
Does routine uniportal thoracoscopy during rib fixation identify more injuries and impact outcomes?
Introduction
Flail chest and severely displaced rib fractures due to blunt trauma are associated with significant morbidity and mortality, especially with concurrent intrathoracic injuries (1,2). The presence of more than three rib fractures in adults has been shown to be marker for associated solid visceral trauma (3). The incidence of associated hemothorax, lung laceration, lung hernia, and diaphragmatic injury have been previously described in rib fracture studies, as well as the potential for complications and reoperations if left undetected (4-6). Most commonly, retained hemothoraces can be present in approximately 50% of patients at the time of surgical stabilization of rib fractures (SSRF) with approximately 25% of these patients at risk for development of empyema (7,8). Though computed tomography (CT) scan capabilities have improved trauma evaluation, they do not identify all intrathoracic injuries. CT scans have a 95% sensitivity in detecting most major and minor thoracic injuries within six hours of blunt trauma, but only a 70–90% sensitivity in detecting traumatic diaphragmatic injuries (9,10).
The use of exploratory thoracoscopy for both diagnosis and treatment in trauma patients with intrathoracic injuries is increasing (11). Video-assisted thoracoscopic surgery (VATS) first emerged in the mid-1990s as a minimally invasive tool to perform anatomic lung resections but has gained in popularity with experience. Advantages to VATS include decreased pain, shorter length of stay (LOS), decreased blood loss, and decreased morbidity and mortality (12,13). Approximately 45% of anatomic lung resections in the United States are performed with VATS techniques (14). More recently, single port VATS, or uniportal thoracoscopy, has emerged as an effective tool for performing anatomic lung resection, management of pleural effusions, and debridement of hemothorax or empyema using angled instruments that can be used together with a camera via a single small intercostal incision (15,16).
At our institution, two thoracic surgeons perform all rib fracture repairs: one performs routine uniportal thoracoscopy (R-VATS) at the time of surgery and other only for select cases based on imaging and surgeon discretion (S-VATS). In this pilot study, we examined the rates of associated intrathoracic injuries and hypothesized that R-VATS at time of SSRF identifies and addresses a greater number of intrathoracic injuries not seen on CT scan and may impact outcomes.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-2087).
Methods
Study population
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by University of North Carolina’s institutional review board (IRB-17-2030) and individual consent for this retrospective analysis was waived.
We retrospectively reviewed all patients who underwent SSRF from 2013 to 2019 by the thoracic surgery service at the University of North Carolina Hospitals Level I Trauma Center for multiple displaced rib fractures or flail chest using ICD-9 and ICD-10 codes.
Exposure and outcome variables
Data collected included basic patient demographics, mechanism of injury, as well as dates of injury, admission, surgery and discharge. The number of displaced rib fractures and any intrathoracic injuries were identified by thoracic radiologists on pre-operative imaging. Members of the thoracic surgery team retrospectively reviewed the imaging for data fidelity. Operative data such as the use of VATS, intraoperative findings, length of operation, and number of ribs repaired were also collected. The primary outcome of interest was the number of additional intrathoracic injuries identified on thoracoscopy at the time of SSRF and not seen on CT scan. Secondary outcome of interests included hospital and intensive care unit (ICU) LOS, readmissions, reoperations, intubation, mechanical ventilation days, and overall mortality.
Statistical analysis
Descriptive analyses were performed to determine proportions of incidental intrathoracic injuries overall and by categories of R-VATS or S-VATS. Chi-square tests and t-tests were used to compare outcomes between SSRF/thoracoscopy and SSRF only groups. All analyses were performed using Stata software, version 15 (StataCorp).
Surgical technique
At our institution, uniportal exploratory thoracoscopy is performed using lung isolation with a double lumen endotracheal tube or bronchial blocker placed through an existing single lumen endotracheal tube. If the patient had a previously placed chest tube, this is removed following induction of general anesthesia and lung isolation. A 3-cm incision is made anterior to the iliac spine in the 6th intercostal space. A 10-mm 30-degree thoracoscope is inserted via a 12-mm port and the pleural space examined. Lung graspers are inserted through the single incision to assist with lung retraction and visual inspection of the entire chest cavity and diaphragm. A sucker can also be inserted through the incision to aspirate any undrained fluid and/or blood. Injuries to the lung are addressed in most instances by insertion of an endostapler and lung grasper via the single port incision alongside the camera. Additional port incisions are made as needed, generally along the planned incision to be used for rib fracture repair. The chest is irrigated with copious amounts of warm saline and a 28-Fr chest tube is placed in the single port incision. SSRF is then begun with a muscle-sparing incision when possible.
