A rare long-term survival of the life-threatening trio: silent myocardial infarction complicated by ventricular septal rupture, type 2 diabetes mellitus and chronic bronchitis
Ventricular septal rupture (VSR) complicating myocardial infarction is rare but life threatening. In the pre-thrombolytic era, ~1-2% of acute myocardial infarction cases were complicated by VSR (1). Reperfusion strategies have led to a reduction to 0.17-0.31% of acute myocardial infarction complicated by VSR (2-4). Unfortunately though, in spite of a decreasing incidence, current mortality among patients with VSR remains high, and appears largely unchanged over the past few decades (2,3,5). Timely diagnosis is key, and definitive surgery, even though challenging associated with high mortality, remains the treatment of choice (3,6). Reports of a long term survival without surgical repair are extremely rare. Our case highlights (I) misdiagnosis of this life-threatening condition for over one month and (II) long term survival of this life-threatening condition on medications independent of corrective surgery.
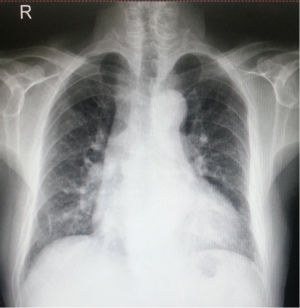
A 74-year-old male was hospitalized for repeated shortness of breath and edema of lower limbs for one month. The patient’s condition had worsened progressively. He has a combined history of diabetes and chronic bronchitis. Past history has no definite evidence of congenital heart disease or primary hypertension. He used to drink alcohol, about 300-350 mL and smoked one pack of cigarettes every day for 40 years. Breathing difficulty, chest discomfort and palpitation on exertion started to appear about half a year ago. These symptoms could be relieved after relaxing for one minute. Sometimes intermittent edema of lower limbs occurred and regressed spontaneously. So the patient didn’t pay any attention to those symptoms. However, edema of lower limbs had become serious over the past one month. Activity tolerance had decreased further. On physical examination, the patient had a regular pulse of 75 beats/min, respiratory rate of 14 breath/min and blood pressure of 110/70 mmHg. A harsh grade III/VI systolic murmur was best heard at the apex and the tricuspid valve region along with tremor, but no distension of the jugular vein. The two lungs had rough breathing sounds and no obvious rales. The 12-lead electrocardiogram at admission (Figure 1) showed sinus rhythm at 75 beats/min, with a premature ventricular contraction. Leads aVF and III showed rS and T-wave inversion. The very small QRS complex was noticed in lead aVF. Cardiac biomarker exam at admission revealed that troponin I was 0.02 ng/mL in normal range, with N terminal pro-natriuretic brain peptide (NT-proBNP) >949.4 pg/mL. Echocardiography (Figure 2) showed the presence of ventricular septal defect about 10 mm, abnormal flow velocity at the site of perforation, and enlargement of right atrium (41 mm) and right ventricle (39 mm). The inferior and inferoseptal segments were abnormal in motion. Chest X-ray (Figure 3) showed aortic type heart without bulging pulmonary segment. Coronary angiography (Figure 4) showed diffuse posterior descending artery (PDA) about 50-70% diameter stenosis without discernible microvasculature in right coronary artery (RCA) system. Left anterior descending (LAD) artery was about 80% diameter stenotic. Left circumflex (LCX) was normal. Although our case was transferred to surgery department, the patient and his relatives denied surgical repair and insisted on being discharged disregarding doctors’ recommendations. He was prescribed aspirin, angiotensin converting enzyme inhibitor, beta blocker and statin at discharge.
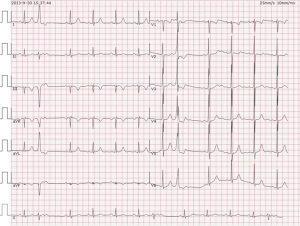

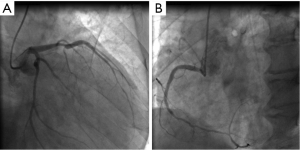
To the best of our knowledge, only five cases reportedly survived the VSR complicating myocardial infarction without surgery for long time (7-12). These cases were all secondary to a clear myocardial infarction accompanied by formation of aneurism, which were different from ours. We first reported a rare long term survival of the life-threatening trio: VSR complicating silent myocardial infarction, diabetes and chronic bronchitis just on medications independent of corrective surgery. VSR after myocardial infarction in our case is confirmative. The patient had no history of congenital heart disease. Furthermore, congenital ventricular septal defect with left to right shunt necessarily involved left ventricle, right ventricle and pulmonary artery system over more than seven decades years long. However, our case showed normal left ventricular chamber on echocardiography and normal pulmonary segment on chest X-ray, which thus failed to support the diagnosis of congenital heart disease. The inferior and inferoseptal walls at basal level were abnormal in motion and became thinning on echocardiography according to standardized myocardial segmentation (13), which strongly supported the diagnosis of VSR after myocardial infarction. In addition, abnormal findings on ECG or coronary angiography all pointed to VSR secondary to myocardial infarction.
