The link between mold sensitivity and asthma severity in a cohort of northern Chinese patients
Introduction
Bronchial asthma is a chronic inflammatory disorder of the airways whose prevalence has increased considerably over the past 20 years (1,2). While most cases of asthma can be controlled with anti-inflammatory and bronchodilator therapy, a minority of patients suffer from severe airway inflammation and airflow obstruction; a condition that leads to recurring exacerbations and multiple hospital admissions (3,4). To date, the factors that contribute to more severe cases of asthma are not fully understood.
Recent evidence indicates that sensitivity to mold allergens is related to asthma severity (5,6). A European community respiratory health survey of 1,132 adults with asthma found that sensitivity to the airborne molds alternaria alternata and Cladosporium herbarum are significant risk factors for severe asthma (7). Several small case control studies have suggested links between mold sensitivity and acute asthma attacks requiring hospitalization (8,9), admission to intensive care for asthma (10), reduced forced expiratory volume in one second (FEV1) (11) and asthma mortality (12). However, the relationship between mold sensitivity and asthma severity has been poorly characterized in Chinese adult populations. Here, we describe a cross sectional investigation of the relationship between asthma severity and airborne mold sensitivity in a cohort of northern Chinese patients.
Methods
Subjects and selection criteria
Ninety-three consecutive outpatients with asthma from a teaching hospital of Peking University were enrolled between March, 2010 and September, 2011. The inclusion criteria for enrollment included a minimum age of 18 years, nonsmoking status, and a history of asthma as confirmed by bronchodilator reversibility or bronchial hyper-responsiveness [following Chinese diagnostic criteria (13)]. Pregnant and lactating women, patients with history of allergic shock and patients diagnosed as allergic bronchopulmonary aspergillosis (ABPA) were excluded from this study. All procedures were approved by the committee on human research at Peking University People’s Hospital. All patients provided written informed consent.
Skin prick allergy tests
Skin prick tests were performed in all patients with five aeroallergens (Allergopharma, Reinbek, Germany) including house dust mites, powder dust mites, weeds, polyvalent molds (Alternaria tenuis, Botrytis cinerea, Cladosporium herbarum, Curvularia lunata, Neurospora sitophila, Helminthosporium halodes), and Aspergillus fumigatus. No exacerbations or respiratory infection were reported for four weeks prior to the skin tests, and neither antihistamines nor systemic corticosteroids were used for two weeks prior to undergoing the skin tests. Skin prick test was performed with 0.01 mL of the indicated allergens (1:500 weight: volume) along with negative control (0.9% sodium chloride solution) and positive control (histamine dihydrochloride, 1 mg/mL) solutions. Skin test results were analyzed according to previously described methods (14).
Assessment of clinical features
All patients were asked to respond to an asthma questionnaire that included general medical history, the number of acute attacks and hospitalizations, and oral corticosteroid use. The questionnaire also included the asthma control test (ACT) (http://www.asthmacontrol.com) to assess clinical control of asthma. Each participant underwent clinical examination with special attention to the respiratory system. Blood was drawn for measurements of absolute eosinophil count (AEC) and serum IgE (sIgE) levels. The total sIgE levels were detected using the ImmunoCAP testing system (Phadia, Uppsala, Sweden).
FEV1 and forced vital capacity (FVC) were measured using a Jaeger spirometer (Carefusion, Hochberg, Germany). A bronchodilator test was performed to assess FEV1 and FVC values after inhalation of two puffs of Salbutamol sulfate (200 μg Ventolin HFA, GlaxoSmithKline, Middlesex, England).
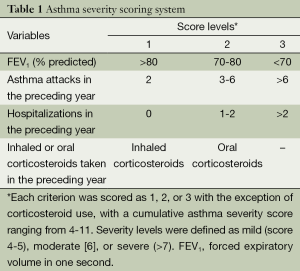
Definitions of asthma severity
An asthma severity score was used to classify the patients’ asthma as mild, moderate, or severe based on the criteria of Zureik et al. (7) and Ronchetti et al. (15). Briefly, scores took into account the patient’s FEV1 values (mild: >80%, moderate: 70-80%, or severe: <70% predicted), the number of asthma attacks in the past year (2, 3-6, or >6), the number of hospital admissions for respiratory problems in the past year (0, 1-2, or >2), and whether inhaled or oral corticosteroids were taken in the past year. Each criterion was scored as 1, 2, or 3 based on increasing severity and with the exception of corticosteroid use, which was scored as either 1 or 2 (Table 1). Scores for all four criteria were combined to produce a severity score ranging from 4 to 11, with severity levels being mild (score 4 or 5), moderate [6], or severe (>7).
