
Diagnosis and management of sternoclavicular joint infections: a literature review
Introduction
Sternoclavicular joint infections (SCJI) constitute less than 1% of all joint infections. Infections of this joint have clinical significance for physicians of all specialties particularly primary care, emergency medicine, infectious disease, thoracic and orthopedic surgeons (1-4). In the primary care setting, it can present as a rash, while in the Emergency Room, it can present as chest pain radiating down the arm (3,4). Due to the ambiguity of presentation and low prevalence, the diagnosis of SCJI is often delayed. This causes infection to spread to the nearby tissues. So, it is important to understand the etiology, pathophysiology and treatment of SCJI. There are currently no standardized diagnostic and therapeutic algorithms for SCJI as defined in literature (1). We present the following article in accordance with the Narrative Review reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-761).
The sternoclavicular joint (SCJ) lies in proximity to important structures such as the subclavian vessels and the phrenic nerve. Infections of this structure should be taken seriously and addressed immediately to prevent extension and damage to the valuable nearby structures. Treatment options for SCJI include IV antibiotics, incision and drainage, surgical debridement and/or en bloc resection depending on the severity and extension of the infection. Surgical resection with or without muscle flaps is often preferred over medical management for osteomyelitis of SCJI. In this paper, we explore the existing literature to understand the knowledge on the diagnosis and treatment methods of SCJI.
Methods
We searched English publications in PubMed with the phrases “sternoclavicular joint”, “sternoclavicular joint infections”, “septic arthritis of the sternoclavicular joint”, “osteomyelitis of sternoclavicular joint” and “surgical management of sternoclavicular joint infection”. We included clinical trials, case reports, case series, retrospective cohort studies, literature and systematic reviews. We excluded papers with non-infectious etiology of SCJ pathologies from this review. Our search yielded 346 papers. We included 95 papers between 2000 and 2019 in our literature review. In this paper, we will focus on the infectious pathologies of SCJ. Two types of infections need to be considered while evaluating SCJ infections: septic arthritis and osteomyelitis. Septic arthritis involves the direct invasion of the joint space by pathogens (5). Osteomyelitis involves infection of the bone that can occur due to hematogenous seeding or direct extension into the joint space (6). Septic arthritis can often convert itself to osteomyelitis due to delay in diagnosis or inadequate initial treatment.
Discussion
Anatomy
The sternoclavicular joint is a saddle type, diarthrodial or synovial joint that functions as the only articulation between the upper extremity and axial skeleton (7). It comprises of the lateral notch of the manubrium, the medio- inferior head of the clavicle, and the costal-cartilage of the first rib. These joints are covered by fibrocartilages on the outside and synovial membranes on the inside. There are four main ligaments that stabilizes the sternoclavicular joint namely, anterior and posterior sternoclavicular ligaments, interclavicular ligament and costoclavicular ligament. The anterior sternoclavicular ligament originates from the anteromedial surface of the first rib and inserts superiorly and laterally on the clavicle. The posterior sternoclavicular ligament originates lateral to the anterior fibers and inserts superiorly and medially on the clavicle. The interclavicular ligament joins the superomedial aspect of the clavicle to the upper sternum. This protects against inferior displacement of the medial clavicle. The costoclavicular or rhomboid ligament, consisting of two fascicles, joins the clavicle with the first rib. This provides stability to the sternoclavicular joint during elevation and rotation of the clavicle (7,8).
Blood supply to this joint comes from the internal thoracic artery and suprascapular artery. The medial supraclavicular nerve (C3 and C4) and the nerve to the subclavius (C5 and C6) innervate this joint. The clavicular head of the pectoralis major, sternocleidomastoid and sternohyoid muscles attach to the medial clavicle anteriorly, posteriorly and inferiorly, respectively.
The bony articulation between the medial end of the clavicle and the manubrium is <50% of the surface area, making the joint potentially unstable (9). The stability is maintained by the anterior and posterior capsule. The anterior capsule prevents anterior subluxation, while the posterior capsule prevents both anterior and posterior subluxation of the SCJ. The sternoclavicular joint can glide up to 30 degrees antero-posteriorly, pivot up to 30 degrees supero-inferiorly and rotate up to 45 degrees axially.
Pathology
The SCJ is lined by fibrocartilage, not hyaline cartilage. The presence of this bulky central disc may predispose this joint to have the same susceptibility to infections as amphiarthrodial joints like the pubic symphysis and sacroiliac joint. These joints have limited mobility and are without a synovial lining (10). The joint capsule is unable to distend freely, which creates high intra-articular pressures. This facilitates dissemination of infections, possibly through lymphatics, into adjacent tissues (11).
