lung gradually becomes atelectatic. A plastic ring retractor is inserted to hold the soft tissue. The complete atelectasis develops in 7–10 minutes, but during this time an intercostal nerve blockade is given with 0.5% bupivacaine between the 2nd and 5th intercostal nerves and near the vagus nerve (right side in the upper mediastinum; left side in the aortopulmonary window). The total amount of bupivacaine is 0.5 mL/kg. We usually administer 4–5 mL 0.5% bupivacaine near the 2nd to 5th intercostal nerves. To deliver local infiltration close to the vagus nerve, we administer 0.5% bupivacaine 3–5 mL with a long or butterfly needle. The left side the vagus blockade is a little more difficult. In the aortopulmonary window, the pleura is elevated a little and the needle is inserted under the elevated pleura into the fatty tissue close to the vagus nerve, and 3–5 mL bupivacaine is injected toward the vagus nerve. This is not painful, and patients do not react during this maneuver. To the vagus nerve blockade, the lung must be touched gently because it is very sensitive to manipulation. We just lift up the lung with an instrument or sponge to visualize the vagus. At 2–3 minutes after the vagus blockade, the lung can be held with the ring forceps without coughing. After this point, the manipulations are the same as in an intubated VATS surgery. There was no cough at the time of the manipulation near or in the bronchus.
Conversion from VATS NITS to open NITS
At the beginning of our NITS practice, when any kind of complications or difficulties occurred during the resection that were difficult to manage using the VATS-NITS approach, the anesthesiologist was asked to intubate the trachea with a double-lumen tube and a thoracotomy was performed. This was done in six cases.
In one case, the reason for conversion was a metastatic lymph node around the right upper lobe; we asked the anesthesiologist to intubate the patient. Because the intubation was a little more difficult and longer than usual, we simply extended the skin incision and used a rib retractor to enlarge the wound to provide a better view to the thoracic cavity. Because the patient remained stable and there were no signs of anesthetic complications, we gradually performed a regular axillary thoracotomy and a right upper sleeve lobectomy without complications.
After this operation, we changed our practice: In case of any surgical difficulties during the VATS-NITS surgery that were not manageable through the VATS method and the patient was stable, we disregarded endotracheal intubation and proceeded with a regular axillary thoracotomy and resection as usual. At the end of the surgery, the thoracotomy is closed, a chest tube is inserted via another incision, and a serratus cannula is inserted for postoperative pain management.
Conversion to open NITS was required in 9 cases due to oncological reasons (lymph node infiltration) in 4, bleeding in 2, technical difficulty to the sleeve in 1, extended adhesion in 1, and palpation difficulty in 1. In cases of major bleeding, the judgment and management of the conversion is the same as in intubated VATS. In our practice, if we cannot control the bleeding with compression of the distal artery or it is on the main pulmonary artery (even if it can be control with compression), a thoracotomy is indicated. As the bleeding begins, if the patient is stable, there is no indication for intubation. Theoretically, if the situation was catastrophic (fortunately none of our cases), the thorax would be opened immediately, the bleeding controlled with a clamp or by hand, and intubation requested of the anesthesiologist with the patient in a lateral position: it would be performed via a laryngeal mask with a single-lumen tube and bronchial blocker under fiberoptic guidance.
However, we must stress that the real-life threatening situation is not the major bleeding from a large vessel; rather, it is bleeding into the airway. This is an immediately indication for intubation. In this situation, the bleeding volume is not serious, so we have time to turn the patient and intubate them normally. Using the LMA (LMA; Ambu Aura-i laryngeal mask), we can completely control the airway.
Intended open NITS
After the excellent results of the first 4 conversion cases from VATS-NITS to open NITS, in 6 patients with a low forced expiratory volume in 1 second [60.3% (36–73%)] and carbon monoxide diffusion [47.5% (26–61%)], we decided to perform a direct/planned/intended open NITS surgery after receiving patient permission. We performed intended axillary thoracotomies after VATS-NITS exploration of the thorax and infiltration of the intercostal spaces and the vagus nerve. Using this method, normal resections were possible. The chest was closed over a drain, and a serratus cannula was inserted for pain management. The serratus anterior plane (SAP) block with cannula, which can be inserted intraoperatively or under ultrasonography guidance, provides prolonged anesthesia of the hemithorax with numbness over the thoracic area supplied by the lateral cutaneous branches of the T2–T9 spinal nerves. This can provide adequate pain relief effect after a thoracotomy. It is filled intraoperatively with bupivacaine (0.5 mg/mL) and followed by a continuous infusion of 5 mL/h for the first 36 hours (10). Patient data are shown in Tables 2 and 3.
