A new free-cost e-service supporting clinicians to manage their difficult-to-treat TB cases: the ERS-WHO TB consilium
Multidrug-resistant tuberculosis (MDR-TB), defined as TB caused by Mycobacterium tuberculosis strains resistant to isoniazid and rifampicin (the core anti-TB drugs currently in use), and extensively drug resistant tuberculosis (XDR-TB), defined as MDR-TB caused by strains resistant to at least one fluoroquinolone and one injectable second-line anti-TB drug in addition to isoniazid and rifampicin, has attracted interest at different levels (1-5).
M/XDR-TB represents a serious threat for TB control and elimination. Therefore, the World Health Organization (WHO) ensures, via its Global TB Report, monitoring and evaluation of prevalence and incidence rates as well as temporal trends of drug resistant TB at both global and regional level (2,3).
According to the latest global WHO estimates, in 2013 there were an estimated 480,000 new cases of MDR-TB with 210,000 estimated deaths. This means that 3.5% of new cases and 20.5% of previously treated cases are estimated to be affected by MDR-TB at global level (2).
The prevalence of MDR-TB is particularly high in several countries belonging to the former Soviet Union (FSU), where 9-35% of new cases and ≥50% of previously treated cases harbor MDR-TB strains (2).
Although XDR-TB has presently been reported by 100 countries worldwide, representative data from continuous surveillance or special surveys regarding the proportion of MDR-TB cases affected by XDR-TB is available from 75 countries and 5 territories only. The analysis of these data indicates that the average proportion of MDR-TB cases harboring XDR-TB strains of M. tuberculosis was 9% (95% CI, 6.5-11.5%) and that 15 out of 75 countries reported 10 or more XDR-TB cases in the most recent year for which data were available.
Again, the highest proportion of MDR-TB cases affected by XDR-TB has been observed in countries belonging to the FSU, specifically in Georgia (20%), Kazakhstan (22.7%), Latvia (21.7%), Lithuania (24.8%) and Tajikistan (Dushanbe city and Rudaki district: 21%) (2).
Recent evidence suggests that the clinical outcome of MDR-TB cases is largely unsatisfactory (2,6-10).
In the largest ever-published cohort of 9,153 MDR-TB cases from 32 observational cohorts supporting an individual data meta-analysis, the clinical outcomes were unacceptably poor (treatment success at 54%; default 23%; failure/relapse 8%; death 15%) (8). In XDR-TB cases and cases with resistance patterns beyond XDR the outcomes were even worse, with treatment success ranging from 19% to 40%, failure/relapse from 15% to 54% and death from 15% to 35% (9,10).
The challenge of providing proper treatment to M/XDR-TB patients has been identified by the international community as one of the main reason explaining poor treatment outcomes, given the high cost and the limited availability of second-line anti-TB drugs, the frequent occurrence of adverse events, the risk of acquiring further mycobacterial resistance and the presence of associated conditions (i.e., alcohol and drug abuse; poor patients’ adherence) or comorbidities (i.e., HIV infection).
WHO recommends that management of MDR-TB cases be supported by a specialized team, composed by different medical specialists, with different competencies and perspectives (including TB clinicians/pneumologists with clinical expertise both for adults and children; physicians with surgical, radiological and public health expertise; health staff with psychological background and nursing experience). The implementation of such a committee (known as “Consilium” in most of the FSU countries) is recommended to ensure a rational use of second line drugs and avoid mismanagement of MDR-TB patients. At present, several high MDR-TB burden countries in the different WHO Regions have introduced Consilium-like committees at national or sub-national level to reach consensus on the best treatment approach for their patients.
In addition to national Consilia, the Green Light Committee (GLC), a WHO-hosted committee (recently re-organized at the Regional level) provides continuous technical assistance on MDR-TB management to countries in different ways, including country visits and on-distance email or telephone coaching while ensuring MDR-TB patients are managed as per international guidelines.
However, before launching the ERS/WHO electronic Consilium in September 2012, there were no online mechanisms facilitating peer-to-peer consultation for individual patients at global level.
