
Risk factors of postoperative recurrence of primary spontaneous pneumothorax
Introduction
Primary spontaneous pneumothorax (PSP) is a common entity that develops in relatively young, healthy patients. Surgical management is indicated in patients with recurrent ipsilateral pneumothorax, simultaneous bilateral pneumothoraxes, and persistent air leakage (1,2). Young patients with PSP represent an opportunity for surgical residents to train in thoracoscopic surgery. This is not the case with secondary spontaneous pneumothorax (SSP), because surgery is sometimes complicated. Thoracoscopic surgery has been performed with increasing frequency in recent decades; however, the recurrence rate of pneumothorax after thoracoscopic surgery ranges from 2% to 14%—a higher rate than after thoracotomy (3,4). To prevent postoperative recurrence, surgeons may perform additional procedures such as pleural reinforcement using oxidized regenerated cellulose (ORC) mesh or absorbable polyglycolic acid (PGA) sheets (3,5-8). Young patients with PSP are reportedly at significant risk for postoperative recurrence (3,9), possibly because of bulla neogenesis (3,8-11). The risk factors for postoperative recurrence of spontaneous pneumothorax are not fully understood. These factors, together with the phenomenon of bulla neogenesis, may contribute to the high rate of recurrence seen in young patients. We aimed to investigate the relation between postoperative recurrence and its risk factors. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-2436).
Methods
Study design
We designed a retrospective study to review the records of patients who underwent surgery for spontaneous pneumothorax at Chiba University Hospital. This study was approved by the institutional review board of Chiba University Graduate School of Medicine, No.2996. The requirement for written consent was waived because of the retrospective nature of this study. Patients were notified of the study and given the option to optout. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). We included patients who underwent conservative treatment for recurrent pneumothorax, such as indwelling chest-tube drainage, and patients who had persistent air leakage. We excluded patients with secondary ipsilateral recurrent pneumothorax after previous surgery.
Surgery for spontaneous pneumothorax
A double-lumen endotracheal tube was inserted into the airway under general anesthesia, and surgery was performed during selective ventilation of the contralateral lung. Surgery was carried out with patients in the lateral position. The first choice for intervention at our institution was thoracoscopic surgery using a 5-mm, 30° video thoracoscope and 3 intercostal ports (5–12 mm) for access. The working ports were typically placed in the third intercostal space in the anterior and posterior axillary line, and the fifth intercostal space in the midaxillary line, but could be placed elsewhere depending on the requirements of the case. Thoracotomy (approximately 4–8 cm) was an option when pleural adhesions prevented the safe use of thoracoscopy or port placement was not suitable for procedures such as pulmorrhaphy. Surgeons were classified as residents, fellows, and specialists. Since our hospital is an educational facility, residents or fellows are selected for procedures that are not expected to be difficult; their procedures are conducted under the guidance of specialists. Bullectomy or bulla ligation were performed to halt air leakage from the pulmonary parenchyma; in some patients, pleural cautery or pulmorrhaphy was also performed. The choice of surgical procedure was made by the surgeons after examining the preoperative CT findings and the immediate intraoperative findings. When bullae were numerous or their stalks were large, we opted for bullectomy. When bullae were small and few in number or their stalks were small, we performed bulla ligation. We performed pleural cautery when the origin of air leakage was not clear but the location was thought to be at the site of the inflammatory changes. We performed pulmorrhaphy when bullectomy or bulla ligation were deemed difficult—for example, when the site of air leakage was near the hilum or when emphysematous changes were extremely prevalent. Pleural reinforcement was considered an optional procedure to prevent recurrence; this was left to the surgeons’ discretion. All patients were followed for at least 1 month postoperatively on an outpatient basis. All patients were instructed to consult the follow-up clinic when any symptoms occurred that were suspicious for recurrent pneumothorax.