Full table
Statistical analysis
The statistical analysis was performed using SPSS, version 20.0 (SPSS, Chicago, IL, United States). Parametric data was expressed as mean ± standard deviation (SD) and significance between groups was determined using a one-way ANOVA (least significant difference test) test. Nonparametric data were expressed as medians with interquartile ranges and compared using Kruskal-Wallis test to determine statistical significance. When the result of nonparametric test was statistically significant, further comparisons between two groups were done with Bonferroni corrected test (P<0.017). The associations between sensitisation to different aeroallergens and severity of asthma (mild, moderate, severe) were tested using logistic regression. Unless otherwise noted, statistical significance was defined as P<0.05.
Results
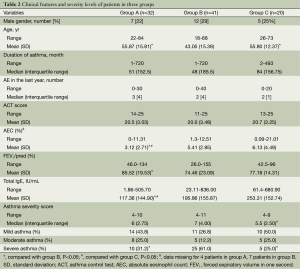
Ninety-three patients who met the inclusion criteria were divided into three groups according to the result of a skin prick allergy test. Group A included 32 asthmatic subjects with negative skin test results; group B included 41 asthmatic subjects with positive skin test results for polyvalent molds or Aspergillus fumigatus, group C included 20 asthmatic subjects with positive skin test results for aeroallergens, but negative for molds.
Clinical features of the three groups are shown in Table 2. Patients in group B were younger (43.05±15.39) than patients in group A (55.88±15.81, P<0.001) and group C (55.80±12.37, P=0.002), and had a lower FEV1 (74.46%±23.09% predicted) compared with patients in group A (85.52±19.53%, P=0.023). Patients in both group B and C had elevated AEC (group A: 3.12%±2.71%, group B: 5.41%±2.85%, group C: 6.1%±4.49%; group A vs. group B, P=0.008; group A vs. group C, P=0.002), and total sIgE values (group A: 117.36±144.90 IU/mL, group B: 195.86±155.87 IU/mL, group C: 253.31±152.41 IU/mL; group A vs. group B, P=0.031; group A vs. group C, P=0.002) compared with patients in group A .
Full table
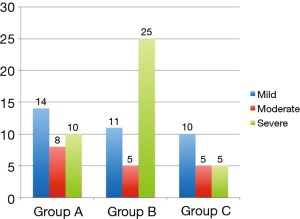
To directly assess the relationship between mold sensitivity and asthma severity, we compared asthma severity scores between the three groups. Patients in group B had higher asthma severity scores (median score: 7) than patients in groups C (median score: 5.5). However, there was no significantly different between patients in group A and group B (Table 2). Of the 93 patients enrolled in this study, 35 (37.6%) had mild asthma, 18 (19.4%) had moderate asthma, and 40 (43%) had severe asthma. Among the three groups, patients in group B had the highest proportion of patients with severe asthma (25 cases, 61%, Figure 1).
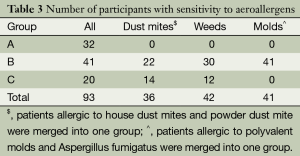
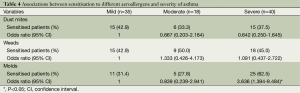
As shown in Table 3, sensitisation to a single allergen alone was rare. In patients with positive skin test results for aeroallergens, over 83% (n=51) of participants were sensitive to two or more allergens. We analyzed the relationship between sensitization to different allergens (house mites, weeds and molds) and asthma severity independently (Table 4). Patients allergic to molds were more likely to have severe asthma, the odds ratio was 3.636 for severe versus mild asthma (P<0.05). No association between asthma severity and allergic to mites or weeds was found in our patient cohort.
