Esophageal cancer revealing a tracheal diverticulum
Introduction
Tracheal diverticulum is a benign entity characterized by single or multiple invaginations of the tracheal wall (1). It is rarely encountered in clinical practice but frequently in postmortem examination as an incidental finding, because almost all patients are asymptomatic (1-3). The overall prevalence of tracheal diverticula has been estimated to be 1% in an autopsy series (1,2,4). Despite many reports about tracheal diverticulum, its combination with esophageal cancer is rare. In this case report, we present a patient with these two lesions and analyze their correlation.
Case presentation
A 74-year-old female was referred to our Hospital because of dysphagia. Over the past few decades, she occasionally suffered from mild dysphagia and laryngeal friction, especially when swallowing food at a mouthful. But in the past six months, the symptoms were intensified and sometimes mucous sputum occurred. No other obvious digestive symptom was present. She denied fever, chest pain, asthma, dyspnea, and obvious weight loss. Her parents, siblings and children have no history of similar diseases. She had no history of smoking and denied regular alcohol intake. Physical examination disclosed no abnormity except for scattered rhonchi in both lungs and laboratory examinations showed mild anemia. An upper endoscopy visualized with esophageal scan revealed a stenotic lesion 24 cm from the incisors which was confirmed by barium contrast study. Pathology of the lesion (extracted by endoscopy) prompted esophageal squamous cell carcinoma.
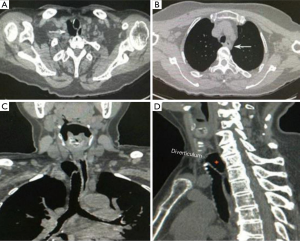
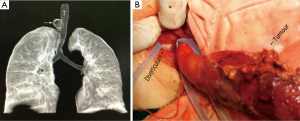
The computed tomography (CT) scans of the neck and chest showed a 3.1 cm × 2.1 cm elliptic air-filled cavity, which was adjacent to the posterolateral wall of the trachea at the level of the T1 vertebral body, and wall thickening of esophagus at the T3 level (Figure 1). We did not find any connection between the diverticulum and trachea through bronchoscopy and CT, but we cannot deny the existence of some very small orifices between them or just some fibrous connections (Figure 2A). A week later, the esophageal carcinoma was surgically resected by thoracoscope through right chest and upper abdomen, while the gastric tube and esophageal stump were anastomosed at the left neck. We could touch the diverticulum and see its translucent smooth surface through the incision on the left side of the neck (Figure 2B). The diverticulum had not been treated surgically. The pathologic report confirmed the diagnosis of esophageal squamous cancer (ulcer type). Postoperative course was normal and significant improvement was observed 2 months after surgery.
Discussion
Tracheal diverticula can be divided into two types: congenital and acquired, and they are different in shape, structure, location, and medical histology (1). The congenital type is considered to be a malformed supernumerary lung and generally consists of respiratory cartilage smooth muscle and epithelium, which is more common in men, and often appears on the right side of trachea, 4-5 cm below the vocal cords (1,4,5). Acquired tracheal diverticula are always larger than congenital ones, and result from increased intraluminal pressure caused by repeated coughing or obstructive pulmonary disease combined with a weakened trachea wall due to respiratory trauma or chronic inflammation (6). Therefore, they can occur at any level and the wall in them is often composed of respiratory epithelium, without any cartilaginous or smooth muscular element.
Tracheal diverticula are usually incidental on radiographic or CT findings. Paratracheal air cysts were visible in only 14% of the study subjects on chest radiographs (4). The optimal modality for diagnosis seems to be a thin-slice CT of the trachea and 3-dimensional (3D) reconstruction, which provide information about the origin, size and connection of the diverticulum. On CT images, 98.5% of the paratracheal air cysts were located in the right posterolateral region, at a level between T1 and T3 vertebra, because this region is probably the point of least resistance at the limit of the intra and extra thoracic trachea (4,7). Differential diagnosis includes pharyngocele, laryngocele, pneumomediastinum, apical hernia of the lung and the other paratracheal air cysts (1-3). Furthermore, most tracheal diverticula are asymptomatic and tend to be incidentally detected. Nevertheless, a tracheal diverticulum filled of sputum and other secretions acts as a bacterial culture medium, leading to repeated respiratory infection and aggravating hemoptysis, stridor, or dyspnea. Rarely, a large diverticulum can compress the recurrent laryngeal nerve, resulting in dysphonia, or compress esophagus, giving rise to dysphagia. On the other hand, treatment options can be divided into surgical resection (rarely advocated but should be reserved for young or symptomatic patients), laser cauterization via rigid bronchoscopy, and conservative treatment (antibiotics, bronchodilators, mycolytic agents and physiotherapy in the elderly and debilitated patients). However, in clinic, specific intervention is usually not necessary for the majority of patients who are asymptomatic (1,3,4). Moreover, some large tracheal diverticula, especially posterior ones, can compress the esophagus thus result in dysphagia (2). In comparison, their tracheal diverticulum and our, have similar form, location and size. This conclusion may also explain why our patient experienced mild dysphagia for years. As far as we know, this is the first case report in which the patient had the combination of esophageal cancer and tracheal diverticula. Although no direct relationship was found between tracheal diverticulum and esophageal cancer through the adjacent tissues, we cannot deny that the dysphagia caused by esophageal cancer can be aggravated by the tracheal diverticulum. As for this case, the dysphagia was alleviated gradually after esophagectomy.
It is noteworthy that the operation should be avoided if the patient suffered from respiratory tract infection or foreign body retention in tracheal diverticulum detected by bronchoscope. Besides, an accurate positioning of the diverticulum by CT is helpful, and protection of the diverticulum during esophagectomy and lymph node dissection is mandatory as it is fragile and risky for perforation or even esophago-tracheal fistula. Additionally, resection of tracheal diverticulum could be considered if it was perforated during the surgery to avoid mediastinal infection. Furthermore, a shortened period of tracheal intubation after the operation is recommended to avoid ventilator associated pneumonia.
Acknowledgements
Funding: This study was supported by Postgraduate Research Fund of Xuzhou Central Hospital (No.2012010). And we appreciate the staff of the Department of Imaging of our hospital.
Disclosure: The authors declare no conflict of interest.
References
- Soto-Hurtado EJ, Peñuela-Ruíz L, Rivera-Sánchez I, et al. Tracheal diverticulum: a review of the literature. Lung 2006;184:303-7. [PubMed]
- Han S, Dikmen E, Aydin S, et al. Tracheal diverticulum: a rare cause of dysphagia. Eur J Cardiothorac Surg 2008;34:916-7. [PubMed]
- Haghi Z, Towhidi M, Fattahi H, et al. Right paratracheal air cyst (tracheal diverticulum). Respir Care 2009;54:1409-11. [PubMed]
- Sato T, Sasaki Y, Yamasaki M, et al. A right paratracheal air cyst caused by tracheal diverticula. Intern Med 2010;49:315-9. [PubMed]
- Charest M, Sirois C, Cartier Y, et al. Infected tracheal diverticulum mimicking an aggressive mediastinal lesion on FDG PET/CT: an interesting case with review of the literature. Br J Radiol 2012;85:e17-21. [PubMed]
- Kokkonouzis I, Haramis D, Kornezos I, et al. Tracheal diverticulum in an asymptomatic male: a case report. Cases J 2008;1:181. [PubMed]
- Zhu G, Xu D, Xu H, et al. Tracheal diverticula in infants: a report of three cases. Clin Imaging 2012;36:221-3. [PubMed]


