
Efficacy of standard chest compressions in patients with Nuss bars
Introduction
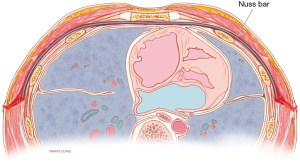
Minimally invasive repair (Nuss procedure) has rapidly become the standard of care for repair of pectus excavatum (PE) deformities (1). The procedure involves intrathoracic placement of metal (titanium or stainless steel) bars which elevate the deformed chest wall (Figure 1). The implants are left in place for 2–3 years while the chest wall remodels then removed during an outpatient procedure (2,3). Excellent, durable results have made the Nuss repair the procedure of choice by most patients and surgeons (Figure 2). Originally described for treatment of children and early adolescents (4), the procedure has been successfully extended into repair of adult populations (3,5,6). The presence of the intrathoracic bars not only changes the architecture of the chest wall, but while in place, impacts the normal excursion and compliance of the anterior chest wall (7). This compliance is integral to delivering effective chest compressions during cardiopulmonary resuscitation (CPR) in the event of a cardiac arrest (7,8). Cardiac and thoracic pumps facilitate blood flow to vital organs through the heart during CPR. With chest compression, the process involves mechanically compressing the heart between the sternum and spine. Chest compression depth is the objective parameter for determining standard CPR success with a recommended depth of 5 cm by the American Heart Association (AHA) (9,10). Recent studies have suggested that a chest compression depth approaching 5 cm (4.7 cm) has an impact on survival rates in out-of-hospital events (11). Our study was performed to assess the amount of force required to perform adequate chest compression depth in patients after a Nuss procedure. Additionally, alternative CPR methods were reviewed for consideration of use in patients after PE repair with Nuss bars in place.

Methods
A lumped element elastic model was developed to simulate the relationship between chest compression forces and displacement in the presence of Nuss bar(s). The AHA recommends a compression depth of about 5 cm (approx 2”) to ensure patient survival (12). As such, the model focussed on the amount of force required to achieve a depth of 5 cm under different chest elasticity conditions.
During CPR chest compressions, the applied forces displace the sternum which leads to the deformation of the thorax. As such, it was assumed that the sternum deflects up and down on a dynamic spring coefficient defined in Eq. [1] developed by Gruben et al. (12). It was also assumed that the costal cartilage and anterior rib bones’ elasticity is the primary factor for the elastic response of the human sternum. Therefore, during chest compressions, the elasticity of the chest operates parallel to the stiffness of the Pectus bar(s) as illustrated in the figure below (Figure 3).

[1]
The lumped element elastic model was adopted to simulate the applied force on the chest to chest displacement relationship in the presence of one to three metal bars in comparison to a chest without metal bars. Hook’s Law was used to determine the effective force required to displace the sternum by some depth x given an effective elastic coefficient (keff) as summarized in Eq. [2] below.
[2]
Since the Nuss bar has to bend inwards towards the direction of the spine in combination with the coastal cartilage and anterior ribs, the effective elasticity was the sum of the spring constants as illustrated in Eq. [3] below.
[3]
The dynamic elastic property of the human chest k_c was modeled using Gruben’s elastic polynomial coefficient (12) shown in Eq. [1].
where a1=29.4, a2=22.3, a3=−1.35, a4=0.325.
The elastic coefficient of the Nuss bar was calculated in two steps. Firstly, the force to deflect the Nuss bar by 5 cm was calculated following a derivation from the “Classical Strength of Materials” Eq. [4] shown below (13):
[4]
where ∆=5 cm,
and E is the young modulus of the Nuss bar. L is the bendable length, b is the breadth and h is the depth/height of the cross-section area of the Nuss bar. Secondly, the realized force and 5 cm deflection were plugged to the Hooke’s Law in Eq. [2] above to solve for k as the elastic constant of the Nuss bar.
For the Nuss bar, a sample bar with the following measurements was used for an estimated elastic constant: bendable length (L) =20.48 cm, depth (h) =0.3048 cm, and width (b) =1.27 cm. Note that the bendable strength is not necessarily the full length of the Nuss bar. It refers to the relatively flat anterior segment after the bar is bent during the Nuss procedure. Thus, it is assumed that the anterior chest moves contiguously with the posterior and wards together with the Nuss bar.
Finally, the human chest displacement in response to force applied during a chest compression was calculated and plotted in MATLAB using equations defined above.