Review of data for patients with spontaneous pneumothorax
We reviewed the medical records of each patient to obtain clinical and perioperative information, including patient age, sex, type of spontaneous pneumothorax (primary or secondary), smoking habits, laterality of the pneumothorax, history of ipsilateral and contralateral spontaneous pneumothorax before surgery, surgical approach (thoracoscopic surgery or thoracotomy), surgical methods (bullectomy using an endoscopic stapler or bulla ligation using a pre-tied loop ligature), pleural reinforcement (ORC mesh, absorbable PGA sheets, or fibrin glue), operative time (<100 or >100 min), and the type of surgeon. We classified surgeons with less than 3 years of experience as residents, and those with more than 3 years of experience who were training as specialists in general thoracic surgeons as fellows. Specialists were general thoracic surgeons certified by The Japanese Board of General Thoracic Surgery. Postoperative recurrence was defined as ipsilateral pneumothorax after surgery.
Statistical analyses
We used recurrence-free probability (RFP), multivariate analysis, and the inverse probability of treatment-weighted (IPTW) method (that employs the propensity score) to assess the relation between postoperative recurrence of pneumothorax and the risk factors in question. We calculated RFP using the Kaplan-Meier method. The Cox regression analysis was used for multivariate analysis. Finally, we performed our propensity score analysis by Cox regression analysis using the IPTW method. A P value of <0.05 indicated statistical significance. The hazard ratio (HR) and 95% confidence intervals (95% CI) were calculated for each variable. We used the EZR software package (http://www.jichi.ac.jp/saitama-sct/SaitamaHP.files/statmed.html) to perform all statistical analyses (12).
Results
Patient profile
Between January 2006 and October 2017, a total of 233 patients with spontaneous pneumothorax underwent surgery for this indication at Chiba University Hospital. Patient characteristics are summarized in Table 1. There were 186 men and 47 women, with an average age of 39.0 years. A total of 53 patients were younger than 20 years of age (22.7%), and 65 were between 20 and 29 years of age (27.9%). Of patients with PSP, 84.5% were younger than 30 years of age (Table S1). A total of 129 patients (55.4%) had PSP, and 113 patients (48.5%) were never-smokers. The type of spontaneous pneumothorax was categorized by comprehensively evaluating the preoperative CT findings, any history of pulmonary disease, and the patient’s smoking history. The underlying diseases in patients with SSP included chronic obstructive pulmonary disease, interstitial pneumonia, and Birt-Hogg-Dubé syndrome (Table S2). Thoracoscopic surgery was the most common approach, performed in 181 patients (77.7%) overall and in 90.6% of patients with PSP (Table S1). A total of 150 patients (64.4%) underwent bullectomy, and 61 patients (26.2%) underwent bulla ligation. Pleural reinforcement to prevent recurrence was performed in almost all patients (91.4%): ORC mesh was the most commonly used material [125 patients (53.6%)], but absorbable PGA sheets [80 patients (34.3%)] and fibrin glue [66 patients (28.3%)] were also used. The median operative time was 96 minutes. A total of 65 patients (27.9%) underwent surgery by a resident [41.4% of patients with PSP had a resident as their primary surgeon (Table S1)], 92 (39.5%) underwent surgery by a fellow, and 76 (32.6%) underwent surgery by a specialist. Additional treatment for prolonged air leakage, such as chemical pleurodesis, was performed in 30 patients.
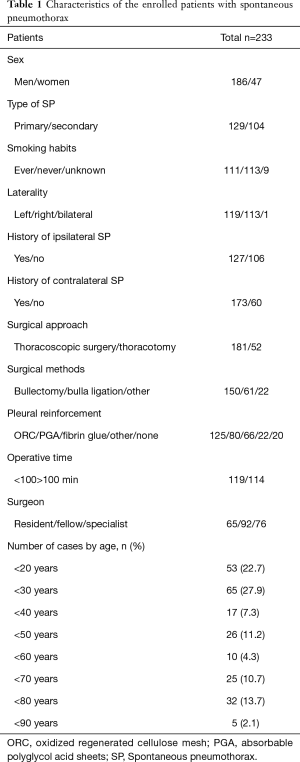
Full table
A total of 41 patients (17.6%) experienced recurrence (Table 2). Of these, 17 (32.1%) were younger than 20 years of age and 17 (26.2%) were between 20 and 29 years of age. Of the 84 patients younger than 30 years of age, 34 (28.8%) experienced a recurrence, accounting for 82.9% of the 41 patients with recurrence.