Available evidence suggests that the existing Consilia either have limited experience or cover only a restricted fraction of the patients in the country or territory (11). On the other hand, the majority of low TB incidence countries do not have a similar consultation committee at national level, even though expertise to manage M/XDR-TB cases in these settings is usually limited to a small group of experts and concentrated in main MDR-TB reference centres.
A recent European Respiratory Society (ERS)/European Centre for Disease Control and Prevention (ECDC) study highlighted several clinical and public health MDR-TB management shortcomings even in some of the high income and low TB incidence countries of the European Union (EU) (12). The existence of WHO guidelines and European Standards of TB Care seems apparently insufficient to guarantee appropriate treatment of M/XDR-TB, while a rapid advice from a multidisciplinary team with clinical and public health experience at national or supranational level would help ensuring proper treatment (13-15). In countries without a formal system of consultation, specialised staff from MDR-TB reference centres usually spends a significant proportion of their working time responding to phone or e-mail clinical queries from all over the country and without any formal recognition, monitoring or support for the service offered. In addition, the recent introduction of two new second line drugs for MDR-TB (bedaquiline and delamanid) raised completely new challenges in terms of correct identification of eligible patients, choice of the optimized background regimen, management of side effects and pharmacovigilance (16,17).
The ERS has increased its commitment, technical support and funding towards TB control and elimination in Europe over time (18-23); this was done through different initiatives, including its presidential TB plan, the European forum for TB innovation and, more recently, the Rome global consultation on TB elimination which produced the global consensus document “Framework for tuberculosis elimination in low-incidence countries” (24).
To this extent and after consultation with WHO (European Office) and ECDC, and under the umbrella of the ERS Presidential initiative, the ERS-WHO electronic TB Consilium initiative has been launched during the 30th ERS Congress in Vienna, on September 6th, 2012. The WHO regional office for Europe signed a memorandum of understanding with ERS to co-ordinate and co-manages this initiative.
Aim of this article is to describe the objectives and the results of this initiative, and to advocate for its use in Asia.
The overarching goal of this initiative is to provide scientifically sound and evidence-based advices to national Consilia and individual clinicians on how to manage drug-resistant TB and other difficult-to-treat TB cases, including co-infection with HIV and paediatric cases, at global level. Through technical guidance provided to clinicians, the main contribution and outcome of the initiative will be a public health response aimed at achieving the correct management of affected patients and prevention of further drug resistance development. Its secondary objective is to ensure monitoring and evaluation of clinical practices on the ground (diagnosis, treatment and prevention). On top of supporting clinicians, the system will also allow evaluating the trends in key challenges and pitfalls which can be addressed through human resources capacity building, including M/XDR-TB management practices (e.g., correct diagnostic and treatment prescription habits), and clinician’s compliance to WHO and other international, evidence-based guidelines.
The ERS/WHO TB Consilium, accessible at www.tbconsilium.org by any physician needing clinical support, ensures a free-cost, multi-lingual (English, Portuguese, Russian and Spanish at present) internet-based consultation system able to provide suggestions on clinical management of complicated TB cases by two independent experts in less than 3 working days. The launch of the initiative has been preceded by a call for experts (including TB clinicians, paediatricians, microbiologists, but also other professionals relevant for patient management). The expert applications have then been reviewed and validated by an expert panel based on strict technical criteria. The electronic TB Consilium platform has been then presented to different countries, national TB programme managers and individual clinicians, and launched at WHO TB Strategic Technical Advisory Group (STAG) in Geneva in 2012. In addition, ERS reached chest specialists through its own publications (newsletter, European Respiratory Journal) and its website. The TB Consilium has been also included in the curriculum of the WHO Course for TB managers and consultants aimed at training on how to apply the new WHO End TB Strategy, focused on the concept of TB Elimination. The course is conducted twice a year in Cepina/Sondalo, Italy (www.publichealthcg.com) and replicated in different continents in different languages.
Recently, a first evaluation of the e-platform’s utilization has been published after the TB Consilium completed its support to the first ten clinical cases (25).
The study evaluated the core variables which are necessary to describe a TB case, including the following: origin of the expert consultation’s request (country generating the request), patient’s country of birth, clinical questions and clinical features of the case, performance of the platform (time to load the case, response time, need for additional request for details, problems encountered, etc.), as well as client’s satisfaction (evaluated through a structured questionnaire).