Results
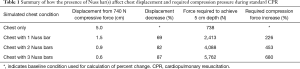
Applying Eq. [2], the elastic coefficients of the human chest only ranged from 29.4 to 147.78 N/cm with an average of 84.51 N/cm. The maximum force required to displace a chest without Nuss bar(s) to the recommended depth of 5 cm was determined to be 738 N [166 pounds force (lbf)]. Using the same compressive force of 738 N, a chest wall model with Nuss bar(s) resulted in significantly less displacement of the chest as shown in Figure 4.
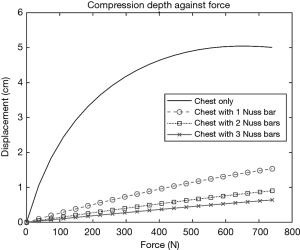
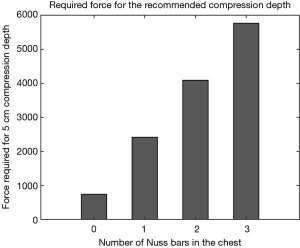
Introduction of the elasticity property of the Nuss bar(s) significantly reduced the dynamic elasticity of the chest’s elastic properties to deform. Unlike native bones which behave like a ceramic material, the metallic bars tend to have a more linear slope in their stress-strain curves. In this case, metal properties seem to be taking over. A compressive force of up to 6,000 N (1,349 lbf) were applied in simulation to demonstrate how much force could be required to displace a chest with Nuss bar(s) to the recommended depth of 5 cm (Table 1). The model showed that excessive forces could be required to achieve such a depth as summarized in Figure 5.
Full table
Discussion
As a center performing high volumes of minimally invasive PE repair in advanced aged adults (3), we initiated this study to assess the feasibility of performing CPR in patients while bars were in place. The Nuss procedure was originally reported for pediatric PE correction using a single bar (4). Multiple bars are now recommended in many patient populations including those with connective tissue disorders (14) and adults (3,5,6,15). As this procedure has been extended into adult populations as old as patients in their 70’s, cardiac events are likely to be more common. Yet, there are very few reports of the use of CPR in patients with Nuss bars (16-19). Although successful resuscitation occurred in a young adult with a single bar, there have been several case reports which describe the limitations of CPR for patients with one or more Nuss Bars (19-22). A summary of these reports is presented in Table 2. One case occurred in the operating room and the bars were removed with subsequent successful resuscitation (19). At least one case report of failed resuscitation had two Nuss bars in place (22).
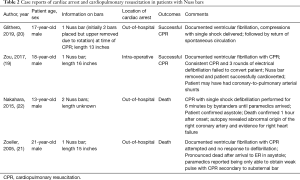
Full table
Our model predicted that a substantial increase in the amount of force is required to generate adequate chest compression during CPR in patients with Nuss bar(s). Additionally, the greater the number of Nuss bars present, the greater the force required. In our model, the presence of multiple Nuss bar(s) predicts that manual chest compressions would be potentially ineffective altogether. In addition, current CPR devices are not capable of compressing a chest with this level of force (23,24). In our model, the forces required for adequate CPR were approximately: (I) no bars 740 N (166 lbf); (II) 1 bar 2,500 N (560 lbf); 3 bars 5,500 N (1,230 lbf). Furthermore, the accompanying high stresses of such a magnitude of force may be associated with potentially serious injuries. As a result, the use of chest compressions during CPR in patients with Nuss Bars is unlikely to result in effective or adequate circulation and may actually cause additional harm. Post-operative Finite Element Methods (FEM) have shown that the stress caused by the Nuss bar(s) can be traced from the costal cartilage to the back of the patient based on variations in stiffness (25). Moreover, the findings of this model suggest that attempting to compress the anterior chest wall with the Nuss bar(s) in place could put bone or cartilage in the chest beyond its stress limits and consequently cause injury (26).