Results
Patient characteristics
Ninety-nine patients (27% female, 73% white, median age 56) underwent SSRF during the study period (Table 1). The most common mechanism of injury was blunt trauma (94%). Forty-two percent of patients had a flail chest. On average, patients presented to our institution with five displaced rib fractures and a median injury severity score (ISS) was 14. The median time between admission to the trauma service and thoracic surgery consultation was 2 days. Sixty-one patients received thoracostomy tubes, most commonly for hemopneumothorax (41%), prior to a thoracic surgery consult. Preoperative CT scan identified the following injuries that were subsequently treated at the time of SSRF: lung laceration (12.1%), lung hernia (5.1%), and retained hemothorax (46.5%).
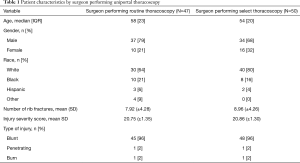
Full table
Missed findings on routine vs. selective uniportal thoracoscopy
The surgeon that performs R-VATS at the time of surgery completed 49 SSRF, while the other who performs S-VATS completed 50 SSRF cases. There was no difference between ISS among the groups. Uniportal thoracoscopy was performed on a total of 69% patients at the time of SSRF with 21 and 47 patients that underwent S-VATS and R-VATS, respectively. The two patients that did not undergo thoracoscopy by the R-VATS surgeon was due to massive hemorrhage requiring urgent exploratory thoracotomy. When thoracoscopy was performed, 31 additional injuries were identified including 7 lung lacerations (22.6%), 4 lung hernias (12.9%), 18 retained hemothoraces (58.1%), and 2 diaphragmatic hernias (6.5%) (Table 2). R-VATS identified 23 additional intrathoracic findings at time of thoracoscopy not seen on CT scan compared to 8 findings in the S-VATS group (P=0.367). Of the 31 additional injuries, all, with the exception of one lung laceration, subsequently underwent wedge resection, hernia reduction, hemothorax evacuation, or diaphragm repair. The patient with the untreated lung laceration had a longer ICU LOS (10 days) and ventilatory support days (5 days) compared to the average ICU LOS and ventilatory support days determined in our study population (Table 3). The patient’s ISS was also lower than the average ISS (17 vs. 20, Table 1). Forty-four percent of these repairs required an additional port incision.
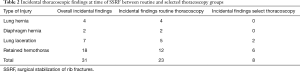
Full table
Full table
Thoracoscopy use vs. no thoracoscopy use
Two patients required readmission and reoperation within three months, neither of which underwent thoracoscopy at the time of SSRF. One patient presented with an empyema and the other a large left diaphragmatic hernia. The patient readmitted with an empyema initially presented from a motor vehicle collision (MVC) with multiple injuries including: a sternal fracture, bilateral rib fractures of the first, 10th, and 12th ribs, thoracic spinous process fractures, and a right acetabular fracture. Similarly, the patient requiring a reoperation for a left diaphragmatic hernia repair presented after an MVC with flail chest, bilateral fractures of the left 3–8 posterior ribs and right 4th, 5th, and 7th posterior ribs, hemothorax, a thoracic lamina fracture, pubic rami fractures, and right iliac and sacral fractures.
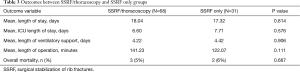
There was no difference in average LOS and ICU LOS between the SSRF/thoracoscopy and SSRF only groups (P=0.814, 95% CI: −6.79, 5.35, and P=0.576, 95% CI: −2.81, 5.02, respectively) (Table 3). There was also no difference in the need for intubation (χ2=0.378, P=0.538). When mechanical ventilation was required, total ventilatory days were the same among SSRF/thoracoscopy and SSRF only groups (P=0.906, 95% CI: −3.26. 3.67). No difference in operative time with or without thoracoscopy (P=0.111, 95% CI: −42.80, 4.46) was observed. Three patients died in the SSRF/thoracoscopy group, while two patients died in the SSRF only group (P=0.667). The patients in the SSRF/thoracoscopy group were >65 years of age with an ISS of 9, 19, and 24 and multiple co-morbidities. ISS of the patients who died in the SSRF only group were 17 and 41. Cause of death in both groups was the result of comfort care measures in the setting of a complicated hospital course with declining respiratory function.
