
Comparing the rate of fiberoptic bronchoscopy use with a video double lumen tube versus a conventional double lumen tube—a randomized controlled trial
Introduction
Single lung ventilation is necessary for many thoracic surgeries in order to expose the surgical field while allowing normal ventilation in the non-operative lung (1). There are several ways to provide single lung ventilation during thoracic surgery, but the double lumen endotracheal tube (DLT) is considered the gold standard. A conventional DLT (c-DLT) consists of a proximal tracheal end and a distal bronchial end, which extends into either the left or right main stem bronchus. Previous studies have shown that the c-DLT allows for faster placement, better lung isolation, and more accurate positioning when compared to other methods such as bronchial blockers (2,3). A fiberoptic bronchoscope (FOB) can be inserted through the c-DLT to confirm that it is accurately positioned. While it is possible to correctly place a c-DLT without an FOB using auscultation alone, this method can be unreliable, and an FOB is typically used to confirm placement (4). The estimated price of a c-DLT is between $35.41–48.00 (5,6). Accounting for maintenance and processing costs, the price of a reusable FOB ranges from $89.43–312.20 per procedure (5,6).
Malpositioning of a DLT during single lung ventilation can lead to detrimental changes in lung function, including poor ventilation, hypoxemia, and air leak (7,8). Time spent repositioning the DLT can be crucial, given that these patients frequently have poor pulmonary function. Multiple studies have shown a high incidence of c-DLT malpositioning (35–48%) requiring repositioning, even when inserted by experienced providers (9,10). Continuous visualization of the tube would be expected to decrease the incidence of DLT malposition, and therefore reduce the time spent verifying tube placement (5).
The VivaSight DLT (VS-DLT) (Ambu, Columbia, MD, USA) is a single-use DLT that incorporates an embedded camera and light source between the tracheal and bronchial cuffs, thus permitting continuous visualization of the tube’s position. It also has an integrated flushing system that allows for intratracheal cleaning of the camera lens should the lens become obstructed by secretions or blood. When correctly positioned, the camera on a VS-DLT is focused on the carina, providing constant visual confirmation of the bronchial cuff in the left mainstem bronchus (10,11). Compared to a c-DLT, continuous visualization using a VS-DLT can significantly reduce the need for an FOB. In prior studies, the cost of a VS-DLT was reported to be between $225–300 (5,6).
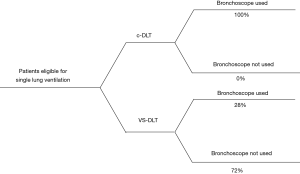
The primary objective of this prospective, randomized, controlled study was to assess the incidence of FOB usage between patients who were intubated with a c-DLT versus a VS-DLT. We hypothesized that an FOB would be required in 100% of c-DLT subjects and in 20% of VS-DLT subjects (12). Secondary endpoints included time to correct tube placement and the incidence of malpositioning during surgery. We hypothesized that time to correct tube placement would be faster with the VS-DLT and that the incidence of malpositioning would be significantly less with the VS-DLT. We present the following article in accordance with the CONSORT 2010 reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-1595).
Methods
Study design and patient population
This randomized, prospective, controlled study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and approved by the University of Texas Southwestern Medical Center Institutional Review Board and was registered at clinicaltrials.gov (NCT 03690284, date of registration 10/01/2018). Between July 2019 and February 2020, a total of 50 subjects were enrolled. All patients gave informed consent to participate in the study. Inclusion criteria were as follows: 18–90 years old, scheduled for a thoracic surgery requiring single lung ventilation, and not emergent. Exclusion criteria included pregnant or nursing women, patients with known or suspected difficult airway, and patients with a contraindication for left-sided DLT insertion (e.g., left-sided bronchial mass). We ended the study once we achieved our goal of 50 patients.
Outcomes
The primary outcome was the effect of DLT type on the rate of FOB usage. Secondary endpoints included the time to correct tube placement, the incidence of malpositioning during surgery, and the ability to predict malpositioning when using either a VS-DLT or a c-DLT. The DLT placement time was defined as the time from the start of laryngoscopy to the time that the bronchial lumen of the DLT was successfully visualized within the left mainstem bronchus. All outcomes were measured intraoperatively.
Randomization
A total of 50 opaque sequentially numbered randomization envelopes were prepared using a random number generator by a non-clinical member of the research team. Each envelope contained a card that read “c-DLT” or “VS-DLT.” Although patients were not aware of their randomized treatment group, it was not feasible to blind anesthesiologists performing the intubation.
