Thyroid gland metastasis from small cell lung cancer: an unusual site of metastatic spread
Introduction
Thyroid gland metastasis is a rare event. Primary tumors that commonly metastasize to the thyroid include breast, lung, kidney and stomach carcinomas (1). Among lung cancer types causing thyroid metastasis, adenocarcinomas are the commonest followed by squamous and large cell carcinomas. Small cell lung carcinoma has not been frequently reported to cause thyroid metastatic deposits. In this report, we present a patient who developed metastatic thyroid lesions of a primary small cell lung cancer and concisely review the clinicopathological features and management of secondary thyroid tumors.
Case report
A 55-year-old male, heavy smoker (40 p/y) presented to our department with one month history of dry cough, exertional breathlessness, headache and mild gait disorder. His past medical history included non-insulin-dependent diabetes mellitus and one-vessel coronary artery disease under percutaneous transluminal coronary angioplasty (PTCA). Physical examination disclosed monophonic wheeze in the right hemithorax and a weakly positive Romberg’s sign without any other deficit. On head and neck palpation, a relatively large-sized non-tender and firm in consistency nodular lesion was detected in the right thyroid lobe without cervical lymphadenopathy. The rest of the clinical evaluation was unremarkable.
Admission chest radiograph showed a right perihilar tumor mass accompanied by a nodular opacity in the right upper lobe. Further imaging evaluation with contrast-enhanced computed tomography of the chest revealed a right hilar lymph node mass measuring 3 cm in diameter with associated bilateral mediastinal lymphadenopathy and a peripheral irregular infiltrate in the anterior segment of the right upper lobe.
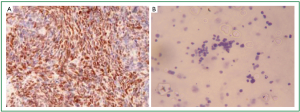
The patient underwent fiberoptic bronchoscopy showing thickening of mucosa over main carina and carina between bronchus to right upper lobe and bronchus intermedius. Radial 20 MHz EBUS (Olympus, UM-BS20-26R) with balloon catheter identified enlarged mediastinal lymph nodes as well as a solid peripheral lesion in the anterior segment of the right upper lobe. Submucosal biopsies, EBUS-guided transbronchial needle aspiration (TBNA) and transbronchial biopsies (TBB) were all positive for small cell lung cancer. Staging work-up using abdominal CT scan and brain magnetic resonance imaging (MRI) disclosed a solitary metastatic lesion in the right hemishpere of cerebellum with surrounding edema. Furthermore, thyroid ultrasound examination showed a relatively ill-defined heterogeneous mass measuring 65 mm × 55 mm × 48 mm in size located in the right lobe with sparse stippled calcifications and occasionally peripheral and central blood flow. Enlarged regional lymph nodes were also noted with obliteration of their normal ovoid morphology and loss of the echogenic hilum (Figure 1).
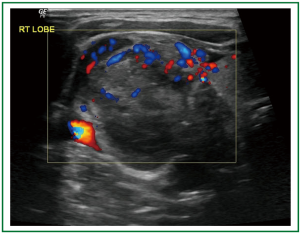
Ultrasonography-guided fine-needle aspiration cytology (US-FNAC) of the thyroid gland was carried out demonstrating a malignant neoplasm consisting of small-sized cells with ill-defined borders that were round-to-oval in shape, typically arranged in clusters with ‘‘molding of their nuclei’’(Figure 2A). On immunocytochemistry the neoplasmatic cells were stained strongly positive to synaptophysin, chromogranin-A (data not shown), CD56 and thyroid-transcription factor-1 (TTF-1) (Figure 2B,C,D). Based on these findings, the diagnosis of metastasis from small cell carcinoma of the lung was made and the disease was classified as stage IV (T1bN3M1b), accordingly.
Because of his good overall performance status (Eastern Cooperative Oncology Group PS:0), the treatment strategy included whole-brain radiotherapy (4,500 cGy/12 fractions) and concurrent administration of cisplatin and etoposide for six cycles. Following this regimen, a near-complete response was noted with residual thyroid lesion. However, the patient was recommended regular follow-up, and after 10 months of diagnosis the disease remains quiescent.
Discussion
Metastasis to the thyroid gland is a rare occurrence compared with the frequency of primary thyroid tumors (1). Clinically established incidence is less than 1% although it ranges from 3.9% to 24.2% based on autopsy studies (2). The most frequent tumors metastasizing to the thyroid comprise renal cell, breast, lung, esophageal and gastric carcinomas as well as melanoma (3). Metastatic thyroid tumors are commonly associated with concurrent metastatic lesions to other organs but they are rarely clinically noticeable. The reason for such a phenomenon is primarily the rapid development of the primary cancer.
Among histological types of lung cancer metastasizing to the thyroid, adenocarcinomas have been identified more frequently followed by squamous and large cell carcinomas (1,3,4). Isolated cases of small cell, combined small cell and large cell carcinoma, bronchioloalveolar carcinoma, adenosquamous carcinoma and pulmonary carcinoid tumor with thyroid metastatic deposits have also been reported (5,6).