Discussion
Uniportal VATS has been shown to have a limited operative time, a low conversion rate to conventional VATS or mini thoracotomy, and decreased post-operative pain and paresthesia with low morbidity and mortality (15,17). In a large retrospective review by Rocco et al., in which patients underwent uniportal VATS for diagnosis and management of pleural effusions, non-anatomic wedge resections, and debridement of hemothorax and empyema, 3.7% of patients were converted to conventional VATS or mini thoracotomy. The mortality rate was 0.6% (15). Our study conversion rate and mortality rate were higher than Rocco et al.’s; however, we suspect this is a due our study population of trauma patients.
Exploratory uniportal VATS of the pleural space at time of SSRF permits the surgeon to discover and address any chest tube-related complication that may exist (parenchymal tears and lacerations) and any undrained or retained hemothorax. Injuries such as lung laceration, lung hernia, and diaphragmatic hernia discovered during exploration can be repaired via the single incision or additional port incisions as needed. Injuries such as traumatic diaphragmatic hernia or tracheobronchial injuries can be repaired via the rib fracture access incision. In addition, the rib fracture pattern can be assessed from the pleural space which aids in tailoring an optimal muscle-sparing incision to address rib fractures.
Our study also demonstrated the utility of uniportal VATS in detecting occult intrathoracic injuries. Uniportal R-VATS at the time of SSRF identified a greater number of occult intrathoracic injuries not identified on CT scan compared to S-VATS, though this was not statistically significant. Although the superiority of CT scan compared to chest radiography in diagnosing chest trauma is well-documented, polytrauma patients are still admitted with missed intrathoracic injuries (18,19). Banaste et al. examined radiologic and clinical markers predictive of missed injuries of trauma patients on whole-body CT scans and identified that patients 30 years or older or have more than two injured anatomical locations are at higher risk of missed injuries identified on the first CT examination (20). The two patients requiring reoperation in our study shared these same features, ultimately resulting in readmission and reoperation.
The first patient was a missed diaphragmatic hernia due to blunt trauma three months prior. Diaphragmatic injuries due to chest trauma are a commonly missed diagnosis, in part due to the low sensitivity of X-rays and CT imaging in the early stages of injury (21,22). False negative results occur due to lack of adequate visualization of the dome of the diaphragm or an obstructed view of the diaphragm in patients with concomitant hemothorax or intraabdominal hemorrhage (23). On initial CT imaging, our patient with a missed diaphragmatic hernia had bilateral hemothoraces. A left diaphragmatic hernia was diagnosed three months later, when the patient presented with epigastric pain and signs of intestinal obstruction. Patients can remain asymptomatic for months or years before presenting with complications, such as incarceration or strangulation of a hollow visceral organ, requiring surgical intervention (4,24). Patients with late cases of diaphragmatic hernias can exhibit a variety of symptoms, such as abdominal pain, dyspnea, or symptoms of intestinal obstruction (4). Due to the relative weakness of the left hemi-diaphragm and the protective effect of the liver on the right, most diaphragmatic hernias occur on the left side (4,25). A high level of suspicion for diaphragmatic injury should be maintained in patients following blunt trauma and present with low rib fractures. The low fractured rib fragment may act as a sharp object that penetrates the adjacent diaphragm mimicking that of a penetrating trauma (26). Powell et al. performed a single center retrospective review of 566 patients with traumatic rib fractures who underwent routine thoracoscopy at time of surgery and found 23 diaphragmatic injuries, 55% of which had been not identified on preoperative imaging (27). The authors concluded that the mechanism of diaphragmatic injury was a penetrating type injury from the fractured segments of the lower ribs.
The second case was an empyema requiring pulmonary decortication as a result of a retained hemothorax. We hypothesize this was a consequence of incomplete drainage of the pleural space by the emergently placed chest tube at primary survey. Chest tubes placed upon admission to the emergency room or trauma bay are routinely removed in the operating room and their insertion incisions irrigated/debrided and closed with interrupted sutures. This is because these tubes in particular carry a substantial risk of insertion site infections and empyema (28). Complication rates of chest tubes placed in an emergency setting can be as high as 37% and consist of insertional, positional, and infective types of complications, with positional-related complications being most common (29-31). Retained hemothorax can be present in approximately 50% of patients at the time of SSRF with about 25% developing an empyema (7,8). DuBose et al. found that the presence of rib fractures was an independent predictor for the development of empyema in patients with posttraumatic retained hemthoraces (7). In addition to increased risk of empyema, retained hemothoraces can increase ICU and hospital LOS (7). In a prospective, randomized controlled trial by Meyer et al., patients treated only with thoracostomy tube for traumatic retained hemothoraces often required further intervention with VATS (32). Early intervention with VATS, specifically within four days, decreased the duration of thoracostomy tube placement, ventilatory days, and hospital and ICU LOS (32,33).