The study concluded that:
- Requests to the TB Consilium originated from different regions of the world, confirming that there is a global need of clinical advice on MDR-TB and difficult-to treat-cases. Requests came mainly from Europe-with the United Kingdom being predominant (5 requests out of 10) but also from India, Latin America and Vietnam;
- Although the majority of requests were for adult patients (mean age, 27.9 years; range, 12-40 years), 2 out of 10 cases were of paediatric interest (a 14-year-old girl from Vietnam and a 12-year-old girl from India, respectively);
- Only one among the first ten cases evaluated was drug susceptible while the remaining nine cases were MDR-TB (2 being XDR-TB and 1 pre-XDR, e.g., MDR-TB with additional resistance to a fluoroquinolone or aminoglycoside);
- Six out of ten cases were pulmonary TB cases, while three were extrapulmonary and one had both pulmonary and extrapulmonary disease. All of them were bacteriologically confirmed;
- In most of the cases the clinician requested experts’ opinion about the most suitable treatment regimen, validation of the treatment regimen prescribed and suggested treatment duration. In a very complicated case from the United Kingdom the clinician requested experts’ opinion for the management of side effects as cachexia and muscle wasting and the appropriateness of surgical treatment. In other cases, specific guidance on possible drug interactions was requested. In one of the extrapulmonary cases the question specifically asked how to monitor the response to treatment and the recommended treatment duration;
- The time needed for the clinician to upload a single case and questions into the electronic platform was estimated to be less than 30 min, with a mean value of 20 min; the average response time was 40 h. In two cases the experts asked the client clinician to provide further clinical details in order to finalise their report properly;
- All clinicians reported to be largely satisfied by the TB Consilium services;
- Experts involved provided very useful comments to improve the platform’s functionality. The main suggestion was aimed at improving reporting of the new diagnostics tests and radiological findings, and a better location for the (open) spaces where the clinician is allowed to add descriptive clinical details;
- The coordinators identified the need to allow a consolidation of the two experts’ reports, in order to provide the clinician with a perspective for the best interpretation and use of the experts’ reports. In addition the client’s satisfaction survey was added, together with the option to invite a third expert or to disengage an expert not able to provide a rapid reply if necessary. The reviewers’ pop-up directory was improved, making details available to facilitate the choice (e.g., language spoken, specialty: paediatrician, surgeon, HIV/infectious disease expert, etc.).
Further update about utilization of the Consilium platform is summarized in Table 1.
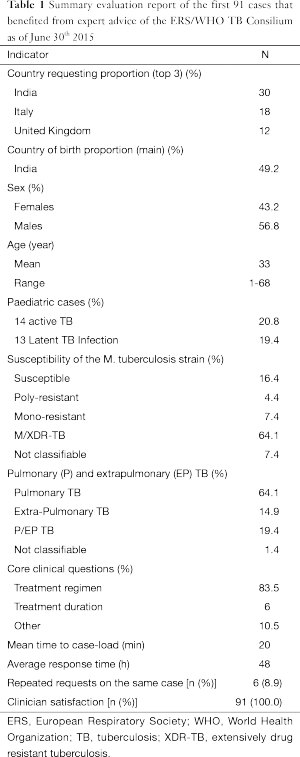
Full table
As of June 30th, 2015, 91 cases benefited from the ERS/WHO Consilium. There were 67 cases of active TB requesting individual advice. In addition, advice was requested for additional 24 cases, including 4 active TB and 20 individuals latently infected in two epidemics (26,27). For 6 individual cases more than one opinion was requested to the experts, in order to ensure adequate treatment monitoring at different stages of the patients’ roadmap towards cure (Table 1).
India, United Kingdom and Italy are the top three countries requesting the ERS/WHO TB Consilium services, the majority of patients (49.2%) being born in India. The patients were young (mean age, 33 years), with a significant proportion of paediatric cases (40.2%), extrapulmonary TB forms (14.9%) and M/XDR-TB cases (64.1%). Females account for 43% of the cases.