The SCJ lies in proximity to important vasculature, nerves and organs in the thoracic cavity such as the great vessels of the superior mediastinum, trachea, esophagus, vagus nerve and phrenic nerve. Hence, pathology of this joint should be managed carefully and promptly to prevent spread to these nearby structures (12). Pathologies of this joint include injury, infections, malignancy, rheumatoid arthritis, SAPHO (syndrome of synovitis, acne, pustulosis, hyperostosis and osteitis) (13), Tietze’s syndrome (14), Lemierre syndrome (15) and Friedrich’s disease (16). SCJIs can often be mistaken with any of these other pathologies.
Medical history and physical exam
A detailed medical history is crucial in evaluating SCJ infections. Since SCJI frequently affects patients with pre-existing systemic diseases, an inquiry about arthritic diseases, diabetes, recent trauma, infections and hospitalizations. is paramount. SCJI are mostly unilateral (95%), with the majority occurring on the right side (60%) (17). This difference in laterality becomes less apparent in IV drug users (18). Unilateral SCJI can often present with fever, joint swelling, warmth and immobility. Bilateral infections can present as a butterfly rash on the chest (19). Some unusual presentations have also been reported in literature, such as a pressure like chest pain radiating to the neck or shoulder. This pattern of pain can mimic a myocardial Infarction. Other unusual presentations include vocal cord palsy (20), dysphagia (21), cervical esophageal rupture (22), lower respiratory infection (23), breast abscess (24) and subclavian compression syndrome (25).
It is very rare that SCJIs get diagnosed at the first visit. Diagnosis is often delayed, as the initial symptoms can be quite subtle (26). Reasons for the delay in diagnosis can be attributed to ambiguity in presentation, slow progression, and prior treatment with steroids (27). Slow progression can be attributed to the surrounding ligaments that reinforce the SCJ creating a relatively non-distensible synovial space. This makes large effusions extremely rare. The mean duration of symptoms for SCJI is approximately 14 days (28).
Risk factors
There are several risk factors for SCJ infections. The most common factors are an immunocompromised state, diabetes mellitus, end stage renal disease (29), intravenous drug use, trauma (30,31), presence of a central venous catheter (32), rheumatoid arthritis and intra-articular injections. Other risk factors include suprapubic catheter (33), crystalline arthropathies, radiation, cirrhosis, joint surgery, skin infections, malignancy (34), chemotherapy, breast cancer and radiation (35), tracheostomy (36), epidural block (37) and coronary angiography (38). However, 23% of cases are not associated with any predisposing factor (39).
SCJIs can spread either hematogenously or from direct extension to contiguous structures. Sixty-two percent of patients with SCJI have bacteremia (40). It is theorized that immunocompetent individuals can clear transient bacteremia, but immunocompromised individuals fail to do so effectively. Transient bacteremia can lead to seeding of the SCJ and ultimately cause osteomyelitis of the joint (41,42). There are three stages for this process: invasion (days), suppuration (weeks), and possible sepsis (43). Contiguous spread, on the other hand, can occur from the joint directly to the skin, lung or other nearby structures. Delayed presentations will result in more extensive direct spread at the time of diagnosis.
Laboratory data
Laboratory workup includes complete blood count, erythrocyte sedimentation rate, c-reactive protein, rheumatoid factor, antinuclear antibody and human leukocyte antigen B27. Mean values, ranges and sensitivities of each lab test are reported in Table 1.
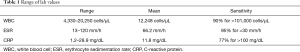
Full table
Imaging
Diagnostic workup includes imaging like x-ray, computed tomography and magnetic resonance imaging if more soft tissue detail is needed. Only 20% of cases of osteomyelitis have abnormal radiographic findings by the second week of symptoms. Inflammatory factors associated with infections accumulate in the joint space increasing the diameter of the joint space. This increased diameter is in contrast to typical osteoarthritis and joint degeneration, in which the joint space is narrowed due to loss of cushioning between bones. If the average joint distention is 14 mm (range, 10–20 mm), it is more likely to be infection. If the distension is 5 mm (range, 3–8 mm), it is more consistent with degeneration (44). A chest X-ray is usually the first step in diagnosis. It may show joint space distension and soft tissue shadow widening. It usually takes 10–12 days for soft tissue swelling to be evident on a typical X-ray. Demineralization and bony destruction tend to appear much later.
Ultrasound (US) is another diagnostic modality that can be used and is a safe diagnostic test to use during pregnancy (45). Infection is less likely if the distance of the joint capsule from the bone is less than 3 mm (46). However, the sensitivity for US is low (47). US-guided aspiration can also be performed if an obvious fluid collection is seen (48).