Anesthesiology
The exclusion criteria of NITS are summarized in Table 4. In the operating room, in addition to standard monitoring (ECG, O2 saturation, non-invasive blood pressure), depth of anesthesia monitoring by bispectral index (BIS; Medtronic Vista) and invasive blood pressure measurements are performed. Midazolam and fentanyl are administered prior to the surgery. Anesthesia is induced and maintained with propofol administrated via target-controlled infusion titrated to keep the BIS at 40–60 according to published recommendations (5). After adequate depth of anesthesia is achieved, a laryngeal mask is inserted for airway maintenance. Spontaneous breathing is also maintained throughout and ventilation is monitored with capnography. Oxygen and air mixture are supplemented via a T-piece and FiO2 is titrated to keep the SpO2 at above 92%.
Anesthetic indications for conversion
The most frequently occurring indications for intubation are the following:
- Hypoxemia: In case of SpO2 <92% or PaO2 <60 mmHg on 100% O2, the operated (non-dependent) lung is reinflated. If this procedure cannot correct the hypoxemia, then endotracheal intubation is performed.
- Hypercapnia: If PaCO2 >75 mmHg or pH <7.15, the operated lung is reinflated to eliminate CO2: patients breathe spontaneously via LMA and we adjust the low PEEP and pressure support on the circle and the lung reinflates due to this positive pressure. If it fails, conversion is necessary.
- Bleeding in the airways: At the first sign of blood in the airway, immediate intubation is required. The airways are always checked via LMA with a fiber optic bronchoscope before and after the resection. If there is any sign of blood or other secretions, it must be suctioned prior to the reinflation.
Method of conversion from NITS to intubation
At the start of our NITS experience, the correct procedure for intubation was as follows: rotation of the operation table to backward as we could, intubation of the trachea with a single-lumen tube, and placement of a bronchial blocker under fiber optic guidance or the insertion of a double-lumen tube. After we had more experience with patient tolerability and difficulties with urgent intubations in the lateral decubitus position, our protocols changed. Currently, if conversion to intubation is necessary, an urgent chest tube is inserted, the wound is covered with a temporary bandage, and the patient is returned to the supine position. In this supine position, intubation is a simple procedure. The time from the decision of the intubation to the supine position is generally less than 2 minutes.
Method of anesthesiology in open NITS cases
If the patient is stable and there is no indication for intubation but the surgical difficulties cannot be managed with the VATS-NITS method, a thoracotomy can be done in NITS circumstances. For the thoracotomy, we do not change the anesthesia and no additional drugs are necessary. Generally, with the same drug administration as in the pre-thoracotomy period, we can keep the patient parameters in the normal range. We follow the ERAS (enhanced recovery after surgery) principles and try to avoid TEA (thoracic epidural anaesthesia) and its possibly hard sympatholytic effect. Therefore, we use TPB (thoracic paravertebral blockade) and the new SAP block. This block is in the new ERAS guidelines with TPB and might be useful after thoracotomies. Our experience absolutely confirmed this theory.
We use the same protocol for intended open cases. In 4 of 15 cases, some noradrenaline was necessary for a short period of time. The indication for the administration of noradrenaline is the low systolic blood pressure or the low mean arterial pressure (MAP). According to our practice, the MAP must be higher than 60 mmHg or the systolic blood pressure higher than 90 mmHg to ensure adequate organ and tissue filling pressure and blood flow. This practice is similar in intubated and non-intubated patients (Table 5).
Full table
Statistical methods
Data of the pulse, systolic and diastolic blood pressure, sat O2, end-tidal carbon dioxide pressure (etCO2), and propofol concentration in the effect were collected from the anesthesiologic documentation. Two-way repeated measures analysis of variance was used to compare the means of the above noted variables before versus after thoracotomy during the NITS open surgery. The 95% CIs for the mean differences were calculated. Values of P<0.05 were considered statistically significant. The analysis was performed using IBM SPSS 24 statistical software.
Results
Among the open NITS cases, there were almost identical numbers of female and male patients; in contrast, among the VATS-NITS cases, there were almost twice as many female as male patients (Tables 1 and 2). There were no cases of perioperative mortality.