Active abdominal compression and decompression-CPR is a novel technique which is reported to improve artificial circulation using thoracic, abdominal and heart pumping mechanisms (27). Although availability is limited in many parts of the world, this relatively new CPR method induces pressure changes in the abdomen triggering the abdominal pump to transmit pressure to thoracic cavity which activates the thoracic and heart pump via the action of the diaphragm (28). A clinical study conducted on the effectiveness of Abdominal Lifting and Compression (AACD-CPR) versus Standard CPR (STD-CPR) by Zhang et al. reported better resuscitation outcomes for the AACD-CPR group as compared to the STD-CPR group. In the study, patients with cardiac arrest were randomized to receive both techniques. According to the report, patients in the AACD-CPR group had a significantly higher heart rate and lower mean arterial pressure (MAP) than those in the STD-CPR group (heart rate: 106.8 versus 79.0; MAP: 60.0 versus 67.3 mmHg (28). Perhaps more striking, the AACD-CPR led to a higher restoration rate of spontaneous circulation (ROSC) than STD-CPR (50% more than STD-CPR) and was associated with an increase in survival rate of patients (28). While there are no reports of the use of AACD-CPR after pectus repair, Zhang et al.’s findings suggest that this alternative method of CPR may have potential utility in patients with Nuss bars.
We continue to perform a modified Nuss as our experience has found this to be a superior for repair of PE in the majority of patients. Repair provides cardiopulmonary benefits including improved cardiac output and strain (29). Repair with an open approach often requires metal stabilization in the form of a strut bar or plating and is not exempt from inadequate and complicated CPR. We have not performed CPR in any of our Nuss patients; however, we have experienced unsuccessful resuscitation after the open Ravitch procedure.
Limitations
Our study was performed to assess the amount of force required to perform adequate chest compression depth in patients after PE repair with Nuss bars in place. The results of this study have limitations to be considered including the inability to account for the 3-dimentional elasticity of the chest wall not in contact with the metal implants. Lateral expansion of the ribs due to elasticity and even fracture may improve the ability to force compression of the anterior chest wall. Additionally, the chest compression forces and displacement presented here do not necessarily represent the cyclic compressions as prescribed in standard CPR. They rather represent a one-time compression with undefined speed. Consequently, the damping effect of the chest was not considered in the study. The parameters used in this model were derived from multiple sources and used a limited sample size in deriving the values the study has adopted. Lastly, the assumptions made on the use of various laws of physics and biomaterials were based on simplifying the complex anatomy of the chest to understand its interaction with the Nuss bar(s) and may not translate to human subjects.
Conclusions
In our model, Nuss bars limited the ability to perform chest compressions due to increased force required to achieve a 5 cm compression (9). The greater the number of Nuss bars present, the greater the force required. This limitation may prevent effective CPR. Use of active abdominal compressions and decompressions should be studied further as an alternative resuscitation modality for patients after the Nuss procedure.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-702). DEJ reports personal fees and other from ZimmerBioMet, Inc., outside the submitted work; in addition, DEJ has a patent ZimmerBioMet with royalties paid. DEJ discloses consulting and intellectual property rights under Mayo Clinic Ventures with Zimmer Biomet, Inc. DEJ also serves as an unpaid editorial board member of Journal of Thoracic Disease from Dec 2018 to Nov 2020. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nuss D, Obermeyer RJ, Kelly RE. Nuss bar procedure: past, present and future. Ann Cardiothorac Surg 2016;5:422-33. [Crossref] [PubMed]
- Kelly RE, Goretsky MJ, Obermeyer R, et al. Twenty-one years of experience with minimally invasive repair of pectus excavatum by the Nuss procedure in 1215 patients. Ann Surg 2010;252:1072-81. [Crossref] [PubMed]
- Jaroszewski DE, Ewais MM, Chao CJ, et al. Success of Minimally Invasive Pectus Excavatum Procedures (Modified Nuss) in Adult Patients (>/=30 Years). Ann Thorac Surg 2016;102:993-1003. [Crossref] [PubMed]
- Nuss D, Kelly RE Jr, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545-52. [Crossref] [PubMed]