Computed tomography (CT) scan has an 83% sensitivity in diagnosing SCJI. CT-guided aspirations are safe and have yielded positive cultures in more than 50% of cases (49). CT can further elucidate the extent of anatomical involvement but cannot show soft tissue involvement.
Magnetic resonance imaging (MRI) is almost 100% sensitive but has low specificity. It yields a faster diagnosis than other imaging modalities. The earliest changes can be seen on MRI within 1–2 days, whereas, other modalities rarely show changes before 10 days. MRI can show capsular distension (>5 mm), extracapsular fluid collection, periarticular muscle edema and bone erosion. Osteomyelitis is seen as a hypointense signal on T1-weighted images and hyperintense signal on T2-weighted images. Even though MRI is sensitive in diagnosing SCJI, it is usually not obtained in the initial work up period. On MRI appearance SCJI can be misinterpreted as a bony metastasis (50).
A triple phase technetium bone scan, positron emission tomography (PET) scan and skeletal scintigraphy are other modalities which are rarely needed to diagnose SCJI. A technetium bone scan can show radiologic changes within hours of onset of infection. The first two phases show hyperemia. PET scan shows increased fluorodeoxyglucose uptake (51). Skeletal scintigraphy may show increased radiotracer uptake in the sternum and sternoclavicular regions.
Infectious etiology
The most common infectious organism that causes SCJI in the general population is Staphylococcus aureus. Blood cultures in SCJI tend to be positive in 65% of cases. S. aureus is found in 44–67% of all septic arthritis cases and in 1.3% of the patients with tuberculosis (52). Endocarditis complicated by Staphylococcus pneumonia can also cause SCJI (53).
Streptococcus pneumoniae and Streptococcus pyogenes are other common causes of SCJI (54). These throat and lung infections can lead to lung abscesses which can spread to the SCJ in both immunocompetent and immunocompromised patients (55). These infections tend to be severe in immunocompromised patients and post-surgical patients complicating the course of treatment (56). Other species of Streptococcus such as Streptococcus viridans or Streptococcus sanguinis have been reported to cause SCJI after mis-placed tracheostomy tube in the pre-tracheal space in a patient with laryngeal cancer (57,58). Two reports of Streptococcus agalactiae have been reported in previous literature as well. One of the reports detailed a patient with uncontrolled diabetes, while the other report highlighted a superinfection after Mycobacterium tuberculosis (MTB) empyema (59,60). Haemophilus, Aggregatibacter, Cardiobacterium, Eikenella and Kingella (HACEK) organisms from the oral cavity have also been known to colonize the SCJ even in children (61,62).
SCJI with Mycobacterium tuberculosis is very rare (<5%) (63). Mycobacterium tuberculosis can spread both hematogenously and contiguously from an apical pulmonary tuberculous focus (64). An unusual presentation of Mycobacterium tuberculosis SCJI was reported in a patient after malaria infection (65,66).
Mycobacterium kansasii is another uncommon aquatic organism known to cause SCJI primarily in immunocompromised individuals. One fatal case was reported in a Caucasian female with Waardenburg syndrome complicated by diabetes mellitus, a learning disability, and 15 previous surgeries for deformities of her foot (67).
Pseudomonas aeruginosa is a gram negative organism responsible for 10% of SCJI in intravenous drug users, sickle cell disease and thalassemia (68). Escherichia coli is responsible for about 5% of SCJI. An unusual case of Escherichia coli was reported after drainage of a Bartholin gland cyst (69). Brucella, Pasteurella and Coxiella are additional causes of SCJI in populations that work with animals (70,71). Salmonella typhi is known to cause SCJI in sickle cell patients (72). Other species of Salmonella like Salmonella enterica serotype D can also cause SCJI (73).
Another source of SCJI is disseminated gonorrhea. There is increased risk for such infections in pregnancy due to an immunocompromised status (74). Propionibacterium and Corynebacterium are also other unusual organisms to cause SCJI (75,76). Propionibacterium can form biofilms on the articular joint. These biofilms delay the clearing of infections and may result in the need for multiple surgeries to debride the joint. Candida is known to be a fungal source of SCJI in HIV patients. Since SCJI can be caused by a myriad of pathogens, cultures of the pathogens are necessary for targeted antibiotics treatment of SCJI.