In addition to diaphragm injuries and retained hemothoraces, both R-VATS and S-VATS incidentally found lung hernias and lacerations at the time of SSRF—though at a higher rate in the R-VATS group. Similar to retained hemothorax, untreated lung lacerations can cause higher rates of infection and increased duration of thoracostomy tube placement, ventilatory days, hospital and ICU LOS (6).
Our study detected no differences in hospital and ICU LOS, operative time, need for mechanical ventilation, and overall mortality between SSRF/thoracoscopy and SSRF only groups. This suggests that there is no additional risk or increased operative time with performing R-VATS at the time of SSRF.
Limitations
There are several limitations to this study. First, this was a retrospective single-center study with a small sample size. Due to the limited sample size, our study is underpowered to detect small differences between groups. Further, readmissions outside of our medical system are not captured as they are not linked to our electronic medical record, which is expected to bias results towards the null (i.e., underestimate the magnitude of our missed intrathoracic estimates). Despite these limitations, we believe our pilot study provides valuable information in the context of R-VATS in the management of SSRF. Future study on this matter is needed and may be best tested in a multi-institutional setting.
Conclusions
R-VATS at the time of SSRF did not identify a statistically significant greater number of occult intrathoracic injuries compared to S-VATS. Though our results may be restricted by a limited sample size, two missed findings in patients who did not undergo thoracoscopy at the time of SSRF required readmission and reoperation. In addition, R-VATS is not associated with increased operative time, LOS, or mortality.
Since reviewing our data, the surgeon that performs selective VATS has been more critical regarding injuries not identified on initial CT imaging. Therefore, the surgeon has been more insistent about performing exploratory thoracoscopy during the surgical management of rib fractures. More study, such as a prospective multi-institutional trial, is needed to determine if there is any benefit to a routine VATS approach in patients meeting requirements for rib fracture repair.
Acknowledgments
Chest Wall Injury Society Summit 2020, Podium Presentation.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-2087
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-2087
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-2087). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by University of North Carolina’s institutional review board (IRB-17-2030) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Albers JE, Rath RK, Glaser RS, et al. Severity of intrathoracic injuries associated with first rib fractures. Ann Thorac Surg 1982;33:614-8. [Crossref] [PubMed]
- Ciraulo DL, Elliott D, Mitchell KA, et al. Flail chest as a marker for significant injuries. J Am Coll Surg 1994;178:466-70. [PubMed]
- Lee RB, Bass SM, Morris JA Jr, et al. Three or more rib fractures as an indicator for transfer to a Level I trauma center: a population-based study. J Trauma 1990;30:689-94. [Crossref] [PubMed]
- Davoodabadi A, Fakharian E, Mohammadzadeh M, et al. Blunt Traumatic Hernia of Diaphragm With Late Presentation. Arch Trauma Res 2012;1:89-92. [Crossref] [PubMed]
- Su YH, Yang SM, Ko HJ. Diagnosis and management of a trapped lung or diaphragm by fractured ribs: analysis of patients undergoing rib fracture repair. BMC Surg 2019;19:123. [Crossref] [PubMed]
- Chou YP, Kuo LC, Soo KM, et al. The role of repairing lung lacerations during video-assisted thoracoscopic surgery evacuations for retained haemothorax caused by blunt chest trauma. Eur J Cardiothorac Surg 2014;46:107-11. [Crossref] [PubMed]
- DuBose J, Inaba K, Demetriades D, et al. Management of post-traumatic retained hemothorax: A prospective, observational, multicenter AAST study. J Trauma Acute Care Surg 2012;72:11-22; discussion 22-4; quiz 316.
