When should large benign tumours in posterior mediastinum be resected?
Introduction
Benign tumours in the posterior mediastinum are often asymptomatic until they reach a considerable size and cause dysphagia or compression of the airways.
It remains controversial if an asymptomatic benign mediastinal tumour in an adults should be removed (1) or treated conservatively (watch-and-wait) (2) while symptomatic mediastinal tumours should be treated surgically (3). During 2010 three patients underwent resection of large benign tumours involving oesophagus at our institution.
Cases
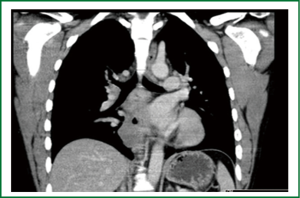
Patient number 1 was a 29 year old male with an oesophageal cyst of (4 cm × 5 cm × 11 cm) (Figure 1). His symptoms were dysphagia and he underwent thoracotomy with resection of a cyst in the muscular layer over a considerable portion of the oesophagus. His postoperative course was uneventful and he was discharged after 8 days. Histology demonstrated an oesophageal cyst and mediastinal sarcoidosis in an enlarged lymph node. He was seen in the outpatient clinic where he was well and asymptomatic.
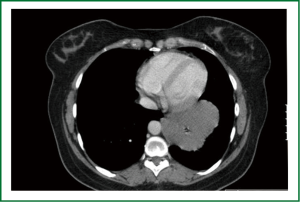
Patient number 2 was a 32 year old female with a bronchogenic cyst of (11 cm × 5 cm × 7 cm) (Figure 2). Her symptoms were dysphagia. She underwent thoracotomy with resection of a tumour infiltrating oesophagus only leaving mucosa after resection. Her postoperative course was complicated with leakage after 5 days and she underwent re-thoracotomy with primary repair of the leakage in oesophagus. Following a slow recovery she was discharged after 18 days and later seen in the outpatient clinic where she was well and asymptomatic.
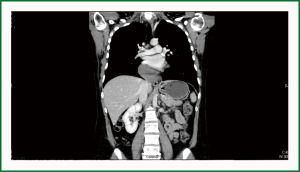
Patient number 3 was a 44 year female with an (18 cm × 4 cm × 5 cm) leiomyoma in the distal oesophagus (Figure 3). Her symptoms were dysphagia and regurgitation. She underwent thoracotomy with resection of a tumour in the distally oesophagus leaving only the mucosa after resection. Her postoperative course was complicated with leakage and she was initially treated endoscopic with a covered oesophageal stent but because of persistent leakage we performed a re-thoracotomy with T-tube drainage of oesophagus. Following a long recovery she was finally discharged after 78 days. She was later seen in outpatient clinic and was found in well conditions without symptoms.
Discussion
The present study demonstrates that surgery of large posterior mediastinal masses may be associated with high postoperative morbidity and risk of a long hospitals stay. Technically it is easier to remove a small tumour than a large tumour, but these patients are often asymptomatic and therefore the tumours are rarely found before the patients become symptomatic. If an asymptomatic benign tumour has been diagnosed the treatment is somewhat controversial: Some centers prefer a strategy of “watch-and-wait” (1) while others advocate early surgery because 45% of asymptomatic patients eventually develop symptoms (4).
With the advances in minimally invasive surgery the video-assisted-thoracoscopic (VATS) technique is thought to be as safe and effective as open surgery (5) but even though we are a high volume VATS center we would advocate for open surgery for tumours of a considerable size because the advantage with VATS surgery are lost with increasing size as it has been seen in VATS surgery for pulmonary cancer.
Complication rates have been reported from 0-27% (4) but major morbidity or mortality in the surgical treatment of mediastinal cysts has not been reported. The term major morbidity has not been clearly defined in the literature but we believe it should include any complication with postoperative leakage from the esophagus as seen in two out of three patients in our small series.
Generally it is recommended that patients with leakage are treated with primary repair regardless of the time to presentation and esophagectomy is reserved for patients with an underlying cancer or extensive transmural necrosis while only a small carefully selected group of patients may be treated successfully without operation (6).
We treated one patient surgically with re-thoracotomy and primary repair. The other patient was treated endoscopic with implantation of a covered stent in distally oesophagus but she had persistent leakage after replacement of the stent two so we finally did re-thoracotomy with T-tube drainage of oesophagus with good effect.
In conclusion, we believe that symptomatic patients with large benign tumours should be referred directly for surgery independent of size while asymptomatic patients should be followed regularly and referred for surgical treatment if their tumour increases in size because surgery may be hazardous as size of the tumour increases and more likely to be associated with major postoperative morbidity.
Statement
We confirm that there has been no duplicate publication or submission elsewhere. In addition, all authors have read and approved the manuscript. Subject to acceptance, the authors will transfer copyright to the Publisher and there is no ethical problem or conflict of interest. There has been no funding.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Ponn RB. Simple mediastinal cysts: resect them all? Chest 2003;124:4-6.
- Bolton JW, Shahian DM. Asymptomatic bronchogenic cysts: what is the best management? Ann Thorac Surg 1992;53:1134-7.
- Cioffi U, Bonavina L, De Simone M, et al. Presentation and surgical management of bronchogenic and esophageal duplication cysts in adults. Chest 1998;113:1492-6.
- Kirmani B, Kirmani B, Sogliani F. Should asymptomatic bronchogenic cysts in adults be treated conservatively or with surgery? Interact Cardiovasc Thorac Surg 2010;11:649-59.
- Lang-Lazdunski L, Pilling J. Videothoracoscopic excision of mediastinal tumors and cysts using the harmonic scalpel. Thorac Cardiovasc Surg 2008;56:278-82.
- Port JL, Kent MS, Korst RJ, et al. Thoracic esophageal perforations: a decade of experience. Ann Thorac Surg 2003;75:1071-4.