Medical management
Medical management is the first step in addressing SCJI. Soft tissue infections such as thrombophlebitis, chest wall cellulitis, myositis and septic arthritis respond well to appropriate medical therapy alone (77). IV antibiotics are considered first line. The type of antibiotic is chosen based on the suspected organism and route of infection of the joint. A broad-spectrum antibiotic is usually utilized as the initial treatment, and then replaced by a narrower choice depending on culture and susceptibility results. The most common antibiotics used are cephalosporins, vancomycin and fluoroquinolones (78). Intravenous antibiotics can be switched to oral ones either on discharge or as deemed appropriate by treating physicians. Symptoms usually resolve within weeks to months. Patients should be followed for an extended period of time to ensure complete resolution of infection (79). Antibiotic duration varies based on the severity of infection.
Surgery
Surgical management is preferred for extensive SCJI with bony involvement, abscesses, and periarticular fluid collection (80). En bloc resection is the preferred surgical procedure and has a much better chance of resolving the infection compared to simple debridement or piecemeal resection (81). Once the resection is performed, a wound vacuum dressing can be placed for weeks to facilitate granulation tissue formation and allow the wound edges to contract. Hyperbaric oxygen therapy is another option for delayed closure (82).
Placement of calcium sulfate beads impregnated with antibiotics has been used with varying success. Vancomycin and gentamicin loaded calcium sulfate beads are used to fill the defect. The beads get completely resorbed within weeks without increasing serum calcium levels (83,84).
When a large defect remains, various options exist for muscle flap reconstruction (85). The pectoralis major can be used and receives its neurovascular supply from the thoraco-acromial bundle (86). Latissimus dorsi flaps are also an option. Use of muscle flaps are associated with a higher need for blood transfusion and longer hospital stays (10.5 vs. 5.5 days) however (87-89).
Postoperative length of stay can be quite long, ranging between 5 and 40 days depending on the type and extent of surgery (90). Postoperative risks include empyema, pleural effusion, abscess, mediastinitis and sepsis (91-93). Sepsis is another life-threatening complication of SCJI (94,95). Mortality rate from SCJI sepsis ranges roughly from 8% to 15%.
Summary
SCJIs are rare but serious joint infections secondary to hematogenous or contiguous spread from a nearby source. SCJIs can occur after trauma, central venous catheter placement or intravenous drug use. Early detection and intervention are the goals of treatment of SCJIs. Patients presenting with symptoms such as fever, rash, tenderness to palpation on the joint should be evaluated for SCJI by obtaining appropriate imaging studies. Surgical intervention should be taken early in the course if antibiotic management is not effective. Patients should be monitored for postoperative developments of mediastinitis and sepsis.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-761
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-761). I Okereke serves as an unpaid editorial board member of Journal of Thoracic Disease from Dec 2018 to Nov 2020. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- von Glinski A, Yilmaz E, Rausch V, et al. Surgical management of sternoclavicular joint septic arthritis. J Clin Orthop Trauma 2019;10:406-13. [Crossref] [PubMed]
- Edwin J, Ahmed S, Verma S, et al. Swellings of the sternoclavicular joint: review of traumatic and non-traumatic pathologies. EFORT Open Rev 2018;3:471-84. [Crossref] [PubMed]
- McAninch SA, Smithson C, Juergens AL, et al. Sternoclavicular Joint Infection Presenting as Nonspecific Chest Pain. J Emerg Med 2018;54:229-31. [Crossref] [PubMed]
- Thompson MA, Barlotta KS. Septic Arthritis of the Sternoclavicular Joint. J Emerg Med 2018;55:128-9. [Crossref] [PubMed]
- Costales C, Butler-Wu SM. A Real Pain: Diagnostic Quandaries and Septic Arthritis. J Clin Microbiol 2018;56:e01358-17. [PubMed]