Unfortunately, this possibly life-threatening condition had been misdiagnosed for more than one month after initial medical contact. Lack of typical symptoms of chest pain is primarily responsible for this long-time misdiagnosis. Studies have shown that diabetes is a risk factor for silent myocardial infarction as well as advanced age >75 years and male sex (14-16). Our case is a 74-year-old, long-time heavy smoking male inflicted with type 2 diabetes mellitus, which these risk factors together perhaps accounted for occurrence of the silent myocardial infarction, thus leading to misdiagnosis for a relatively long time. Worsening chronic bronchitis was actually as a result of pulmonary edema due to left ventricle dysfunction, which misled the patient to the respiratory outpatient department. For future considerations, systematic diagnostic work-up could avert this misdiagnosis if respiratory physicians attached importance to basic skill trainings.
GUSTO-1 trial demonstrated as high as 94% myocardial infarction patients complicated by VSR would die at day 30 without surgery (3). Unexpectedly, our case had lived well for more than one and a half years, only with mild edema of lower limbs as of the day we prepared this case report. Spontaneous recanalization of blocked RCA contributed to myocardial salvage to a great degree. Very focalized two segments and small septal defect of 10 mm were involved on echocardiography. Less myocardial compromise and small left to right shunt meant more reserved myocardial function and more stable hemodynamic condition, which may have accounted for an extremely rare long-term survival of this life-threatening condition on medications without surgical repair.
Our case is fortunate. But we still want to emphasize the importance of systematic diagnostic work-up, high vigilance for possibility of VSR complicating myocardial infarction in aged patients with diabetes and chronic bronchitis, which may mislead doctors’ judgments and put patients at high risk. Close follow-up of this patient is warranted to know about the natural course, progression and prognosis of this life-threatening trio.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Birnbaum Y, Fishbein MC, Blanche C, et al. Ventricular septal rupture after acute myocardial infarction. N Engl J Med 2002;347:1426-32. [PubMed]
- Moreyra AE, Huang MS, Wilson AC, et al. Trends in incidence and mortality rates of ventricular septal rupture during acute myocardial infarction. Am J Cardiol 2010;106:1095-100. [PubMed]
- Crenshaw BS, Granger CB, Birnbaum Y, et al. Risk factors, angiographic patterns, and outcomes in patients with ventricular septal defect complicating acute myocardial infarction. GUSTO-I (Global Utilization of Streptokinase and TPA for Occluded Coronary Arteries) Trial Investigators. Circulation 2000;101:27-32. [PubMed]
- López-Sendón J, Gurfinkel EP, Lopez de Sa E, et al. Factors related to heart rupture in acute coronary syndromes in the Global Registry of Acute Coronary Events. Eur Heart J 2010;31:1449-56. [PubMed]
- French JK, Hellkamp AS, Armstrong PW, et al. Mechanical complications after percutaneous coronary intervention in ST-elevation myocardial infarction (from APEX-AMI). Am J Cardiol 2010;105:59-63. [PubMed]
- Morillon-Lutun S, Maucort-Boulch D, Mewton N, et al. Therapeutic management changes and mortality rates over 30 years in ventricular septal rupture complicating acute myocardial infarction. Am J Cardiol 2013;112:1273-8. [PubMed]
- Rothfeld EL, Zucker IR, Parsonnet V. Postinfarction ventricular septal defect and the Eisenmenger syndrome. Chest 1972;62:224-6. [PubMed]
- Harikrishnan S, Tharakan J, Titus T, et al. Ventricular septal rupture following myocardial infarction: clinical, haemodynamic, angiographic profile and long-term outcome. Int J Cardiol 2007;120:279-80. [PubMed]
- Sivadasan Pillai H, Tharakan J, Titus T, et al. Ventricular septal rupture following myocardial infarction. Long-term survival of patients who did not undergo surgery. Single-centre experience. Acta Cardiol 2005;60:403-7. [PubMed]
- Landale DG, Schlappi JC. Thirteen-year survival with acquired interventricular septal defect after myocardial infarction. Am Heart J 1962;64:33-7. [PubMed]
- Albagli C, Eshchar J. Perforation of the interventricular septum with survival for five years. Br Heart J 1963;25:536-9. [PubMed]
- Theaker JM. Inferior cardiac aneurysm involving the interventricular septum. A complication of an acquired ventricular septal defect. Br Heart J 1984;51:454-6. [PubMed]
- Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002;105:539-42. [PubMed]
- Jónsdóttir LS, Sigfusson N, Sigvaldason H, et al. Incidence and prevalence of recognised and unrecognised myocardial infarction in women. The Reykjavik Study. Eur Heart J 1998;19:1011-8. [PubMed]
- Sigurdsson E, Thorgeirsson G, Sigvaldason H, et al. Unrecognized myocardial infarction: epidemiology, clinical characteristics, and the prognostic role of angina pectoris. The Reykjavik Study. Ann Intern Med 1995;122:96-102. [PubMed]
- Burgess DC, Hunt D, Li L, et al. Incidence and predictors of silent myocardial infarction in type 2 diabetes and the effect of fenofibrate: an analysis from the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study. Eur Heart J 2010;31:92-9. [PubMed]