A late visceral hernia after diaphragmatic flap coverage of the bronchial stump
Background
The bronchial stump support has been recommended to reduce the risk of a bronchopleural fistula in patients undergoing pneumonectomy, especially in those with neoadjuvant treatment (1). For this purpose, the bronchial stump is usually covered by tissue flaps, such as pericardium, pleura, omentum, and muscle flaps including intercostal, latissimus dorsi, serratus anterior, and diaphragm muscles (2,3). Therefore, the use of the diaphragmatic muscle flaps has not been popular in thoracic surgery, and several visceral herniations in the early follow-up period have been reported (4). Here in this report, we presented a patient with visceral herniation, detected 5 years after a pneumonectomy for non-small cell lung cancer operation with a diaphragmatic muscle flap support on the bronchial stump. He underwent an emergency thoraco-laparatomy 9 years after the first surgery due to acute abdomen symptoms. To our knowledge, this is the first reported case with visceral herniation in the late period undergoing repair.
Case report
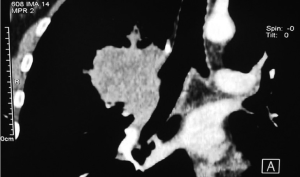
A 54-year-old man presented to the thoracic surgery clinic complaining with sudden and severe abdominal pain, accompanied by right chest pain, vomiting, and nausea. He had underwent a right pneumonectomy due to non-small cell lung cancer (squamous cell carcinoma) after a neoadjuvant chemotherapy, 9 years ago in our clinic (Figure 1). A diaphragmatic muscle pedicle flap had been used to reinforce the bronchial stump following pneumonectomy. A chest roentgenogram showed a total opacity in the right hemithorax. The computed tomography of the chest demonstrated abdominal visceral organ herniation into the right side of the thorax (Figure 2). Although a small visceral organ herniation had already been detected 5 years after pneumonectomy during a follow-up consultation which was not present in the previous visits, and the patient had been offered to undergo repair, he had refused any surgical intervention since he had been asymptomatic. Then, he was lost to follow-up. The patient had no history of an abdominal or chest trauma, or any disease after the pneumonectomy operation.
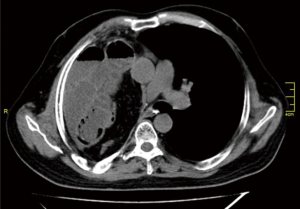
The patient was operated on through a right thoracoabdominal incision at the supine position. The right hemithorax was filled with transverse colon, small bowel, and omentum through a diaphragmatic defect. Some parts of the small bowel were aperistaltic, and showing signs of ischemia, but after warm compressing these parts of the bowel became normal, and thus there was no need for an intestinal resection. Following the reduction of the visceral organs into the abdomen, the diaphragmatic defect was repaired using a mesh.
The patient had an uneventful recovery. The chest drain was removed 3 days after the surgery. The patient was started on a clear liquid diet on the first postoperative day. Diet was advanced to puree on postoperative day 3, to soft meals on day 4, and regular diet was administered on day 5. The patient was discharged on the postoperative day 10, and was alive and without problem 18 months after the operation. A chest computed tomography taken on the first year follow-up demonstrated no recurrence.
Discussion
Diaphragmatic muscle flaps have been used for reconstructive procedures in the esophagus and tracheobronchial tree for more than 40 years (5,6). Since the diaphragmatic muscle is strong, elastic, well vascularized, and resistant to necrosis, with good regeneration capacity, Westaby et al. (7) proposed its use as an ideal material for reconstruction within the chest. Mineo and Ambrogi (3) presented their technique in four patients, and concluded that diaphragmatic muscle flap was helpful in closing postoperative bronchopleural fistulas. The abovementioned data favored the use of diaphragmatic muscle flaps (3,5-7). Despite these favorable data, the “best evidence topic” study of Llewellyn-Bennett et al. (1) demonstrated that the use of diaphragmatic muscle flaps for reconstructive procedures in thoracic surgery did not become popular, and the surgeons mostly preferred tissue flaps or muscle flaps other than the diaphragm. The reason for that is not given in details, but may be simply due to surgeon’s preference or due to the trend toward a lower morbidity compared to intercostal muscle flaps, as reported by Lardinois et al. (4).
Mineo and Ambrogi (8) reported some complications including arrhythmia, respiratory insufficiency, and empyema after diaphragmatic muscle flap use in 25 patients. They did not report any visceral herniation for 11 patients who survived more than 1 year. Lardinois et al. (4) compared the intercostal muscle flaps with diaphragmatic muscle flaps for the bronchial stump reinforcement in cases undergoing pneumonectomy. In their study, they preferred diaphragmatic muscle flaps in 13 patients, and reported three (23%) visceral herniations in the early phase of their experience. Besides these two abovementioned studies, there exist no reports concerning the outcome (early and/or late) of diaphragmatic muscle flaps in the bronchial stump coverage.
Our patient developed visceral herniation 5 years after the pneumonectomy operation. He was advised to undergo surgery for repair when the small herniation was detected, but he denied the proposal since he had been asymptomatic. Later on, he admitted with signs and symptoms of acute abdomen 9 years after surgery, and underwent an urgent diaphragmatic repair with an uneventful recovery. To our knowledge, this is the first reported case about the late development of a visceral herniation after diaphragmatic muscle flap usage.
Conclusions
The use of the diaphragmatic muscle flaps has not been popular in thoracic surgery. The rate of early visceral herniations following diaphragmatic muscle flaps is not low. Although not reported before, one should keep in mind that even years after the procedure, it is possible to face with a late visceral herniation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Llewellyn-Bennett R, Wotton R, West D. Prophylactic flap coverage and the incidence of bronchopleural fistulae after pneumonectomy. Interact Cardiovasc Thorac Surg 2013;16:681-5. [PubMed]
- Pairolero PC, Arnold PG, Piehler JM. Intrathoracic transposition of extrathoracic skeletal muscle. J Thorac Cardiovasc Surg 1983;86:809-17. [PubMed]
- Mineo TC, Ambrogi V. Early closure of the postpneumonectomy bronchopleural fistula by pedicled diaphragmatic flaps. Ann Thorac Surg 1995;60:714-5. [PubMed]
- Lardinois D, Horsch A, Krueger T, et al. Mediastinal reinforcement after induction therapy and pneumonectomy: comparison of intercostal muscle versus diaphragm flaps. Eur J Cardiothorac Surg 2002;21:74-8. [PubMed]
- Suvorova TA. Plastic surgery of the bronchial stump with a diaphragmatic flap. Khirurgiia (Mosk) 1958;34:69-80. [PubMed]
- Petrovsky BV. The use of diaphragm grafts for plastic operations in thoracic surgery. J Thorac Cardiovasc Surg 1961;41:348-55. [PubMed]
- Westaby S, Shepherd MP, Nohl-Oser HC. The use of diaphragmatic pedicle grafts for reconstructive procedures in the esophagus and tracheobronchial tree. Ann Thorac Surg 1982;33:486-90. [PubMed]
- Mineo TC, Ambrogi V. The diaphragmatic flap: A multiuse material in thoracic surgery. J Thorac Cardiovasc Surg 1999;118:1084-9. [PubMed]