- Khan K, Wozniak SE, Mehrabi E, et al. Sternoclavicular Osteomyelitis in an Immunosuppressed Patient: A Case Report and Review of the Literature. Am J Case Rep 2015;16:908-11. [Crossref] [PubMed]
- Renfree KJ, Wright TW. Anatomy and biomechanics of the acromioclavicular and sternoclavicular joints. Clin Sports Med 2003;22:219-37. [Crossref] [PubMed]
- Blasberg JD, Donington JS. Infections and radiation injuries involving the chest wall. Thorac Surg Clin 2010;20:487-94. [Crossref] [PubMed]
- Paice EW, Wright FW, Hill AG. Sternoclavicular erosions in polymyalgia rheumatica. Ann Rheum Dis 1983;42:379-83. [Crossref] [PubMed]
- Schipper P, Tieu BH. Acute Chest Wall Infections: Surgical Site Infections, Necrotizing Soft Tissue Infections, and Sternoclavicular Joint Infection. Thorac Surg Clin 2017;27:73-86. [Crossref] [PubMed]
- Bar-Natan M, Salai M, Sidi Y, et al. Sternoclavicular infectious arthritis in previously healthy adults. Semin. Arthritis Rheum 2002;32:189-95. [Crossref] [PubMed]
- Robinson CM, Jenkins PJ, Markham PE, et al. Disorders of the sternoclavicular joint. The J Bone Joint Surg Br 2008;90:685-96. [Crossref] [PubMed]
- Restrepo CS, Martinez S, Lemos DF, et al. Imaging appearances of the sternum and sternoclavicular joints. Radiographics 2009;29:839-59. [Crossref] [PubMed]
- Hiramuro-Shoji F, Wirth MA, Rockwood CA Jr. Atraumatic conditions of the sternoclavicular joint. J Shoulder Elbow Surg 2003;12:79-88. [Crossref] [PubMed]
- Garimorth K, Kountchev J, Bellmann R, et al. Lemierre's syndrome following infectious mononucleosis. Wien Klin Wochenschr 2008;120:181-3. [Crossref] [PubMed]
- Higginbotham TO, Kuhn JE. Atraumatic disorders of the sternoclavicular joint. J Am Acad Orthop Surg 2005;13:138-45. [Crossref] [PubMed]
- Masmoudi K, Elleuch E, Akrout R, et al. Bilateral septic arthritis of the sternoclavicular joint complicating infective endocarditis: a case report. J Med Case Rep 2018;12:205. [Crossref] [PubMed]
- El Ibrahimi A, Daoudi A, Boujraf S, et al. Sternoclavicular septic arthritis in a previously healthy patient: a case report and review of the literature. Int J Infect Dis 2009;13:e119-121. [Crossref] [PubMed]
- Mamarelis G, Sohail MZ, Mamarelis A, et al. Spontaneous Bilateral Sternoclavicular Joint Septic Arthritis and Lumbar Discitis: An Unusual Case in a Healthy Adult. Case Rep Orthop 2017;2017:7101694.
- Jamil F, Hussain K. Vocal cord palsy as a presenting feature of sternoclavicular joint septic arthritis. J Surg Case Rep 2015;2015:rju147 .
- Das AK, Monga P. Septic arthritis of the sterno-clavicular joint as a cause of dysphagia: a report of two cases and review of literature. Clin. Rheumatol 2014;33:141-3. [Crossref] [PubMed]
- Katsoulis IE, Bossi M, Damani N, et al. Arthritis of the sternoclavicular joint masquerading as rupture of the cervical oesophagus: a case report. J Med Case Rep 2009;3:40. [Crossref] [PubMed]
- Lane N, Mackie A, Srivastava S. An unusual cause of 'musculoskeletal' chest pain. Acute Med 2009;8:111-3. [PubMed]
- Dhulkotia A, Asumu T, Solomon P. Breast abscess: a unique presentation as primary septic arthritis of the sternoclavicular joint. Breast J 2005;11:525-6. [Crossref] [PubMed]
- Rachapalli V, John A, Unsworth-White MJ. Mediastinal mass: a diagnostic conundrum. J Thorac Cardiovasc Surg 2007;133:586-7. [Crossref] [PubMed]
- Mohyuddin A. Sternoclavicular joint septic arthritis manifesting as a neck abscess: a case report. Ear Nose Throat J 2003;82:618-21. [Crossref] [PubMed]
- Crisostomo RA, Laskowski ER, Bond JR, et al. Septic sternoclavicular joint: a case report. Arch Phys Med Rehabil 2008;89:884-6. [Crossref] [PubMed]
- Kang BS, Shim HS, Kwon WJ, et al. MRI findings for unilateral sternoclavicular arthritis: differentiation between infectious arthritis and spondyloarthritis. Skeletal Radiol 2019;48:259-66. [Crossref] [PubMed]
- Carlos GN, Kesler KA, Coleman JJ, et al. Aggressive surgical management of sternoclavicular joint infections. J Thorac Cardiovasc Surg 1997;113:242-7. [Crossref] [PubMed]
- Tickell KD, Banim R, Kustos I. Salmonella sternoclavicular osteomyelitis in a patient with Crohn's disease. BMJ Case Rep 2013;2013:bcr2012007809.