Protocol
In the operating room, standard American Society of Anesthesiologists (ASA) monitors were applied. Subjects underwent induction of anesthesia according to a standardized protocol consisting of fentanyl, propofol, and lidocaine. Neuromuscular blockade was achieved with rocuronium. Subjects were then intubated with either a c-DLT or a VS-DLT using direct laryngoscopy with a Mac 3 blade. The use of any adjunct airway devices and the difficulty of intubation was recorded. All intubations were performed by senior anesthesia residents.
In the c-DLT group, tube insertion was halted after the tracheal lumen passed the cords. Then, an FOB was inserted into the bronchial lumen to guide the tube into the left mainstem bronchus. For the VS-DLT group, the patient’s mouth was suctioned prior to laryngoscopy, and the lens of the VS-DLT was defogged using DEFOGGERTM Anti Fog Kit (DeRoyal, Dominican Republic). As the VS-DLT was inserted through the glottis, visualization from the built-in camera was used to guide the tube into the left mainstem bronchus. The DLT placement time was defined as the time from the start of laryngoscopy to the time that the bronchial lumen of the DLT was successfully visualized within the left mainstem bronchus. When single lung ventilation became necessary, the bronchial cuff was inflated, and the appropriate side of the DLT was clamped. If the lens of the VS-DLT became obscured, providers were instructed to take the following steps in order per the manufacturer: (I) inject 20 mL of air into the injection port, (II) connect a 10 mL syringe filled with 2 mL saline and inject twice for a total of 4 mL, (III) connect a 10 mL syringe with 5–10 mL of air and inject twice, (IV) connect an empty 10 mL syringe and aspirate the saline injected twice, and (V) confirm correct tube position with an FOB. An FOB was readily available in the operating room for all subjects.
Data collection
In the preoperative area, research personnel recorded patient demographic data, including age, gender, total body weight (TBW), body mass index (BMI), ASA physical status classification, and baseline vital signs. The following information was recorded for each patient at induction and intubation: time to intubation, difficulty of intubation, Mallampati score, and Cormack-Lehane grade. Anesthesia providers were asked to record the incidence of FOB use for the verification of tube placement, any instances of DLT dislodgement, their ability to predict DLT dislodgement, the presence of secretions during the case, and their ability to clear secretions. Patients randomized to the VS-DLT arm had the quality of visualization during intubation, at incision, throughout the case, and at extubation recorded. Study data were collected and managed using REDCap electronic data capture tools hosted at UT Southwestern (13).
Adverse events
Adverse events monitored included the following: airway injury, prolonged hypoxia (oxygen saturation <92% for >1 minute), bronchospasm, laryngospasm, aspiration, reintubation, a prolonged postanesthesia care unit (PACU) stay, or unplanned hospital admission.
Statistical analysis
Frequencies and percentages were reported for categorical variables. Medians and interquartile ranges were reported for continuous variables. The Kruskal-Wallis test, chi square test, and Fisher’s exact test were used to compare the distributions of variables between the arms, as appropriate. Standardized differences were calculated using Cohen’s d with rank order statistics for continuous variables and Cramer’s V for categorical variables. Bar plots were created to visualize the distributions of variables by group. Statistical significance is indicated by P<0.05. An a priori power analysis was conducted to determine the required sample size required to test the difference between two independent group proportions using the formula for the two-sample z-test with an estimated difference in proportions of 40% and a significance level of 5%. Results showed that a total sample size of 50 patients with two equal sized groups of 25 was required to achieve 90% power. All statistical analysis was conducted in R v3.6.0.
Results
In this study, 25 patients were assigned to c-DLT and 25 subjects were assigned to VS-DLT. The study was concluded after we reached our goal of 50 patients. Analysis was performed with the original assigned group. Patient demographics and the types of surgery for each cohort are summarized in Table 1. There were no statistically significant differences between the two cohorts for the recorded patient characteristics. Our primary outcome, the rate of FOB use in verifying correct placement of the DLT, was significantly reduced in the VS-DLT group (28%) when compared to the c-DLT group (100%) (Table 2, Figure 1) (P<0.001). Additional outcomes are summarized in Table 2. The incidence of dislodgement was significantly lower in the VS-DLT group (16%) compared to the c-DLT group (48%) (P=0.034). The ease of intubation and quality of lung collapse were comparable between the two groups. However, correct tube placement took significantly less time in the VS-DLT group (54 s) than in the c-DLT group (156 s) (P<0.001). After turning laterally, the position of the tube changed less frequently in the VS-DLT group (20%) than in the c-DLT group (56%). Secretions were reported in 48% of VS-DLT subjects and 12% of c-DLT subjects. Interventions to clear secretions were successful in 42% of the VS-DLT subjects who had secretions (Table 3).
