Pulmonary multislice computed tomography findings in acute aortic dissection
Abstract
Objective: To document the type and incidence of pulmonary multislice computed tomography (CT) findings at presentation in patients with acute aortic dissection.
Materials and methods: Multidetector CT scans of 36 patients with a diagnosis of acute aortic dissection or intramural hematoma were retrospectively reviewed.
Results: Pleural effusion, dependent stasis, mosaic attenuation, interlobular septal thickening, thickening of the peribronchovascular interstitium, vascular enlargement, compression atelectasis were common findings. Additionally air trapping, emphysema, consolidation, nodules, bronchiectasis or scarring were also noted.
Conclusions: Various pulmonary imaging findings may accompany acute aortic dissection. These findings and their clinical significance should be further investigated.
Key words: Acute aortic dissection; computed tomography; MDCT; lung
Introduction
The role of computed tomography (CT) in the diagnosis of acute aortic dissection is well known (1). In acute aortic dissection, type and extent of dissection together with presence of visceral perfusion deficits can confidently be evaluated using multidetector computed tomography (MDCT) (1). Studies regarding the use of CT in acute aortic dissection have mostly been focused on the vascular findings (1-3).
Lungs are commonly adversely affected from cardiovascular events and pulmonary complications may arise in critically ill patients (4). However, there is limited information on CT findings of the lungs in patients presenting with acute aortic dissection. Individual case reports present obstruction of a pulmonary artery due to the compressive effect of dissecting aneurysm which causes perfusion defect in the corresponding lung (5,6). Pleural effusion is documented to develop during the course of aortic dissection (7). Massive bullous emphysema and thickening of the peribronchovascular interstitium were also reported in association with aortic dissection (8-11).
The purpose of this study is to evaluate the type and incidence of pulmonary CT findings at presentation in patients with acute aortic dissection.
Materials and methods
Patients who had presented to our hospital between years January 2007- March 2010, and had a diagnosis of aortic dissection or intramural hematoma were searched from the computer based records of the hospital. This search revealed 134 patients whose CT images were stored on the picture archiving and communication system (Syngo XS, PACS, Siemens Medical Systems, Germany). Patients with chronic dissection (>14 days from the onset of symptoms) and those with undetermined time of onset (incidentally detected dissection on a CT scan performed for some other indication) were excluded. CT scans of patients who had acute dissection (≤14 days from the onset of symptoms) but undergone surgery already (replacement of the ascending aorta with/without the arch) were not included because it was not possible to evaluate the lungs completely due to early postoperative changes including extensive atelectases and pleural effusions. The CT examinations of the remaining 36 patients were retrospectively reviewed.
CT examinations were performed on a 16-detector MDCT (Somatom Sensation 16, Siemens, Erlangen, Germany) at the arterial phase following intravenous administration of 100 mL nonionic iodinated contrast agent (Iodixanol, Visipaque 320 mgI/mL, GE Healthcare, Milwaukee, Wisconsin, USA) into an antecubital vein with a power injector at a rate of 4 mL/s. The examination was initiated using a bolus tracking technique, 4 seconds after attenuation of the region of interest positioned in the ascending aorta reached 150 HU. The acquisition parameters were 120 kVp tube voltage, 270-315 mAs current, 16×0.75 mm collimation, 13.5 feed/rotation, and 420 msec gantry rotation time.
CT findings of the lungs as well as pleural effusions were noted. All dissections were classified according to the DeBakey system (type 1: Dissection involves the ascending aorta and extends into the descending aorta, type 2: Involves the ascending aorta only, type 3: Involves the descending aorta only) (12). The duration of time between the onset of symptoms and CT examination was also noted from the surgical notes in addition to the surgical findings of rupture.