The majority of the clinical queries are, again, focused on the most appropriate treatment regimen and its duration in M/XDR-TB cases, TB/HIV co-infected individuals and other difficult-to-treat cases which included extrapulmonary and paediatric TB cases. In 13 (19.4%) cases, the clinician requested experts’ opinion about the appropriateness of introducing one of the new TB drugs to treat MDR-TB cases. In 12 cases this request was considered appropriate while in 1 case the experts suggested alternative regimens sparing the new TB drug.
The time necessary to load the cases into the platform remained stable at 20 min, while the average time necessary to provide the clinical feedback by two top global TB experts has slightly increased with the increasing number of consultations, being now at 48 h. This time include also week-ends, holiday time and non-working days, as several requests are submitted on Fridays. Clients confirmed their appreciation for the feedback received.
There are plans to add the translation of the platform into French. In addition, ERS is working hardly to further expand the platform functionality in different areas, as follows:
- A new function related to trans-border migrants has recently completed pre-testing, has been then shown to TB national programme managers and will be launched late in 2015 in Europe in collaboration with WHO, to be then expanded globally. It is aimed at supporting clinicians treating trans-border migrants affected by TB to liaise with the country where the patient is planning to migrate during TB treatment, so that data can be exchanged and continuum of care can be ensured. This functionality will contribute to prevent management errors due to lack of information on the previous patient’s medical history as well as early treatment interruptions after the patient’s migration to a different country or destination.
- A new functionality is under development in collaboration with the civil society organizations, aimed at allowing patients to directly request specific advices for their TB infection or disease to a physician, a nurse, a psychologist, and/or to ask motivational support by other patients who survived the disease.
- Last but not least, a new functionality is under preparation to support clinicians and public health specialists in managing index cases’ contacts and latently infected individuals (including those generated by outbreaks and micro-epidemics).
A plan has been developed to increase the number of experts serving the ERS/WHO TB Consilium in its different functionalities, based on the increasing workload expected in the coming months due to its expanded use in Asia and Latin America. To cope with the new challenges, new experts speaking Spanish, Portuguese and Russian have been recently added to the initial pool of TB Consilium consultants. In addition a coordinator has been identified to run the patients’ branch, in collaboration with European Lung Foundation (ELF), the patients’ voice supported by ERS.
At present two co-directors manage the ERS/WHO Consilium, with the support of one area coordinator. The number of area coordinators will be increased over time, to ensure timely response to all the queries posed.
All the TB Consilium functionalities have been developed based on the requirements of the Swiss legislation in force, which ensures adequate confidentiality and data protection.
The ERS/WHO TB Consilium initiative will represents an effective instrument able to support the new WHO End-TB Strategy focused on the concept of TB pre-elimination (defined as <10 TB cases per million population) and TB elimination (defined as <1 TB case per million) (23).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Raviglione M, Marais B, Floyd K, et al. Scaling up interventions to achieve global tuberculosis control: progress and new developments. Lancet 2012;379:1902-13. [PubMed]
- World Health Organization. Global tuberculosis report 2014. Available online: http://www.who.int/tb/publications/global_report/en/