Bronchogenic carcinomas of the small-cell undifferentiated type have been found to rarely cause thyroid metastasis. It is conjectured that this aggressive neoplasm, with a known propensity for early and wide blood-borne dissemination, would probably not present as a thyroid nodule. It is considered more likely that the hepatic, bony, brain or nodal metastases would present first and prompt appropriate investigation, rather than a solitary nodule in a thyroid. The present case refers to a patient with small cell lung cancer who developed metastatic lesions to the thyroid at the time the primary tumor was diagnosed. However, only one extremely rare case of primary small cell carcinoma of the thyroid gland has recently been described (7).
From a clinical standpoint, metastatic deposits in the thyroid may be asymptomatic or present with scant symptoms. Thyroid function tests are usually normal and substantially of little assistance in the diagnosis. Ultrasonography (US) usually shows focal or diffusely-infiltrating hypoechoic lesions; similarly, heterogeneous hypodense areas with mild contrast enhancement are observed on CT scans (8). However, calcifications including microcalcification, coarse calcification and peripheral calcification may represent one of the most specific US features of thyroid malignancy yielding a specificity of 85.8-95% and malignancy rate of 75% with regard to microcalcifications and coarse calcifications, respectively (9). They can exist independently within the lesions or can coexist as it occurred in the present case since coarse calcifications and microcalcifications were noted in the same thyroid lesion.
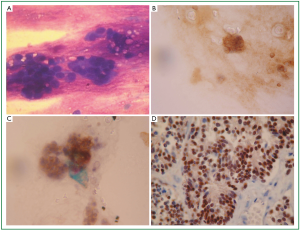
Metastatic tumors can easily masquerade as primary thyroid neoplasms. Fine-needle aspiration cytology (FNAC) is the initial procedure of choice in the evaluation of these patients (4). However, when FNAC findings are inconclusive, immunocytochemistry and electron microscopy are essential tools to make the distinction between primary and metastatic tumors. In the present case, the diagnosis was made based on distinct cytomorphologic features in conjunction with characteristic cell markers for neuroendocrine tumors. More specifically, tumor cells were stained positively for synaptophysin, chromogranin-A, CD56 and thyroid transcription factor 1 (TTF-1). These findings are often seen in cases of small cell lung carcinomas. Nevertheless, TTF-1 expression is highly specific for primary thyroid tumors. Immunoreactivity for calcitonin and thyroglobulin in thyroid lesion specimen was negative thus ruling out the existence of any primary thyroid tumor. Furthermore, our patient’s tumor was strongly positive for cytokeratine 8/18 (CK 8/18) and negative for cytokeratine 7 (CK 7) suggesting its lung origin (Figure 3A,B) (10).
In conclusion, the appearance of a new thyroid lesion in any patient with a known history of malignancy should be considered as potentially metastatic. Several thyroid lesions representing metastases might be overlooked because the physician’s attention is directed to more important lesions elsewhere, and thyroid examination is perfunctory.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Papi G, Fadda G, Corsello SM, et al. Metastases to the thyroid gland: prevalence, clinicopathological aspects and prognosis: a 10-year experience. Clin Endocrinol (Oxf) 2007;66:565-71.
- Lin JD, Weng HF, Ho YS. Clinical and pathological characteristics of secondary thyroid cancer. Thyroid 1998;8:149-53.
- Cichoń S, Anielski R, Konturek A, et al. Metastases to the thyroid gland: seventeen cases operated on in a single clinical center. Langenbecks Arch Surg 2006;391:581-7.
- Aron M, Kapila K, Verma K. Role of fine-needle aspiration cytology in the diagnosis of secondary tumors of the thyroid-twenty years’ experience. Diagn Cytopathol 2006;34:240-5.
- Osawa M, Takigawa N, Kiura K, et al. Isolated metastasis of lung cancer to the thyroid gland. Lung Cancer 2007;58:156-8.
- Maly A, Meir K, Maly B. Isolated carcinoid tumor metastatic to the thyroid gland: report of a case initially diagnosed by fine needle aspiration cytology. Acta Cytol 2006;50:84-7.
- Beach DF, Klump WJ, Haddad G, et al. Extrapulmonary small cell: a novel case of small cell carcinoma of the thyroid gland. Med Oncol 2012;29:1405-8.
- Ferrozz F, Campodonico F, De Chiara F, et al. Thyroid metastases: the echographic and computed tomographic aspects. Radiol Med 1997;94:214-9.
- Hoang JK, Lee WK, Lee M, et al. US features of thyroid malignancy: pearls and pitfalls. Radiographics 2007;27:847-60; discussion 861-5.
- Jagirdar J. Application of immunohistochemistry to the diagnosis of primary and metastatic carcinoma to the lung. Arch Pathol Lab Med 2008;132:384-96.