- Fordham S, Cope S, Sach M. Optimal management of sternoclavicular septic arthritis. Eur J Emerg Med 2009;16:219-20. [Crossref] [PubMed]
- Pradhan C, Watson NF, Jagasia N, et al. Bilateral sternoclavicular joint septic arthritis secondary to indwelling central venous catheter: a case report. J Med Case Rep 2008;2:131. [Crossref] [PubMed]
- Monteiro N, Moleiro F, Lerias G, et al. Sternoclavicular septic arthritis due to methicillin-resistant Staphylococcus aureus in a patient with a suprapubic catheter. BMJ Case Rep 2015;2015:bcr2014208748.
- Rodchuae M, Ruangpin C, Katchamart W. Clinical manifestations, treatment outcomes, and risk factors for sternoclavicular septic arthritis. Rheumatol Int 2017;37:819-24. [Crossref] [PubMed]
- Chanet V, Soubrier M, Ristori JM, et al. Septic arthritis as a late complication of carcinoma of the breast. Rheumatology (Oxford) 2005;44:1157-60. [Crossref] [PubMed]
- Sharif KF, Baik FM, Jategaonkar AA, et al. Septic arthritis of the sternoclavicular joint: A unique late complication after tracheostomy. Am J Otolaryngol 2018;39:646-8. [Crossref] [PubMed]
- Shioya N, Ishibe Y, Kan S, et al. Sternoclavicular joint septic arthritis following paraspinal muscle abscess and septic lumbar spondylodiscitis with epidural abscess in a patient with diabetes: a case report. BMC Emerg Med 2012;12:7. [Crossref] [PubMed]
- Hoseini SK, Nouri A, Jozaghi S. A case of septic arthritis of the sternoclavicular joint after coronary angiography. Int Angiol 2008;27:536-8. [PubMed]
- Ross JJ, Shamsuddin H. Sternoclavicular septic arthritis: review of 180 cases. Medicine 2004;83:139-48. [Crossref] [PubMed]
- Robertson JJ. An Unusual Cause of Chest Pain in a Young Healthy Female. J Emerg Med 2015;49:429-31. [Crossref] [PubMed]
- Bautista-Casasnovas A, Varela-Cives R, Estevez Martinez E, et al. What is the infection risk of oesophageal dilatations? Eur J Pediatr 1998;157:901-3. [Crossref] [PubMed]
- Gürel HG, Basciftci FA, Arslan U. Transient bacteremia after removal of a bonded maxillary expansion appliance. Am J Orthod Dentofacial Orthop 2009;135:190-3. [Crossref] [PubMed]
- Corey SA, Agger WA, Saterbak AT. Acromioclavicular septic arthritis and sternoclavicular septic arthritis with contiguous pyomyositis. Clin Orthop Surg 2015;7:131-4. [Crossref] [PubMed]
- Johnson MC, Jacobson JA, Fessell DP, et al. The sternoclavicular joint: can imaging differentiate infection from degenerative change? Skeletal Radiol 2010;39:551-8. [Crossref] [PubMed]
- El Mezouar I, Tahiri L, Lazrak F, et al. Gonococcal polyarthritis with sternoclavicular joint involvement in pregnant woman: a case report. Pan Afr Med J 2014;17:242. [Crossref] [PubMed]
- Cone LA, Lopez C, O'Connell SJ, et al. Staphylococcal septic synovitis of the sternoclavicular joint with retrosternal extension. J Clin Rheumatol 2006;12:187-9. [Crossref] [PubMed]
- Bodker T, Tottrup M, Petersen KK, et al. Diagnostics of septic arthritis in the sternoclavicular region: 10 consecutive patients and literature review. Acta Radiol 2013;54:67-74. [Crossref] [PubMed]
- Song HK, Guy TS, Kaiser LR, et al. Current presentation and optimal surgical management of sternoclavicular joint infections. Ann Thorac Surg 2002;73:427-31. [Crossref] [PubMed]
- Taneja AK, Bierry G, Simeone FJ, et al. Diagnostic yield of CT-guided sampling in suspected sternoclavicular joint infection. Skeletal Radiol 2013;42:479-85. [Crossref] [PubMed]
- Alexiou E, Georgoulias P, Valotassiou V, et al. Multifocal septic osteomyelitis mimicking skeletal metastatic disease in a patient with prostate cancer. Hell J Nucl Med 2015;18:77-8. [PubMed]
- Henriksen J, Tang M, Hjortdal V. Abscess Formation after Septic Arthritis in the Sternoclavicular Joint of Two Healthy Men. Case Rep Surg 2015;2015:292854.