- Zignol M, van Gemert W, Falzon D, et al. Surveillance of anti-tuberculosis drug resistance in the world: an updated analysis, 2007-2010. Bull World Health Organ 2012;90:111-9D. [PubMed]
- Matteelli A, Centis R, D’Ambrosio L, et al. Multidrug-resistant tuberculosis today. Bull World Health Organ 2012;90:78. [PubMed]
- Abubakar I, Dara M, Manissero D, et al. Tackling the spread of drug-resistant tuberculosis in Europe. Lancet 2012;379:e21-3. [PubMed]
- Skrahina A, Hurevich H, Zalutskaya A, et al. Alarming levels of drug-resistant tuberculosis in Belarus: results of a survey in Minsk. Eur Respir J 2012;39:1425-31. [PubMed]
- Migliori GB, Dara M, de Colombani P, et al. Multidrug-resistant tuberculosis in Eastern Europe: still on the increase? Eur Respir J 2012;39:1290-1. [PubMed]
- Ahuja SD, Ashkin D, Avendano M, et al. Multidrug resistant pulmonary tuberculosis treatment regimens and patient outcomes: an individual patient data meta-analysis of 9,153 patients. PLoS Med 2012;9:e1001300. [PubMed]
- Falzon D, Gandhi N, Migliori GB, et al. Resistance to fluoroquinolones and second-line injectable drugs: impact on multidrug-resistant TB outcomes. Eur Respir J 2013;42:156-68. [PubMed]
- Migliori GB, Sotgiu G, Gandhi NR, et al. Drug resistance beyond extensively drug-resistant tuberculosis: individual patient data meta-analysis. Eur Respir J 2013;42:169-79. [PubMed]
- Blasi F, Dara M, van der Werf MJ, et al. Supporting TB clinicians managing difficult cases: the ERS/WHO Consilium. Eur Respir J 2013;41:491-4. [PubMed]
- Migliori GB, Sotgiu G, D’Ambrosio L, et al. TB and MDR/XDR-TB in European Union and European Economic Area countries: managed or mismanaged? Eur Respir J 2012;39:619-25. [PubMed]
- Falzon D, Jaramillo E, Schünemann HJ, et al. WHO guidelines for the programmatic management of drug-resistant tuberculosis: 2011 update. Eur Respir J 2011;38:516-28. [PubMed]
- Migliori GB, Zellweger JP, Abubakar I, et al. European union standards for tuberculosis care. Eur Respir J 2012;39:807-19. [PubMed]
- van der Werf MJ, Sandgren A, D’Ambrosio L, et al. The European Union standards for tuberculosis care: do they need an update? Eur Respir J 2014;43:933-42. [PubMed]
- Sotgiu G, Pontali E, Centis R, et al. Delamanid (OPC-67683) for treatment of multi-drug-resistant tuberculosis. Expert Rev Anti Infect Ther 2015;13:305-15. [PubMed]
- Salfinger M, Migliori GB. Bedaquiline: 10 years later, the drug susceptibility testing protocol is still pending. Eur Respir J 2015;45:317-21. [PubMed]
- Blasi F, Barnes PJ, Gaga M, et al. Future directions for the ERS: presidential plans. Eur Respir J 2013;42:875-80. [PubMed]
- Blasi F, Reichman LB, Migliori GB. Presenting the European Forum for TB Innovation: innovative thinking in progressing towards TB elimination in Europe. Eur Respir J 2012;40:806-8. [PubMed]
- Diel R, Loddenkemper R, Zellweger JP, et al. Old ideas to innovate tuberculosis control: preventive treatment to achieve elimination. Eur Respir J 2013;42:785-801. [PubMed]
- D’Ambrosio L, Dara M, Tadolini M, et al. Tuberculosis elimination: theory and practice in Europe. Eur Respir J 2014;43:1410-20. [PubMed]
- Voniatis C, Migliori GB, Voniatis M, et al. Tuberculosis elimination: dream or reality? The case of Cyprus. Eur Respir J 2014;44:543-6. [PubMed]
- Migliori GB, Sotgiu G, Blasi F, et al. Towards the development of EU/EEA Standards for Tuberculosis Care (ESTC). Eur Respir J 2011;38:493-5. [PubMed]
- Lönnroth K, Migliori GB, Abubakar I, et al. Towards tuberculosis elimination: an action framework for low-incidence countries. Eur Respir J 2015;45:928-52. [PubMed]
- D’Ambrosio L, Tadolini M, Dupasquier S, et al. ERS/WHO tuberculosis consilium: reporting of the initial 10 cases. Eur Respir J 2014;43:286-9. [PubMed]
- Esposito S, D’Ambrosio L, Tadolini M, et al. ERS/WHO Tuberculosis Consilium assistance with extensively drug-resistant tuberculosis management in a child: case study of compassionate delamanid use. Eur Respir J 2014;44:811-5. [PubMed]
- Codecasa LR, Ciconali G, Mazzola E, et al. Managing an extensively drug-resistant tuberculosis outbreak: the public health face of the medal. Eur Respir J 2015;45:292-4. [PubMed]


