Fixation of sternal fracture using absorbable plating system, three years follow-up
Introduction
Sternal fractures which account for approximately 3% to 8% of all recorded fractures (1,2), occur in patients facing major blunt anterior chest trauma, quite often due to car accidents, or direct high energy trauma to the front of chest. An indirect trauma from flexion compression of the spine or head injuries can result in severe unstable fractures of the sternum or multiple thoracic compression fractures. The lateral plain chest radiographs can reveal unstable fractures* (*, a break in continuity of bone caused by high force). The diagnoses of sternal fractures (especially small lineal fractures) can be difficult in anterioposterior chest X-rays, Computed tomography (CT) is more accurate to make the diagnosis and describe the morphology of the sternal fractures. CT scan may reveal associated intrathoracic injuries such as myocardial contusion, cardiac rupture, aortic dissection, pulmonary contusion, flail chest, rib and columna fractures. Usually sternal fractures are treated conservatively. Surgical correction should be considered in case of deformity, loss of sternal continuity, overlap, mobility of sternum, and presence of intractable pain.
Case report
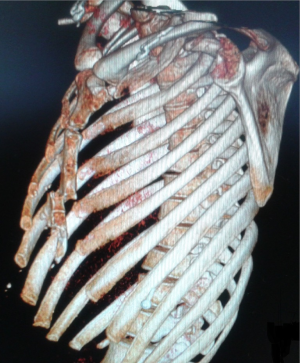
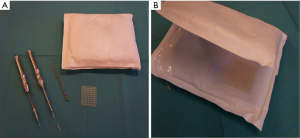
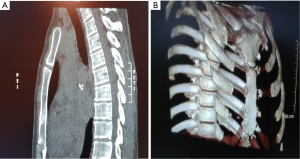
A 42-year-old woman was referred to our department after she had slipped from a 5-m high ladder falling direct on her anterior chest. She had severe pain and deformity of the sternum. CT scanning revealed a displaced 4th transverse ridge fracture of corpus sternum where the upper fragment slipped behind the lower part without any ribs or vertebral column injuries (Figures 1,2). The fracture was fixed by using an absorbable plate—LactoSorb® (42 mm × 42 mm large, 10×10 hole, 1.14 mm thick, fixed by six LactoSorb screws 11 mm long and 2 mm width). We performed a short midline longitudinal incision over the sternum and cleaned the site from hematoma to expose healthy bone without shortening sternum. We used two bone reduction forceps placed within the surrounding intercostal spaces to assist manual reduction of the fracture. The heated LactoSorb plate was shortened longitudinally and contoured manually to the underlying sternum and secured using three self drilling, self-tapping LactoSorb screws on each side (Figure 3A,B). A hot plate is soft but becomes hard in a few seconds when cooled at room temperature. We chose six (11 mm × 2 mm) LactoSorb screws as that was the thickness of the sternum measured on CT. We drilled with hand drill using adjustable stop bone tap. The tap was set to 11 mm to avoid deeper insertion. The wound was irrigated, a handy-vac drainage system was placed and incision was closed. The plate was only 1.14 mm thick and therefore was not visible or palpable under the skin. The handy-vac drainage system was removed 1st post-operative day. The patient was discharged from the hospital the 2nd post-operative day and returned to her work as physiotherapist after 3 weeks. CT-scan 3 years later revealed complete healing of the fracture (Figure 4A,B).