Anesthesiology
Regarding the 15 open NITS cases, there were no significant differences in systolic blood pressure (P=0.316; 95% CI, −10.469 to 3.742), satO2% (P=0.27; 95% CI, −1.902 to 0.593), or propofol concentration in the effect site (P=0.053; 95% CI, −0.307 to 0.002) but there were significant differences in pulse (P=0.007; 95% CI, −10.001 to −2.72), diastolic blood pressure (P=0.013; 95% CI, −9.489 to −1.420) and etCO2 (P=0.016; 95% CI, −7.484 to −0.952) during the NITS surgery or before and after the thoracotomy. Despite these statistical findings, due to the open NITS procedure use in 11 patients, it was not necessary to change the anesthesiologic treatment after thoracotomy. In 4 patients, noradrenaline administration was necessary to maintain adequate MAP, but it was ceased toward the end of the surgery. Two patients after pneumonectomy were admitted to the intensive care for observation, but the other 13 were transferred from the recovery room to the ward.
Surgery
According to our preliminary experience, all parts of a lung resection including lymphadenectomy can be performed via open NITS just as with the conventional intubated way without complications (Table 3). We had no R1–2 resections. The operative time was a little longer in the converted cases because of the exploration until conversion (Table 3). The majority of the resections were lobectomies, and in the patients with a BMI ≤30, the mediastinum and the diaphragm movement did not disturb the resection. The only new experience was the softness of the airways without the endotracheal tube, which requires special attention during mediastinal lymphadenectomy. Most of our patients had advanced lung cancer with lymph node metastasis. There were 3 patients with a prolonged air leak longer than 5 days (20%; 3/15), and the mean drainage time in the 15 open NITS cases was 4.2 days (range, 1–14). The overall conversion rate with surgical indications (3 to intubation and thoracotomy; 9 to open NITS) was 7.5% (12/160). One patient who underwent surgery due to a serious hemoptysis for which a lower bilobectomy was done died 25 days postoperative of cardiac insufficiency. His preoperative lung functions were very limited as follows: forced expiratory volume in 1 second (26%), carbon monoxide diffusing capacity (26%), and VO2max (13.9 mL/kg/min). His postoperative period was uneventful, and he was discharged on postoperative day 7 to rehabilitation.
Discussion
The most criticized part of the NITS procedure is the “unsafe” airway. Although the conversion from NITS to an intubated method depends on anesthesiologic and surgical indications, it is recommended in any difficulties during the NITS thoracic surgery that the patient be intubated and the surgical procedure continue in that manner (11). With our experiences and practice, we recommended distinguishing between anesthesiologic and surgical indications for the conversion because the different problems should be managed differently.
In a review article from Mineo, the overall conversion rate to general anesthesia was 0–9%, but it did not detail the rates of surgical versus anesthesiologic indications (11). The conversion rate of the Liua study was 7%, which could be reduced with more experience, but this article did not distinguish between anesthesiologic and surgical indications for conversion; rather, intubation was required for both (5).
Intubation in the lateral decubitus position can be difficult. In our practice, in case of conversion with anesthesiologic indication, we quickly cover the wound over a chest tube and turn the patient to the supine position, in which intubation is very easy, taking less than 2 minutes. In difficult intubation cases, we do not perform intubation in the lateral position. Other authors reported inserting a chest drainage tube during the intubation to prevent tension pneumothorax, but they did not turn the patients to the supine position first (11,12).
In our practice, the overall surgical indication for conversion was 7.5%, which is very similar to the data of other centers; most frequently, serious adhesion, mediastinal movement, and bleeding cause the conversion (11). At the beginning of our NITS procedure, we intubated for any complication, and surgical reasons caused 1.8% (3/166) of cases. Later we realized that in surgical difficulties, when the patient is stable, intubation is not necessary from the anesthesiologic point of view and a thoracotomy and all resections can be performed without it.
Although there were statistically significant differences between the data of pulse, diastolic blood pressure, and etCO2 before versus after NITS thoracotomy, the changes were not dramatic and did not require any serious modification in the drug administration in 11 patients. Confidence intervals for the differences clearly present that, despite statistical significance, there is no clinical relevance of the differences. In 4 patients, to maintain MAP, minor and temporal noradrenalin administration was necessary but could be ceased during surgery. This shows that, in adequate intercostal and vagus nerve blockade, the thoracotomy procedure itself does not require any modification in the NITS anesthesiology. In the literature, we did not find any articles analyzing long-term experiences or presenting metanalysis about open NITS procedures (5,11,12).
An open NITS surgery is feasible for any minor and major lung resection. As we demonstrated here, the pneumonectomy and even a sleeve resection can be performed under open NITS, but attention must be paid to prevent blood from entering the airway.