- Ghasemi Barghi R, Mirakbari SM. Septic arthritis of sternoclavicular joint: a case report of a rare finding in injecting drug users. Arch Iran Med 2010;13:248-50. [PubMed]
- Hamilton RJ, Wylie R. Sternoclavicular pyarthrosis. J Emerg Med 2003;24:327-8. [Crossref] [PubMed]
- Savcic-Kos RM, Mali P, Abraham A, et al. Streptococcus pyogenes sternoclavicular septic arthritis in a healthy adult. Clin Med Res 2014;12:155-9. [Crossref] [PubMed]
- Eckhouse SR, Person TD, Reed CE, et al. Sternoclavicular joint infection necessitating through skin and lung parenchyma. Ann Thorac Surg 2010;90:309-11. [Crossref] [PubMed]
- Vu TT, Yammine NV, Al-Hakami H, et al. Sternoclavicular joint osteomyelitis following head and neck surgery. Laryngoscope 2010;120:920-3. [PubMed]
- Hashmi A, Zerfas D, Baciewicz FA Jr. Sternoclavicular osteomyelitis: a new complication of misplaced tracheostomy tube. Ann Thorac Surg 2011;92:2240-1. [Crossref] [PubMed]
- Mandac I, Prkacin I, Matovinovic MS, et al. Septic arthritis due to Streptococcus sanguis. Coll Antropol 2010;34:661-4. [PubMed]
- Shibayama A, Yoshizaki T, Tamaki M, et al. Pyogenic Sternoclavicular Arthritis Caused by Streptococcus agalactiae in an Elderly Adult with Diabetes Mellitus. J Am Geriatr Soc 2016;64:1376-7. [Crossref] [PubMed]
- Buell KG, Ajmal S, Whitaker JA. A Complicated Case of Group B Streptococcus Empyema Necessitans. Cureus 2017;9:e1591. [PubMed]
- Loh JK, O'Shea D, O'Connell K, et al. Sternoclavicular joint septic arthritis and osteomyelitis caused by Aggregatibacter aphrophilus. QJM 2014;107:751-4. [Crossref] [PubMed]
- Alves S, Rodrigues L, Santos M, et al. Kingella kingae sternoclavicular osteoarthritis. BMJ Case Rep 2018;2018:bcr2017223213.
- Rizzo V, Salmasi Y, Hunter M, et al. Delayed diagnosis of chronic postoperative sternal infection: a rare case of sternal tuberculosis. BMJ Case Rep 2018;2018:bcr2017223650.
- Jain A, Jajodia N, Aggarwal A, et al. Tuberculosis of the sternoclavicular joint. J Orthop Surg (Hong Kong) 2015;23:315-8. [Crossref] [PubMed]
- Djiba B, Kane BS, Diallo MA, et al. Tuberculosis arthritis of the sternoclavicular joint after uncomplicated falciparum malaria: a case report. Ann. Clin. Microbiol. Antimicrob 2017;16:44. [Crossref] [PubMed]
- Epperla N, Kattamanchi S, Fritsche TR. Appearances are Deceptive: Staphylococcus Superinfection of Clavicular Tuberculous Osteomyelitis. Clin Med Res 2015;13:85-8. [Crossref] [PubMed]
- Bhatt K, Banavathi K. Mycobacterium kansasii osteomyelitis - a masquerading disease. JMM Case Rep 2018;5:e005114. [Crossref] [PubMed]
- Kaw D, Yoon Y. Pseudomonas sternoclavicular pyarthrosis. South Med J 2004;97:705-6. [Crossref] [PubMed]
- Kelly JC, Jia X, Vindenes T, et al. Chorioamnionitis and sternoclavicular septic arthritis after drainage of Bartholin gland abscess. Obstet Gynecol 2014;124:436-8. [Crossref] [PubMed]
- Mikroulis DA, Verettas DA, Xarchas KC, et al. Sternoclavicular joint septic arthritis and mediastinitis. A case report and review of the literature. Arch Orthop Trauma Surg 2008;128:185-7. [Crossref] [PubMed]
- Angelakis E, Thiberville SD, Million M, et al. Sternoclavicular joint infection caused by Coxiella burnetii: a case report. J Med Case Rep 2016;10:139. [Crossref] [PubMed]
- Bachmeyer C, Ammouri W, M'Bappe P, et al. Unusual sites of Salmonella osteoarthritis in patients with sickle cell disease: two cases. Clin. Rheumatol 2007;26:1356-8. [Crossref] [PubMed]
- Chiu WK, Huang TW, Cheng YL. Septic arthritis of the sternoclavicular joint caused by salmonella in a healthy person. Acta Chir Belg 2009;109:645-6. [Crossref] [PubMed]