Discussion
Operative fixation of the sternal fractures was first described by Mckim in 1943 (3). He used a Kirschner wire. Several surgical techniques have been described during the past seven decades such as wires, nylon bands, Mersilene tape and locking plates. The most common stabilisation method is to use locking plates. In Ergene et al. studies indications for surgery were severe pain, dislocation with overlapping of sternal edges and thoracic wall instability (1). No major intra- or post-operative complication has been reported in the studies (2). Only a few articles have been published about surgical fixation of the sternum. A minority of sternal fractures require osteosynthesis. LactoSorb is a resorbable poly-L-lactic acid/polyglycolic acid copolymer, which provides desirable strength, comparable to that of titanium plating and it retains approximately 70% of its strength at 8 weeks (2). Kessler et al. used LactoSorb plates for rotator cuff repair in 45 patients with excellent postoperative result. LactoSorb plate maintained its strength during the healing period of the repair (4). Ricalde et al. compared the strength of six different resorbable plating systems using an in vitro model before and after heating them. LactoSorb performed the best with regard to the force required to cause a clinically significant displacement of 1 to 2 mm. He estimated the resorption time to be less than 1 year (5). Suuronen et al. performed mandibular osteotomies in sheep, and fixed them either with bioabsorbable poly-L-lactide or metallic dynamic compression plates. During the follow-up period of about 6 months, radiolographical, histological and microradiographical examinations at 6, 12, 24 weeks were performed. It has been shown that bony union with callus formation was accomplished by 6 weeks without any sign of plate failure. LactoSorb has a predictable resorption within 12-18 months (6), It has a low incidence of inflammatory and allergic reactions. Primarily, LactoSorb has been used in maxillofacial surgery. Our department has used it to fix sternum after osteotomy# (#, a surgical cut in bone to repair a deformity) in more than 150 pectus carinatum repair with excellent result. We experienced no operative or post operative complications. There has been no mortality, intensive admissions, plate failure, infection, pseudoarthroses or chronic pain. The hospital stay was about 2-3 days. Mollaoglu et al. investigated the early tissue response to titanium and LactoSorb screws and found that both materials can be used safely. The biodegradation of LactoSorb screws was not completed by the end of day 60. LactoSorb and titanium miniplates and screws are well tolerated and induced bone formation without causing adverse tissue response (7,8). Transverse metal plating systems may be dangerous when rapid sternal entry is required. By using resorbable plates instead of metallic systems one may reduce operations time, shorten hospital stay, sickness leave, provide better cosmetic results and avoid a second operation for removal of the implanted system, which may cause additional pain, discomfort and further complications.
Conclusions
Absorbable plates may be considered in fixation of traumatic sternal fractures as they have low incidence of failure, inflammation, and allergic reactions. They promote osteogenesis, and reduce the operation time. We report surgical fixation of a traumatic transverse sternal fracture using absorbable plate with an uneventful course. Sternal fixation with absorbable plates may require further investigation.
Acknowledgements
The authors thank professor Vibeke Hjortdal, associate professor Thomas D. Christensen for editorial and advisory assistance and Ninna Madsen for providing 3-D CT scan.
Disclosure: The authors declare no conflict of interest.
References
- Ergene G, Tulay CM, Anasız H. Sternal fixation with nonspecific plate. Ann Thorac Cardiovasc Surg 2013;19:364-7. [PubMed]
- Chou SS, Sena MJ, Wong MS. Use of SternaLock plating system in acute treatment of unstable traumatic sternal fractures. Ann Thorac Surg 2011;91:597-9. [PubMed]
- McKim LH. A method of fixation for fractures of the stern. Ann Surg 1943;118:168-60.
- Kessler KJ, Bullens-Borrow AE, Zisholtz J. LactoSorb plates for rotator cuff repair. Arthroscopy 2002;18:279-83. [PubMed]
- Ricalde P, Caccamese J, Norby C, et al. Strength analysis of 6 resorbable implant systems: does heating affect the stress-strain curve? J Oral Maxillofac Surg 2008;66:2493-7. [PubMed]
- Suuronen R, Pohjonen T, Vasenius J, et al. Comparison of absorbable self-reinforced multilayer poly-l-lactide and metallic plates for the fixation of mandibular body osteotomies: an experimental study in sheep. J Oral Maxillofac Surg 1992;50:255-62. [PubMed]
- Mollaoglu N, Cetiner S, Alpaslan C, et al. The early tissue response to titanium and LactoSorb screws. Dent Traumatol 2003;19:139-44. [PubMed]
- Wiltfang J, Merten HA, Schultze-Mosgau S, et al. Biodegradable miniplates (LactoSorb): long-term results in infant minipigs and clinical results. J Craniofac Surg 2000;11:239-43; discussion 244-5. [PubMed]