Results
A total of 36 CT scans were reviewed, the patients consisted of 26 males and 10 females. The age of the patients at the time of CT scan ranged between 31 and 86 (mean: 61). The interval of time between the onset of symptoms and presentation of the patient to the emergency department ranged between 1 and 8 days (Mean±SD: 1.8±1.8). All CT scans were performed at the initial presentation of the patient to our hospital, 27 of these were performed within the first 24 hours (day 1) from the onset of symptoms. The evaluation of CT scans revealed intramural hematoma in 7 patients, while the remaining 29 patients demonstrated a dissection flap. A total of 10 patients had evidence of rupture at surgery including pericardial hemorrhage (n=9), pleural hemorrhage (n=3) and mediastinal hemorrhage (n=1). Eighteen patients had DeBakey type 1, 7 patients type 2, and 11 patients type 3 dissection.
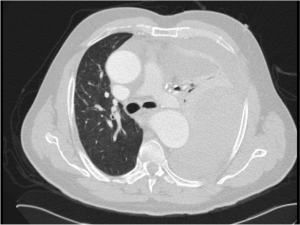
Pulmonary findings possibly related to acute dissection are demonstrated in Table 1. These include pleural effusion, dependent stasis, mosaic attenuation with ground glass density, interlobular septal thickening, thickening of the peribronchovascular interstitium and vascular enlargement as well as atelectasis and/or air trapping as a consequence of the dissection (Table 1, Figures 1,2,3,4).
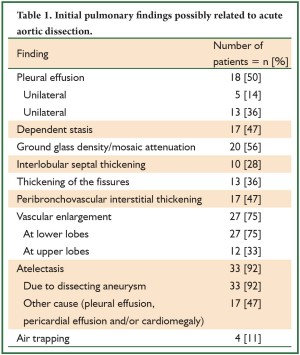
Full Table
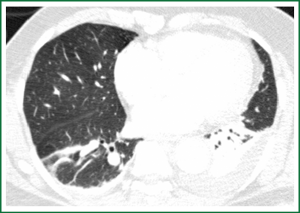
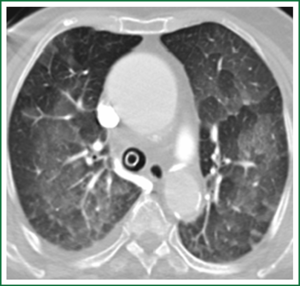
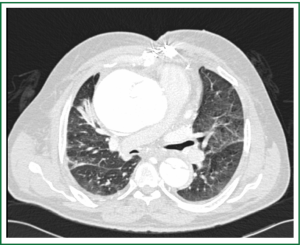
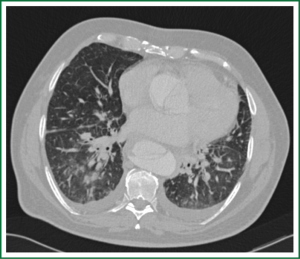
Atelectases were relaxation type secondary to dissecting aneurysm, pleural or pericardial effusions and/or cardiomegaly. All of the atelectases due to aneurysmal compression (n=33) were subsegmental, involving one or more lobes. Compression by causes other than the dissecting aneurysm resulted in subsegmental (n=16), segmental (n=3) and/or unilateral total pulmonary (n=1) atelectases in a total of 17 patients. Four patients had air trapping in the left (n=3) or right (n=1) lower lobe posterior basal segment secondary to the compression of the segmental bronchus by the descending aorta (Figure 4).
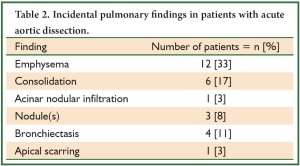
Incidental lung findings not considered directly related to the dissection are summarized in Table 2. Emphysema was demonstrated in 9 patients as centrilobular (n=6), paraseptal (n=2) or both (n=1). Three patients had an evidence of acute pulmonary infection by CT, including consolidation in 2 and acinar nodular infiltration in one patient. Single incidental nodule was found in one patient. One patient had a few and one multiple parenchymal nodules. Two patients had mild tubular bronchiectasis while one showed cystic and another significant traction bronchiectasis. One patient demonstrated extensive apical scarring accompanied by parenchymal distorsion and paracicatricial emphysema.