Full table
The 5-year RFP was 65.6% for all patients (Table 3). In patients younger than 20 years of age, the RFP was 44.2%, and in those between 20 and 29 years of age it was 48.5%.
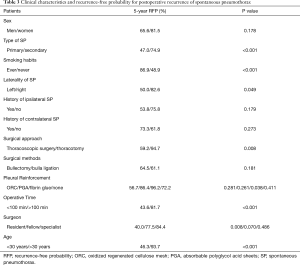
Full table
The recurrence rate for bullectomy was 20.7% (31/150 patients), and the recurrence rate was 16.4% (10/61 patients) for bulla ligation (P=0.5669, Table S3). The 5-year RFP for patients undergoing bullectomy was 64.5%, and in patients undergoing bulla ligation it was 61.1% (P=0.181; Table 3). The recurrence rate for patients who underwent pleural reinforcement with ORC mesh was 20.8%, and the rate for those who received absorbable PGA sheets was 8.6% (P=0.02; Table S3). The 5-year RFP for patients who underwent pleural reinforcement using ORC mesh was 56.7% (P=0.281), and for those who underwent reinforcement with absorbable PGA sheets it was 86.4% (P=0.261; Table 4). The recurrence rate for ligation with reinforcement using a PGA sheet was 4.0% (1/25 patients; P=0.09) and the 5-year RFP was 90.0% (P=0.459)
Full table
Recurrence-free probability and multivariate analysis of risk factors for recurrence
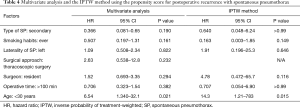
Table 4 shows that PSP (P<0.001), never-smoker status (P<0.001), left-sided pneumothorax (P=0.049), thoracoscopic surgery (P=0.008), operative time less than 100 min (P<0.001), surgery by a resident surgeon (P=0.008), and younger than 30 years old (P<0.001) were significant risk factors for postoperative recurrence. Factors for multivariate analysis were selected based on the results of RFP analysis. Multivariate analysis (Table 4) indicated that age younger than 30 years (HR 6.54; 95% CI, 1.34–32.1; P=0.021) was an independent predictor of recurrence.
Assessment of risk factors for recurrence using the IPTW method
According to our univariate analysis, the confounding factors for PSP were the patient’s smoking habit, the laterality of the pneumothorax, the surgical method, the surgical approach, the classification of surgeon, the performance of pleural reinforcement, and patient age younger than 30 years (Table S1). When IPTW analysis was performed to discriminate significant confounders, only patient age less than 30 years was revealed to be a significant factor (HR 14.3; 95 CI, 1.21–783; P=0.0153; Table 4).
Discussion
For the patients with recurrent spontaneous pneumothorax, thoracoscopic bullectomy is considered a definitive treatment choice (3,4). Despite its high recurrence rate when performed alone (16.3–24.1%) (9,13-15). Various additional intraoperative procedures were designed to be performed for preventing postoperative recurrence—pleural reinforcement is among the more effective procedures. Cho et al. (16) reported a 4.8% recurrence rate using absorbable ORC mesh coverage and fibrin glue in patients with PSP, while Lee et al. (17) reported a 3.9% recurrence rate using absorbable PGA sheets to widely cover the staple line and pleural abrasion in patients with PSP.