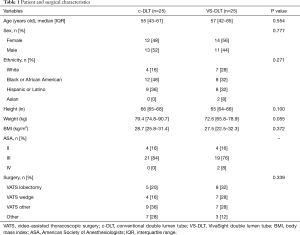
Full table
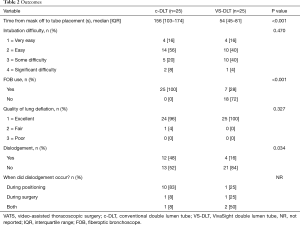
Full table
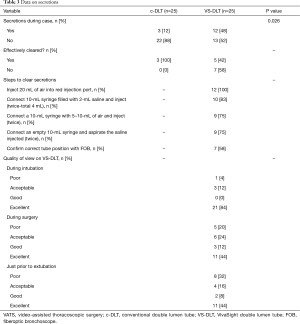
Full table
Discussion
In this prospective randomized controlled trial of 50 patients undergoing thoracic surgery, the rate of FOB use decreased significantly when intubating with a VS-DLT compared to a c-DLT (P<0.001). The rate of FOB usage in this study (28%) is somewhat higher than previously reported in Heir et al. (6.8%) and Larsen et al. (6.6%) (5,14).
The time to correct placement of the c-DLT took three times longer than correct placement of the VS-DLT (Table 2). However, this may not be clinically relevant as the time required to insert either DLT was under 3 minutes for the majority of cases. This difference is likely due to the reduced need for a separate FOB to check positioning of the tube when intubating with the VS-DLT. The camera attached to the VS-DLT allows for continuous visualization inside the airway, which allows confirmation of correct tube placement much more quickly. In contrast, all intubations with a c-DLT required an FOB to verify correct placement, thereby increasing the time required for intubation.
Malpositioning is a common complication of c-DLT use in single lung ventilation (1). In a study by Inoue et al., 83% of patients undergoing single lung ventilation that became hypoxemic were found to have had DLT malpositioning (7). Thus, it is important to quickly identify and rectify tube malpositioning to avoid hypoxemia, poor ventilation, and air leaks as these can lead to increased patient morbidity and mortality. Continuous visualization of the carina provided by the VS-DLT allows the operator to quickly and simply assess tube position. If the tube is found in the correct position, then the provider can evaluate for other possible causes of hypoxemia. If the tube is malpositioned, then the provider can quickly correct the tube’s positioning. Malposition occurred significantly more in the c-DLT group (48%) versus the VS-DLT group (16%) (Table 1). This is likely due to the continuous visualization that the VS-DLT provides, which can enable the provider to forewarn potential dislodgement. This is especially true for when the patient is turned into the lateral position, which is the time that the tube is most likely to move following its initial placement. Both the VS-DLT and the c-DLT were rated comparably by surgeons with respect to lung deflation (Table 2). There were no adverse events reported in any of the subjects.
Intubation using the VS-DLT may also decrease provider stress, particularly in robotic cases where the airway is not easily accessible. When using the VS-DLT, providers can view the DLT position in the airway in real time and correct it without the need for ancillary devices. This added benefit has not been captured by previous studies but may have a positive effect on patient care and provider morale. As our study progressed, we found anecdotal evidence that provider satisfaction was greater with the VS-DLT, but we did not quantify this.
While this study demonstrated potential clinical benefits associated with the use of a VS-DLT, there may be some disadvantages when compared to the use of a c-DLT. According to the most recent analysis, after accounting for repair, maintenance, and cleaning costs, the per procedure cost of a reusable FOB with a c-DLT is $347.61 while the cost of a VS-DLT is $299.96 (5). However, an FOB was required in 28% of the VS-DLT cases, which eliminates any potential cost savings. Additionally, the fixed costs associated with training in FOB use and always having an FOB available will not be reduced by regular use of the VS-DLT. Thus, based on the most current estimates of cost, the VS-DLT may be more expensive per procedure than the c-DLT.
In addition, we found that secretions impaired visualization in just over half of the VS-DLT cohort and that the integrated flushing system and manufacturer’s recommended steps were only able to successfully clear secretions in about half of these cases (Table 3). Unlike an FOB which can be removed and cleaned, the built-in camera on the VS-DLT must be cleaned intratracheally. Thus, despite the benefit of continuous visualization provided by the VS-DLT, it is susceptible to obstruction from secretions which can result in a suboptimal view of the airway (Figure 2). Thus, a separate FOB was required to re-verify positioning of the tube in 58% of the VS-DLT cases that were obstructed by secretions (Table 3). Despite a similar rate of secretions compared to previous studies, this study had a lower rate of being able to effectively clear the secretions (6). The reason for this may be that prior studies included administration of an antisialagogue, which was not done in our study due to concerns for tachycardia in this patient population. As suggested in Rapchuk et al., suctioning the airway and defogging the camera lens prior to intubation may allow for a longer optimal view of the airway after intubation (1). The need for an FOB when the VS-DLT view is obstructed increases the cost associated with the procedure.