- Pilegaard HK. Extending the use of Nuss procedure in patients older than 30 years. Eur J Cardiothorac Surg 2011;40:334-7. [PubMed]
- Park HJ, Jeong JY, Jo WM, et al. Minimally invasive repair of pectus excavatum: a novel morphology-tailored, patient-specific approach. J Thorac Cardiovasc Surg 2010;139:379-86. [Crossref] [PubMed]
- Nuss D. Minimally invasive surgical repair of pectus excavatum. Semin Pediatr Surg 2008;17:209-17. [Crossref] [PubMed]
- Segal N, Robinson AE, Berger PS, et al. Chest compliance is altered by static compression and decompression as revealed by changes in anteroposterior chest height during CPR using the ResQPUMP in a human cadaver model. Resuscitation 2017;116:56-9. [Crossref] [PubMed]
- Handley AJ, Koster R, Monsieurs K, et al. European Resuscitation Council guidelines for resuscitation 2005. Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation 2005;67 Suppl 1:S7-23. [Crossref] [PubMed]
- Kleinman ME, Brennan EE, Goldberger ZD, et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132:S414-435. [Crossref] [PubMed]
- Duval S, Pepe PE, Aufderheide TP, et al. Optimal combination of compression rate and depth during cardiopulmonary resuscitation for functionally favorable survival. JAMA Cardiol 2019;4:900-8. [Crossref] [PubMed]
- Gruben KG, Guerci AD, Halperin HR, et al. Sternal force-displacement relationship during cardiopulmonary resuscitation. J Biomech Eng 1993;115:195-201. [Crossref] [PubMed]
- Yoganandan N, Pintar FA. Biomechanics of human thoracic ribs. J Biomech Eng 1998;120:100-4. [Crossref] [PubMed]
- Redlinger RE Jr, Rushing GD, Moskowitz AD, et al. Minimally invasive repair of pectus excavatum in patients with Marfan syndrome and marfanoid features. J Pediatr Surg 2010;45:193-9. [Crossref] [PubMed]
- Jaroszewski DE, Gustin PJ, Haecker FM, et al. Pectus excavatum repair after sternotomy: the Chest Wall International Group experience with substernal Nuss bars. Eur J Cardiothorac Surg 2017;52:710-17. [Crossref] [PubMed]
- Picton P, Walker D, White N, et al. Cardiopulmonary resuscitation following minimally invasive repair of pectus excavatum (Nuss technique). Resuscitation 2003;57:309-10. [Crossref] [PubMed]
- Lee KH, Kim KW, Kim EY, et al. Proper compression landmark and depth for cardiopulmonary resuscitation in patients with pectus excavatum: a study using CT. Emerg Med J 2015;32:301-3. [Crossref] [PubMed]
- Russo V, Ranno M, Nigro G. Cardiopulmonary resuscitation in pectus excavatum patients: is it time to say more? Resuscitation 2015;88:e5-6. [Crossref] [PubMed]
- Zou J, Luo C, Liu Z, et al. Cardiac arrest without physical cardiac injury during Nuss repair of pectus excavatum. J Cardiothorac Surg 2017;12:61. [Crossref] [PubMed]
- Glithero KJ, Tackett JJ, DeMason K, et al. Successful cardiopulmonary resuscitation following minimally invasive pectus excavatum repair: A case report. Int J Surg Case Rep 2019;65:255-8. [Crossref] [PubMed]
- Zoeller GK, Zallen GS, Glick PL. Cardiopulmonary resuscitation in patients with a Nuss bar--a case report and review of the literature. J Pediatr Surg 2005;40:1788-91. [Crossref] [PubMed]
- Nakahara O, Ohshima S, Baba H. Cardiopulmonary arrest during the Nuss procedure: case report and review. Acute Med Surg 2015;2:250-2. [Crossref] [PubMed]
- Beesems SG, Hardig BM, Nilsson A, et al. Force and depth of mechanical chest compressions and their relation to chest height and gender in an out-of-hospital setting. Resuscitation 2015;91:67-72. [Crossref] [PubMed]
- Remino C, Baronio M, Pellegrini N, et al. Automatic and manual devices for cardiopulmonary resuscitation: A review. Advances in Mechanical Engineering 2018;10:168781401774874. [Crossref]
- Tse KM, Tan LB, Lee SJ, et al. Feasibility of using computer simulation to predict the postoperative outcome of the minimally invasive Nuss procedure: Simulation prediction vs. postoperative clinical observation. J Plast Reconstr Aesthet Surg 2018;71:1496-506. [Crossref] [PubMed]
- Zhong W, Ye J, Liu J, et al. Numerical Simulation and Clinical Verification of the Minimally Invasive Repair of Pectus Excavatum. Open Biomed Eng J 2014;8:147-52. [Crossref] [PubMed]
- Kim D, Rhee D, Woo S, et al. Acute Mallory-Weiss syndrome after cardiopulmonary resuscitation by health care providers in the emergency department. Journal of Acute Disease 2015;4:335-7. [Crossref]
- Zhang S, Liu Q, Han S, et al. Standard versus Abdominal Lifting and Compression CPR. Evid Based Complement Alternat Med 2016;2016:9416908.
- Ewais MM, Chaparala S, Uhl R, et al. Outcomes in adult pectus excavatum patients undergoing Nuss repair. Patient Relat Outcome Meas 2018;9:65-90. [Crossref] [PubMed]