Postoperative recurrence of spontaneous pneumothorax especially in young patients is relatively common due to bulla neogenesis (9). Nakayama et al. reported that after performing thoracoscopic bullectomy for PSP with application of an absorbable PGA sheet, patients younger than 23 years of age have a lower probability of 5-year recurrence-free status than those aged 23 years or older (78.1% vs. 93.8%) (3). The recurrence rate in our study was higher (28.8%) and 5- year RFP was lower (46.3%) in patients younger than 30 years of age, even with pleural reinforcement.
The treatment of young patients with PSP presents opportunities for residents to train in thoracoscopic surgery. Since our hospital is an educational facility, residents or fellows perform surgery, under the guidance of specialists, if the procedure is not expected to be difficult. In contrast to SSP, surgery for PSP in our study often involved resident surgeons. We therefore speculate that the higher rate of recurrence in surgery for PSP may be due to surgeon inexperience. To eliminate this as a possible confounding factor, we used propensity scoring to determine that patient younger than 30 years of age is the only significant factor for postoperative recurrence, regardless of the type of surgeon or surgical approach.
Our study demonstrates a trend toward a higher recurrence rate for bullectomy (5-year RFP: 64.5%) than for bulla ligation (5-year RFP: 61.1%; P=0.181). Our results are consistent with those of Fujino et al., who report that the recurrence rate for bulla ligation in patients with spontaneous pneumothorax is significantly lower than that of bullectomy (5.8% vs. 17.8%) (18). We speculate that, of the various surgical methods, bulla ligation is less stressful on the surgical site than bullectomy, and as a result, bulla neogenesis is less likely. Our study also showed that the postoperative recurrence rate is higher in patients who undergo reinforcement using ORC mesh than with PGA sheets, with rates similar to those found by Ozawa et al. (22.8% vs. 3.6%) (8). Pleural reinforcement using ORC sheets prevents recurrence by thickening the visceral pleura near the surgical site. It also prevents adhesion formation between the surgical site and the chest wall. However, the mesh sheet may fall into the chest cavity. We speculate that this may cause recurrence more frequently than with the use of PGA sheets. Although we can only report a limited number of cases, we found that ligation with reinforcement using a PGA sheet may be an effective surgical method for preventing recurrence, with only a 4% recurrence rate and a 5-year RFP of 90.0%. It is very difficult to determine exactly why bulla ligation with the use of PGA sheets causes less recurrence, but it may be better for surgeons to combine methods that are less likely to lead to recurrence. Surgeons should think carefully about the surgical and pleural reinforcement methods used for each patient. One method of reducing postoperative recurrence is the use of 50% glucose solution for pleural reinforcement, as described by Fujino et al. (19). Abrasion of the surrounding pleural lesion after bullectomy or bulla ligation may also reduce recurrence.
The major limitations of this study were that it was conducted at a single institution, and the results were based on a small number of patients. Multicenter prospective trials are needed to confirm the results of this study.
Conclusions
In conclusion, patients younger than 30 years old with spontaneous pneumothorax, especially PSP, had a significantly higher recurrence rate after surgical repair. It is necessary to prevent postoperative recurrence by devising the operative method and pleural reinforcement method.