- O'Leary AJ, Tejura H, Latibeaudiere M, et al. Gonorrhoea infection presenting in pregnancy with septic arthritis of the sternoclavicular joint. J Obstet Gynaecol 2006;26:373-4. [Crossref] [PubMed]
- Taylor T, Coe M, Mata-Fink A, et al. Native join Propionibacterium septic arthritis. Infect Dis Rep 2017;9:7185. [Crossref] [PubMed]
- Nguyen M, Moffatt-Bruce SD, Merritt RE, et al. Clinical Effectiveness of Negative Pressure Wound Therapy Following Surgical Resection of Sternoclavicular Joint Infection: A Case Report. Cureus 2016;8:e815. [PubMed]
- Womack J. Septic arthritis of the sternoclavicular joint. J Am Board Fam Med 2012;25:908-12. [Crossref] [PubMed]
- Murga A, Copeland H, Hargrove R, et al. Treatment for sternoclavicular joint infections: a multi-institutional study. J Thorac Dis. 2017;9:1503-8. [Crossref] [PubMed]
- Dhillon MS, Gupta RK, Bahadur R, et al. Tuberculosis of the sternoclavicular joints. Acta Orthop Scand 2001;72:514-7. [Crossref] [PubMed]
- Nusselt T, Klinger HM, Freche S, et al. Surgical management of sternoclavicular septic arthritis. Arch Orthop Trauma Surg 2011;131:319-23. [Crossref] [PubMed]
- Joethy J, Lim CH, Koong HN, et al. Sternoclavicular joint infection: classification of resection defects and reconstructive algorithm. Arch Plast Surg 2012;39:643-8. [Crossref] [PubMed]
- Tanaka Y, Kato H, Shirai K, et al. Sternoclavicular joint septic arthritis with chest wall abscess in a healthy adult: a case report. J Med Case Rep 2016;10:69. [Crossref] [PubMed]
- Whitlark JD, Kirollos JA, Jackson SM. Simplified Method for Treating Osteomyelitis of the Sternoclavicular Joint. Ann Thorac Surg 2016;101:1211-2. [Crossref] [PubMed]
- Huang K, Zhang C. Sternoclavicular Joint Infection Treated with Debridement, Vancomycin-Loaded Calcium Sulfate, and Partial Pectoralis Muscle Flap: A Case Report. JBJS Case Connect 2015;5:e86. [Crossref] [PubMed]
- Jackson RS, Carter YM, Marshall MB. Surgical Management of the Infected Sternoclavicular Joint. Oper Tech Thorac Cardiovasc Surg 2013;18:42-52. [Crossref]
- Al-Mufarrej F, Martinez-Jorge J, Carlsen BT, et al. Use of the deltoid branch-based clavicular head of pectoralis major muscle flap in isolated sternoclavicular infections. J Plast Reconstr Aesthet Surg 2013;66:1702-11. [Crossref] [PubMed]
- Raymond D. Surgical intervention for thoracic infections. Surg Clin North Am 2014;94:1283-303. [Crossref] [PubMed]
- Chen H, Ji X, Hao M, et al. A three-stage procedure using bone transportation for the treatment of sternoclavicular infectious arthritis. J Orthop Surg Res 2016;11:152. [Crossref] [PubMed]
- Bendon CL, Giele HP. Second toe metatarsophalangeal joint transfer for sternoclavicular joint reconstruction. J Hand Surg Am 2014;39:1327-32. [Crossref] [PubMed]
- Abu Arab W, Khadragui I, Echave V, et al. Surgical management of sternoclavicular joint infection. Eur J Cardiothorac Surg 2011;40:630-4. [PubMed]
- Gorospe L, Ayala-Carbonero AM, Jover-Diaz R. Septic sternoclavicular arthritis complicated with bilateral pleural effusions. Asian Cardiovasc Thorac Ann 2017;25:404-5. [Crossref] [PubMed]
- Chen WS, Wan YL, Lui CC, et al. Extrapleural abscess secondary to infection of the sternoclavicular joint. Report of two cases. J Bone Joint Surg Am 1993;75:1835-9. [Crossref] [PubMed]
- Dajer-Fadel WL, Ibarra-Perez C, Borrego-Borrego R, et al. Descending necrotizing mediastinitis and sternoclavicular joint osteomyelitis. Asian Cardiovasc Thorac Ann 2013;21:618-20. [Crossref] [PubMed]
- Haddad M, Maziak DE, Shamji FM. Spontaneous sternoclavicular joint infections. Ann Thorac Surg 2002;74:1225-7. [Crossref] [PubMed]
- Akkasilpa S, Osiri M, Ukritchon S, et al. Clinical features of septic arthritis of sternoclavicular joint. J Med Assoc Thai 2001;84:63-8. [PubMed]