There are some limitations to this study. We were unable to blind providers to the randomization of the DLT, which could result in response bias in favor of one tube or the other. In addition, most of the intubations were performed by senior anesthesia residents, which may reduce the generalizability of these findings to the general population of anesthesia providers. Lastly, the survey format of this study is more prone to observer bias and response bias than other more objective experimental designs. Thus, these results may be less valid than other mechanisms of data collection.
Conclusions
The use of an FOB seems to be significantly reduced with use of a VS-DLT compared to a c-DLT. Additionally, the time to correct tube placement is shorter and the incidence of malposition is much lower in the VS-DLT group. Continuous visualization with a VS-DLT therefore appears to be beneficial in clinical practice. However, the reduction in the rate of FOB usage may not be as high as previously reported. As costs of these devices vary between institutions and over time, future cost analyses may find a more compelling economic justification for the use of a VS-DLT.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-1595
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-1595
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-20-1595
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-1595). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the University of Texas Southwestern Medical Center Institutional Review Board (IRB #2018-0098) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rapchuk IL, Kunju S, Smith IJ, et al. A six-month evaluation of the VivaSight video double-lumen endotracheal tube after introduction into thoracic anaesthetic practice at a single institution. Anaesth Intensive Care 2017;45:189-95. [Crossref] [PubMed]
- Campos JH, Hallam EA, Van Natta T, et al. Devices for lung isolation used by anesthesiologists with limited thoracic experience: comparison of double-lumen endotracheal tube, Univent torque control blocker, and Arndt wire-guided endobronchial blocker. Anesthesiology 2006;104:261-6, discussion 5A. [Crossref] [PubMed]
- Narayanaswamy M, McRae K, Slinger P, et al. Choosing a lung isolation device for thoracic surgery: a randomized trial of three bronchial blockers versus double-lumen tubes. Anesth Analg 2009;108:1097-101. [Crossref] [PubMed]
- Cohen E. Double-lumen tube position should be confirmed by fiberoptic bronchoscopy. Curr Opin Anaesthesiol 2004;17:1-6. [Crossref] [PubMed]
- Larsen S, Holm JH, Sauer TN, et al. A Cost-Effectiveness Analysis Comparing the VivaSight Double-Lumen Tube and a Conventional Double-Lumen Tube in Adult Patients Undergoing Thoracic Surgery Involving One-Lung Ventilation. Pharmacoecon Open 2020;4:159-69. [Crossref] [PubMed]
- Heir JS, Guo SL, Purugganan R, et al. A Randomized Controlled Study of the Use of Video Double-Lumen Endobronchial Tubes Versus Double-Lumen Endobronchial Tubes in Thoracic Surgery. J Cardiothorac Vasc Anesth 2018;32:267-74. [Crossref] [PubMed]
- Inoue S, Nishimine N, Kitaguchi K, et al. Double lumen tube location predicts tube malposition and hypoxaemia during one lung ventilation. Br J Anaesth 2004;92:195-201. [Crossref] [PubMed]
- Hou HW, Ouyang BY. Influence of the position of double-lumen endobronchial tube on the efficacy of lung separation and ventilation. Nan Fang Yi Ke Da Xue Xue Bao 2006;26:576-8. [PubMed]
- Levy-Faber D, Malyanker Y, Nir RR, et al. Comparison of VivaSight double-lumen tube with a conventional double-lumen tube in adult patients undergoing video-assisted thoracoscopic surgery. Anaesthesia 2015;70:1259-63. [Crossref] [PubMed]
- Schuepbach R, Grande B, Camen G, et al. Intubation with VivaSight or conventional left-sided double-lumen tubes: a randomized trial. Can J Anaesth 2015;62:762-9. [Crossref] [PubMed]
- Massot J, Dumand-Nizard V, Fischler M, et al. Evaluation of the Double-Lumen Tube Vivasight-DL (DLT-ETView): A Prospective Single-Center Study. J Cardiothorac Vasc Anesth 2015;29:1544-9. [Crossref] [PubMed]
- de Bellis M, Accardo R, Di Maio M, et al. Is flexible bronchoscopy necessary to confirm the position of double-lumen tubes before thoracic surgery? Eur J Cardiothorac Surg 2011;40:912-6. [Crossref] [PubMed]
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-81. [Crossref] [PubMed]
- Heir JS, Purugganan R, Jackson TA, et al. A retrospective evaluation of the use of video-capable double-lumen endotracheal tubes in thoracic surgery. J Cardiothorac Vasc Anesth 2014;28:870-2. [Crossref] [PubMed]