Acknowledgments
This data was presented at 35th Annual Meeting of the Japanese Association for Chest Surgery, Chiba, Japan, May 2018.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting Checklist. Available at http://dx.doi.org/10.21037/jtd-20-2436
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-2436
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-20-2436
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-2436). YS serves as an unpaid editorial board member of Journal of Thoracic Disease from Apr 2019 to Mar 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the institutional review board of Chiba University Graduate School of Medicine, No.2996. The requirement for written consent was waived because of the retrospective nature of this study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Onuki T, Kawamura T, Kawabata S, et al. Neo-generation of neogenetic bullae after surgery for spontaneous pneumothorax in young adults: a prospective study. J Cardiothorac Surg 2019;14:20. [Crossref] [PubMed]
- MacDuff A, Arnold A, Harvey J, et al. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii18-ii31. [Crossref] [PubMed]
- Nakayama T, Takahashi Y, Uehara H, et al. Outcome and risk factors of recurrence after thoracoscopic bullectomy in young adults with primary spontaneous pneumothorax. Surg Today 2017;47:859-64. [Crossref] [PubMed]
- Sahn SA, Heffner JE. Spontaneous pneumothorax. N Engl J Med 2000;342:868-74. [Crossref] [PubMed]
- Muramatsu T, Nishii T, Takeshita S, et al. Preventing recurrence of spontaneous pneumothorax after thoracoscopic surgery: a review of recent results. Surg Today 2010;40:696-9. [Crossref] [PubMed]
- Sakamoto K, Takei H, Nishii T, et al. Staple line coverage with absorbable mesh after thoracoscopic bullectomy for spontaneous pneumothorax. Surg Endosc 2004;18:478-81. [Crossref] [PubMed]
- Lee S, Kim HR, Cho S, et al. Korean Pneumothorax Study Group. Staple line coverage after bullectomy for primary spontaneous pneumothorax: a randomized trial. Ann Thorac Surg 2014;98:2005-11. [Crossref] [PubMed]
- Ozawa Y, Sakai M, Ichimura H. Covering the staple line with polyglycolic acid sheet versus oxidized regenerated cellulose mesh after thoracoscopic bullectomy for primary spontaneous pneumothorax. Gen Thorac Cardiovasc Surg 2018;66:419-24. [Crossref] [PubMed]
- Tsuboshima K, Matoba Y, Wakahara T, et al. Natural history of bulla neogenesis for primary spontaneous pneumothorax: a propensity score analysis. Gen Thorac Cardiovasc Surg 2019;67:464-9. [Crossref] [PubMed]
- Huang H, Ji H, Tian H. Risk factors for recurrence of primary spontaneous pneumothorax after thoracoscopic surgery. Biosci Trends 2015;9:193-7. [Crossref] [PubMed]
- Noh D, Lee S, Haam SJ, et al. Recurrence of primary spontaneous pneumothorax in young adults and children. Interact Cardiovasc Thorac Surg 2015;21:195-9. [Crossref] [PubMed]
- Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplantation 2013;48:452-8. [Crossref] [PubMed]
- Hirai K, Kawashima T, Takeuchi S, et al. Covering the staple line with a polyglycolic acid sheet after bullectomy for primary spontaneous pneumothorax prevents postoperative recurrent pneumothorax. J Thorac Dis 2015;7:1978-85. [PubMed]
- Cardillo G, Bintcliffe OJ, Carleo F, et al. Primary spontaneous pneumothorax: a cohort study of VATS with talc poudrage. Thorax 2016;71:847-53. [Crossref] [PubMed]
- Hong KP, Kim DK, Kang KH. Staple line coverage with a polyglycolic acid patch and fibrin glue without pleural abrasion after thoracoscopic bullectomy for primary spontaneous pneumothorax. Korean J Thorac Cardiovasc Surg 2016;49:85-91. [Crossref] [PubMed]
- Cho S, Huh DM, Kim BH, et al. Staple line covering procedure after thoracoscopic bullectomy for the management of primary spontaneous pneumothorax. Thorac Cardiovasc Surg 2008;56:217-20. [Crossref] [PubMed]
- Lee S, Park SY, Bae MK, et al. Efficacy of polyglycolic acid sheet after thoracoscopic bullectomy for spontaneous pneumothorax. Ann Thorac Surg 2013;95:1919-23. [Crossref] [PubMed]
- Fujino M, Yamakawa H, Matsui Y, et al. Evaluation of video-assisted thoracoscopic surgery for double loop ligation of the bullae for spontaneous pneumothorax. JPN J Chest Surg 2010;24:999-1003. [Crossref]
- Fujino K, Motooka Y, Koga T, et al. Novel approach to pleurodesis with 50% glucose for air leakage after lung resection or pneumothorax. Surg Today 2016;46:599-602. [Crossref] [PubMed]