Full Table
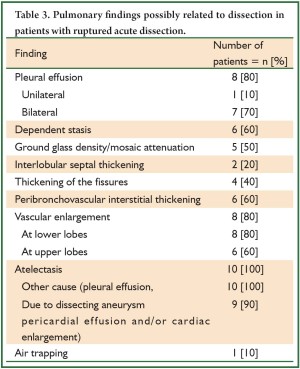
Table 3 demonstrates the findings of patients with evidence of ruptured dissection at surgery; including pleural effusion, stasis, mosaic attenuation due to ground glass areas, interlobular septal thickening, thickening of the fissures, thickening of the peribronchovascular interstitium, vascular enlargement, atelectases, including one patient with total left pulmonary collapse due to significant hemorrhage into the pleural space (Figure 5).
Full Table
Discussion
MDCT has significantly improved evaluation of aortic dissection and branch vessel involvement (1,13). MDCT has also been reported to provide superior image quality in evaluation of the lung parenchyma, especially in critically ill patients, by being capable of acquiring a large volume of information in a single breath hold and therefore, making a comprehensive diagnosis feasible in patients with suspected focal and diffuse lung disease (14). Our search of the literature revealed little information on CT findings of the lungs in patients with acute aortic dissection. Pleural effusion is known to develop during the course of aortic dissection (7). Obstruction of a pulmonary artery due to the compressive effect of dissecting aneurysm causing pulmonary perfusion defect, massive bullous emphysema and thickening of the peribronchovascular interstitium were also reported in association with aortic dissection in some case reports (5,6,8-11).
Pleural effusion, mosaic attenuation with ground glass densities, interlobular septal thickening, thickening of the peribronchovascular interstitium, and vascular enlargement are nonspecific CT findings suggesting hydrostatic pulmonary edema (12,15,16). In our series, one or more of these findings were noted in 32 patients, which could probably represent clinically evident or subclinical pulmonary edema. In our opinion, this could be due to the sudden change in vascular resistance and/or left ventricular afterload in patients with acute aortic dissection. As an alternative mechanism for the pulmonary edema, bronchial artery compromise by the dissection itself was suggested through development of lung ischemia (17). Whether this edema progresses later on and is responsible of the respiratory problems developing during the course of some patients should be investigated.
Lung findings secondary to compressive effects of the dissecting aneurysm should also be emphasized. Significant pericardial and/or pleural effusion caused subsegmental or segmental atelectasis in 17 of our patients in one or more lobes. Also subsegmental atelectasis along the course of dissecting aneurysm was noted in one or more lobes of 33 patients. In four patients, air trapping was found in left lower lobe posterior basal segment which was deemed secondary to the compression of aneurysmal descending aorta on the segmental bronchus. These atelectatic zones as well as air trapping may contribute to impaired oxygenation and respiratory insufficiency complicating the clinical course of some patients with aortic dissection. Compressive effects of the dissecting aneurysm are not limited to atelectasis and air trapping. Individual case reports present obstruction of a pulmonary artery which causes perfusion defect in the corresponding lung (5,6). However, we did not observe any pulmonary artery obstruction in our series.
Patients with ruptured dissection demonstrated more striking lung findings due to massive pleural effusions caused by hemorrhage into the pleural space and extensive relaxation atelectases due to the pleural or pericardial effusions. Thickening of the peribronchovascular interstitium was also reported as a manifestation of ruptured dissection and mediastinal hemorrhage previously (9-11). Significant thickening of the peribronchovascular interstitium was present in 6 of our patients with rupture as well as in 11 patients without rupture. As the cause of these findings, the differentiation between edema and rupture may be made depending on the presence of massive effusions as well as the clinical condition of the patient. Intramural hematoma has been suggested as an early stage or variant of aortic dissection (18). In our series, 6 patients had intramural hematoma, 5 of these were ruptured.