Full table
Full table
Discussion
To date, the relationship between the increases in mold sensitivity and allergy severity have not been adequately investigated (16,17). In the present study, we have identified a positive link between mold sensitivity and asthma severity in a cohort of adult patients in northern China. Patients with severe asthma were more common in patients allergic to molds. Furthermore, asthmatic subjects with mold allergies had a lower FEV1 compared to asthmatic subjects without allergies, suggesting more compromised pulmonary function in mold-sensitive patients.
Our study has significant implications for the management of asthmatic patients, given the mold allergy prevalence in China. Cross-sectional surveys performed in allergic patients (including those with asthma and/or rhinitis) showed the overall prevalence of mold sensitivity was between 4.4-19.8% (18,19). In our previous study of 200 asthmatic outpatients, 31 patients (16.5%) had positive skin reactivity to mixed mold, and 11 patients (5.5%) had positive reactivity to Aspergillus fumigatus (20).
The relationship between mold sensitivity and the asthma severity has recently received increased attention in Mainland China. A retrospective study reported three cases of severe asthma with fungal sensitization (SAFS) in 2010 (21). A comparison of sIgE titers against five mold and seven non-mold allergens in 100 patients with asthma, showed that Aspergillus-sIgE, Penicillium-sIgE and Candida-sIgE titers were higher in the patients with severe asthma compared to those of patients with moderate and mild asthma (P<0.001 and P<0.05, respectively), and higher in the patients with moderate asthma than patients with mild asthma (P<0.05) (22). Taken together with our findings, these studies suggest that mold sensitivity contributes to asthma severity. Further understanding of the relationship between fungal concentrations of indoor, outdoor environments with asthma exacerbations would contribute to the control of asthma.
House dust mites were the most prevalent allergens in our cohort, as well as in other studies in China (18,19). In a China Alliance of Research on Respiratory Allergic Disease (CARRAD) survey, moderate-severe asthma was associated with increasing wheal size and sIgE response to Dermatophagoides pteronyssinus and Dermatophagoides farinae in China (23). Zureik et al. found that both sensitivity to mold and dust mites were related to asthma severity (7). In contrast, our data indicated that only mold sensitivity was positively correlated with asthma severity. This discrepancy may be due to differences in allergens, age, or other region-specific characteristics of the patient populations studied as well as the different measurements of clinical disease severity.
However, this study also has limitations. Firstly, it was a small cross sectional study in a specialized clinic; our results may not accurately represent the general northern Chinese population. Secondly, skin prick tests to individual molds instead of “polyvalent molds” would have provided more convincing and precise information when correlating with severity of asthma. New diagnostic approaches, such as fungal enzyme microarrays, would have provided a better and enhanced insight regarding sensitization to molds.
Conclusions
In conclusion, we identified a link between mold sensitization and asthma severity in a cohort of patients in northern China, and this link was not found in other two common allergens, house mites and weeds. It may be possible to reduce asthma morbidity through reduced exposure to mold of other interventions that affect mold sensitivity. Furthermore, an understanding of how mold allergies contribute to asthmatic disease could lead to novel treatment and management options for patients with severe asthma.
Acknowledgements
Funding: This work was supported by grants from the Research and Development funds of Peking University People’s Hospital (Grant No. RDC2009-16).
Authors’ contributions: Yanliang Ma and Guizhen Tian participated in the design of the study, performed the statistical analyses, and wrote the manuscript. Fei Tang, Bing Yu, Yanwen Chen, and Yueli Cui participated in the acquisition and analysis of the data. Quanying He and Zhancheng Gao conceived the study, participated in its design, and assisted with writing the manuscript. All authors reviewed and approved the final manuscript.
Disclosure: The authors declare no conflict of interest.