- Pieracci FM, Lin Y, Rodil M, et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg 2016;80:187-94. [Crossref] [PubMed]
- Boulanger BR, Milzman DP, Rosati C, et al. A comparison of right and left blunt traumatic diaphragmatic rupture. J Trauma 1993;35:255-60. [Crossref] [PubMed]
- Zinck SE, Primack SL. Radiographic and CT findings in blunt chest trauma. J Thorac Imaging 2000;15:87-96. [Crossref] [PubMed]
- Salati M, Brunelli A, Rocco G. Uniportal video-assisted thoracic surgery for diagnosis and treatment of intrathoracic conditions. Thorac Surg Clin 2008;18:305-10. [Crossref] [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Onaitis MW, Petersen RP, Balderson SS, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg 2006;244:420-5. [PubMed]
- Cools-Lartigue J, Park B. Economic assessment in minimally invasive thoracic oncological surgery—USA experience. Shanghai Chest 2018;2:89. [Crossref]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [Crossref] [PubMed]
- Rocco G. Single-Port Video-Assisted Thoracic Surgery (Uniportal) in the Routine General Thoracic Surgical Practice. Oper Tech Thorac Cardiovasc Surg 2009;14:326-35. [Crossref]
- Wang L, Liu D, Lu J, et al. The feasibility and advantage of uniportal video-assisted thoracoscopic surgery (VATS) in pulmonary lobectomy. BMC Cancer 2017;17:75. [Crossref] [PubMed]
- Chardoli M, Hasan-Ghaliaee T, Akbari H, et al. Accuracy of chest radiography versus chest computed tomography in hemodynamically stable patients with blunt chest trauma. Chin J Traumatol 2013;16:351-4. [PubMed]
- Trupka A, Waydhas C, Hallfeldt K, et al. Value of thoracic computed tomography in the first assessment of severely injured patients with blunt chest trauma: results of a prospective study. J Trauma 1997;43:405-11. [Crossref] [PubMed]
- Banaste N, Caurier B, Bratan F, et al. Whole-Body CT in Patients with Multiple Traumas: Factors Leading to Missed Injury. Radiology 2018;289:374-83. [Crossref] [PubMed]
- Hanna WC, Ferri LE, Fata P, et al. The current status of traumatic diaphragmatic injury: lessons learned from 105 patients over 13 years. Ann Thorac Surg 2008;85:1044-8. [Crossref] [PubMed]
- Payne JH Jr, Yellin AE. Traumatic diaphragmatic hernia. Arch Surg 1982;117:18-24. [Crossref] [PubMed]
- Van Hise ML, Primack SL, Israel RS, et al. CT in blunt chest trauma: indications and limitations. Radiographics 1998;18:1071-84. [Crossref] [PubMed]
- Reber PU, Schmied B, Seiler CA, et al. Missed Diaphragmatic Injuries and Their Long-Term Sequelae. J Trauma 1998;44:183-188. [Crossref] [PubMed]
- Ganie FA, Lone H, Lone GN, et al. Delayed Presentation of Traumatic Diaphragmatic Hernia: a Diagnosis of Suspicion with Increased Morbidity and Mortality. Trauma Mon 2013;18:12-6. [Crossref] [PubMed]
- Kim S, Choi W, Lee K, et al. The clinical implications of severe low rib fracture in the management of diaphragm injury: A Case Control Study. Int J Surg 2017;42:178-82. [Crossref] [PubMed]
- Powell L, Chai J, Shaikh A. Experience with acute diaphragmatic trauma and multiple rib fractures using routine thoracoscopy. J Thorac Dis 2019;11:S1024-S1028. [Crossref] [PubMed]
- Sethuraman KN, Duong D, Mehta S, et al. Complications of Tube Thoracostomy Placement in the Emergency Department. J Emerg Med 2011;40:14-20. [Crossref] [PubMed]
- Bailey RC. Complications of tube thoracostomy in trauma. J Accid Emerg Med 2000;17:111-4. [Crossref] [PubMed]
- Bertoglio P, Guerrera F, Viti A, et al. Chest drain and thoracotomy for chest trauma. J Thorac Dis 2019;11:S186-S191. [Crossref] [PubMed]
- Harris A, O’Driscoll B, Turkington P. Survey of major complications of intercostal chest drain insertion in the UK. Postgrad Med J 2010;86:68-72. [Crossref] [PubMed]
- Meyer D, Jessen M, Wait M, et al. Early evacuation of traumatic retained hemothoraces using thoracoscopy: a prospective, randomized trial. Ann Thorac Surg 1997;64:1396-400; discussion 1400-1. [Crossref] [PubMed]
- Huang FD, Yeh WB, Chen SS, et al. Early Management of retained hemothorax in blunt head and chest trauma. World J Surg 2018;42:2061-6. [Crossref] [PubMed]