The other part of the oncological principles is lymph node management. As we demonstrated, a good number of mediastinal lymph nodes (N2) can be removed during open NITS (9.6 and 21.6) versus VATS-NITS in other centers (all the lymph nodes N1+N2: 17.2) (5). In a review article of NITS metastasectomy from Migliore (13) it is mentioned, that the main criticisms against the NITS is the difficulty of the mediastinal lymphadenectomy. In our practice, we did not find any difficulties in performing lymphadenectomy. The only technical difference from intubated cases is that in open NITS patients, the airways are soft because of the absence of the intratracheal tube, so preparation around this soft airway must be done carefully. Using our technique, no cases of cough or airway injury occurred during the peribronchial manipulation.
In conclusion, the anesthesiologic and surgical indications in cases of conversion in VATS-NITS should be strictly distinguished because of the different management approaches to these problems. The anesthesiologic difficulties required intubation, but if the patient’s oxygenation and circulation are normal, intubation is not necessary to manage surgical difficulties and a simple thoracotomy can be performed. Using open NITS thoracotomy, every step of a major lung resection can be completed without additional risk for patients. Although we worked out a safety way for conversion in NITS procedures, we can’t predict if the NITS or awake surgery for major lung resection will become more common in the future or not. Currently mainly the technical questions of the procedure are discussed in the literature, and only few studies are published with physiological and the positive immune effect of the NITS (14). As a safe conversion practice was presented and the long term physiological and cancer-related effect of the NITS are proved, the current judgment of the non-intubated thoracic procedures will be changed.
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing.
Funding: None.
Footnote
Conflicts of Interest: Al authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-19-3830). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The authors confirm that the research adhered to the conditions of the ethics committee of the institutions and confirm the provisions of the Helsinki Declaration. Patient data were retrieved retrospectively from our medical record system (Medsolution) and the patients’ personal data were secured. Ethical permission number: 111/2017-SZTE.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yana TD, Caoa C, D’amicoc TA, et al. Video-assisted thoracoscopic surgery lobectomy at 20 years. Eur J Cardiothorac Surg 2014;45:633-9. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Single-port thoracoscopic lobectomy in a nonintubated patient: the least invasive procedure for major lung resection? Interact Cardiovasc Thorac Surg 2014;19:552-5. [Crossref] [PubMed]
- Hung M-H, Hsu H-H, Cheng Y-J, et al. Nonintubated thoracoscopic surgery: state of the art and future directions. J Thorac Dis 2014;6:2-9. [PubMed]
- Tacconi F, Pompeo E. Non-intubated video-assisted thoracic surgery: where does evidence stand? J Thorac Dis 2016;8:S364-75. [Crossref] [PubMed]
- Liu J, Cui F, Pompeo E, et al. The impact of non-intubated versus intubated anaesthesia on early outcomes of video-assisted thoracoscopic anatomical resection in non-small-cell lung cancer: a propensity score matching analysis. Eur J Cardiothorac Surg 2016;50:920-5. [Crossref] [PubMed]
- Bertolaccini L, Batirel H, Brunelli A, et al. Uniportal video-assisted thoracic surgery lobectomy: a consensus report from the Uniportal VATS Interest Group (UVIG) of the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019;56:224-9. [Crossref] [PubMed]
- Diego Gonzalez-Rivas. Uniportal thoracoscopic surgery: from medical thoracoscopy to non-intubated uniportal video-assisted major pulmonary resections Ann Cardiothorac Surg 2016;5:85-91. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Migliore M, Hirai K. Uniportal VATS: Comment on the consensus report from the uniportal VATS interest group (UVIG) of the European Society of Thoracic Surgeons. Eur J Cardiothorac Surg 2020;57:612. [PubMed]
- Blanco R, Parras T, McDonnell JG, et al. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia 2013;68:1107-13. [Crossref] [PubMed]
- Mineo TC, Tacconi F. From “awake” to “monitored anesthesia care” thoracic surgery: A 15 year evolution. Thorac Cancer 2014;5:1-13. [Crossref] [PubMed]
- Hung M-H, Hsu H-H, Chan K-C, et al. Non-intubated thoracoscopic surgery using internal intercostal nerve block, vagal block and targeted sedation. Eur J Cardiothorac Surg 2014;46:620-5. [Crossref] [PubMed]
- Migliore M, Borrata F, Nardini M, et al. Systematic review on awake surgery for lung metastases. Video-assist Thorac Surg 2017;2:70-4. [Crossref]
- Mineo TC, Ambrogi V. Immune effects after uniportal nonintubated video-thoracoscopic operations. Video-assist Thorac Surg 2018;3:4-10. [Crossref]