Other lung findings such as emphysema, bronchiectasis, active infection, or nodules were also noted as incidental findings in our series. Although considered to be not directly related to acute dissection, knowledge and appropriate management of these underlying disorders, may also have a role in the clinical management after immediate stabilization of the patient.
Conclusions
Various pulmonary CT findings may exist at initial presentation of patients with acute aortic dissection. These findings and their clinical significance should be investigated in larger series with clinical and radiological correlation.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Yoo SM, Lee HY, White CS. MDCT evaluation of acute aortic syndrome. Radiol Clin North Am 2010;48:67-83.
- Smith AD, Schoenhagen P. CT imaging for acute aortic syndrome. Cleve Clin J Med 2008;75:7-9, 12, 15-17 passim.
- Sebastià C, Pallisa E, Quiroga S, et al. Aortic dissection: diagnosis and follow-up with helical CT. Radiographics 1999;19:45-60, quiz 149-150.
- Webb WR. Pulmonary edema, the acute respiratory distress syndrome and radiology in the intensive care unit. In: Webb WR, Higgins CB, eds. Thoracic Imaging: Pulmonary and Cardiovascular Radiology, 1st ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2005:331-355.
- Neri E, Toscano T, Civeli L, et al. Acute dissecting aneurysm of the ascending thoracic aorta causing obstruction and thrombosis of the right pulmonary artery. Tex Heart Inst J 2001;28:149-51.
- Rau AN, Glass MN, Waller BF, et al. Right pulmonary artery occlusion secondary to a dissecting aortic aneurysm. Clin Cardiol 1995;18:178-80.
- Komukai K, Shibata T, Mochizuki S. C-reactive protein is related to impaired oxygenation in patients with acute aortic dissection. Int Heart J 2005;46:795-9.
- Kayrak M, Sonmez O, Vatankulu MA, et al. Completely asymptomatic proximal aortic dissection and massive bullous lung disease: coincidence or is there any etiologic link? Eur J Cardiothorac Surg 2009;35:1102-4.
- Muthu SK, Copley SJ. Case report: thickening of the peribronchovascular interstitium secondary to acute thoracic aortic dissection--chest radiograph and CT appearances. Clin Radiol 2008;63:236-8.
- Panicek DM, Ewing DK, Markarian B, et al. Interstitial pulmonary hemorrhage from mediastinal hematoma secondary to aortic rupture. Radiology 1987;162:165-6.
- Cao DB, Yang SR, Tong Q, et al. Interstitial pulmonary hemorrhage along the pulmonary artery secondary to ruptured aortic dissection. Intern Med 2010;49:1681-2.
- Brasileiro FC, Vargas FS, Kavakama JI, et al. High-resolution CT scan in the evaluation of exercise-induced interstitial pulmonary edema in cardiac patients. Chest 1997;111:1577-82.
- Vertinsky AT, Schwartz NE, Fischbein NJ, et al. Comparison of multidetector CT angiography and MR imaging of cervical artery dissection. AJNR Am J Neuroradiol 2008;29:1753-60.
- Schoepf UJ, Bruening RD, Hong C, et al. Multislice helical CT of focal and diffuse lung disease: comprehensive diagnosis with reconstruction of contiguous and high-resolution CT sections from a single thin-collimation scan. AJR Am J Roentgenol 2001;177:179-84.
- Storto ML, Kee ST, Golden JA, et al. Hydrostatic pulmonary edema: high-resolution CT findings. AJR Am J Roentgenol 1995;165:817-20.
- Ribeiro CM, Marchiori E, Rodrigues R, et al. Hydrostatic pulmonary edema: high-resolution computed tomography aspects. J Bras Pneumol 2006;32:515-22.
- Ventemiglia RA, Braverman B, Di Mauro J, et al. The ischemic lung: Role of the bronchial arteries in lung function. Cardiovasc Dis 1981;8:480-98.
- Yoshida S, Akiba H, Tamakawa M, et al. Thoracic involvement of type A aortic dissection and intramural hematoma: diagnostic accuracy--comparison of emergency helical CT and surgical findings. Radiology 2003;228:430-5.