References
- Yangzong Y, Shi Z, Nafstad P, et al. The prevalence of childhood asthma in China: a systematic review. BMC Public Health 2012;12:860. [PubMed]
- Wang WY, Lin JT, Su N, et al. Survey on the prevalence rate of bronchial asthma in Beijing area among the residents aged over 14 years from 2010 to 2011. Zhonghua Yi Xue Za Zhi 2013;93:1383-7. [PubMed]
- Jackson DJ, Sykes A, Mallia P, et al. Asthma exacerbations: origin, effect, and prevention. J Allergy Clin Immunol 2011;128:1165-74. [PubMed]
- Peters SP, Jones CA, Haselkorn T, et al. Real-world Evaluation of Asthma Control and Treatment (REACT): findings from a national Web-based survey. J Allergy Clin Immunol 2007;119:1454-61. [PubMed]
- Denning DW, O'Driscoll BR, Hogaboam CM, et al. The link between fungi and severe asthma: a summary of the evidence. Eur Respir J 2006;27:615-26. [PubMed]
- Knutsen AP, Bush RK, Demain JG, et al. Fungi and allergic lower respiratory tract diseases. J Allergy Clin Immunol 2012;129:280-91. [PubMed]
- Zureik M, Neukirch C, Leynaert B, et al. Sensitisation to airborne moulds and severity of asthma: cross sectional study from European Community respiratory health survey. BMJ 2002;325:411-4. [PubMed]
- O'Driscoll BR, Hopkinson LC, Denning DW. Mold sensitization is common amongst patients with severe asthma requiring multiple hospital admissions. BMC Pulm Med 2005;5:4. [PubMed]
- Niedoszytko M, Chełmińska M, Jassem E, et al. Association between sensitization to Aureobasidium pullulans (Pullularia sp) and severity of asthma. Ann Allergy Asthma Immunol 2007;98:153-6. [PubMed]
- Black PN, Udy AA, Brodie SM. Sensitivity to fungal allergens is a risk factor for life-threatening asthma. Allergy 2000;55:501-4. [PubMed]
- Fairs A, Agbetile J, Hargadon B, et al. IgE sensitization to Aspergillus fumigatus is associated with reduced lung function in asthma. Am J Respir Crit Care Med 2010;182:1362-8. [PubMed]
- Targonski PV, Persky VW, Ramekrishnan V. Effect of environmental molds on risk of death from asthma during the pollen season. J Allergy Clin Immunol 1995;95:955-61. [PubMed]
- Asthma Group of Chinese Society of Respiratory Diseases. Guidelines for prevention and treatment of Asthma. Chin J Tuberc Respir Dis 2008;31:177-85.
- Schwartz HJ, Greenberger PA. The prevalence of allergic bronchopulmonary aspergillosis in patients with asthma, determined by serologic and radiologic criteria in patients at risk. J Lab Clin Med 1991;117:138-42. [PubMed]
- Ronchetti R, Indinnimeo L, Bonci E, et al. Asthma self-management programmes in a population of Italian children: a multicentric study. Italian Study Group on Asthma Self-Management Programmes. Eur Respir J 1997;10:1248-53. [PubMed]
- Zainudin BM, Lai CK, Soriano JB, et al. Asthma control in adults in Asia-Pacific. Respirology 2005;10:579-86. [PubMed]
- Lin JT, Chen P, Zhou X, et al. Budesonide/formoterol maintenance and reliever therapy in Chinese patients with asthma. Chin Med J (Engl) 2012;125:2994-3001. [PubMed]
- Li J, Sun B, Huang Y, et al. A multicentre study assessing the prevalence of sensitizations in patients with asthma and/or rhinitis in China. Allergy 2009;64:1083-92. [PubMed]
- Hao GD, Zheng YW, Gjesing B, et al. Prevalence of sensitization to weed pollens of Humulus scandens, Artemisia vulgaris, and Ambrosia artemisiifolia in northern China. J Zhejiang Univ Sci B 2013;14:240-6. [PubMed]
- Ma YL, Zhang WB, Yu B, et al. Prevalence of allergic bronchopulmonary aspergillosis in Chinese patients with bronchial asthma. Zhonghua Jie He He Hu Xi Za Zhi 2011;34:909-13. [PubMed]
- Huang S, Wang JL, Wang LM. A retrospective study of 3 cases of severe asthma with fungal sensitization. Zhonghua Jie He He Hu Xi Za Zhi 2010;33:840-3. [PubMed]
- Zou H, Su L, Fang Q, et al. Specific IgE response to fungi and asthma severity. Chinese Archives of Otolaryngology-Head and Neck Surgery 2013;20:133-6.
- Li J, Huang Y, Lin X, et al. Influence of degree of specific allergic sensitivity on severity of rhinitis and asthma in Chinese allergic patients. Respir Res 2011;12:95. [PubMed]


