Insight into the differences in classification of mediastinal and hilar lymph nodes between Wang’s lymph node map and the International Association for the Study of Lung Cancer lymph node map
Introduction
Lung cancer continues to be the leading cause of cancer-related morbidity and mortality worldwide (1). The key to improving the prognosis of patients with lung cancer is earlier diagnosis and management. Accurate assessment of lymph node involvement is essential in the staging and management of lung cancer. In 1978, Wang and colleagues at Johns Hopkins described in detail the transbronchial needle aspiration (TBNA) biopsy technique for the diagnosis of tumors in the right paratracheal region using a rigid bronchoscope with a rigid 25-gauge esophageal variceal needle (2). In 1983, Wang developed a flexible needle for use with a flexible bronchoscope to perform TBNA (3). It has been shown that use of a flexible bronchoscope to perform TBNA is safe and effective for assessing mediastinal lymph nodes for the diagnosis and staging of lung cancer (4,5). The success of TBNA relies on identifying the lymph node locations and puncture sites accurately, and on improvements to the instrument (6), the ability to push the needle through the bronchial wall, specimen preparation and interpretation (7), and education through hands-on training (8). To improve the diagnostic yield of TBNA, several techniques—including fluoroscopy (9), computed tomography (CT) scan guidance (10), endobronchial ultrasound (EBUS) (11) and electromagnetic navigation (ENB) (12)—have been employed, with the recent introduction of EBUS being the most important. EBUS facilitates not only real-time visualization of lymph nodes and surrounding vessels but also detection of small lymph nodes with greater sensitivity than by CT scan, thereby improving the efficacy of TBNA. EBUS also allows real-time visualization of the needle penetrating the tracheobronchial wall into the mass or lymph nodes to obtain a specimen. The yield of EBUS-TBNA is higher in most lymph node stations and it has a lower complication rate than conventional TBNA (cTBNA) (13,14). A recent study indicated that EBUS elastography of mediastinal and hilar lymph nodes may facilitate prediction of nodal metastasis, and could potentially increase the diagnostic yield of EBUS-TBNA and reduce the number of unnecessary biopsies (15). Hence, EBUS-TBNA is an exciting technology, and represents an important milestone in the development of TBNA. However, the equipment and needles for EBUS-TBNA are expensive, and some patients feel uncomfortable during the procedure; many request that the procedure be performed under general anesthesia (16). The core of EBUS-TBNA is TBNA; visualization may be important to improve the procedure, but is not the key factor. Nothing can replace adequate training for cTBNA and EBUS-TBNA. EBUS should be utilized to enhance reliability, but its use must not reduce the surgical skills required to perform TBNA (16,17).
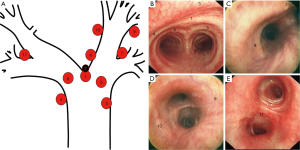
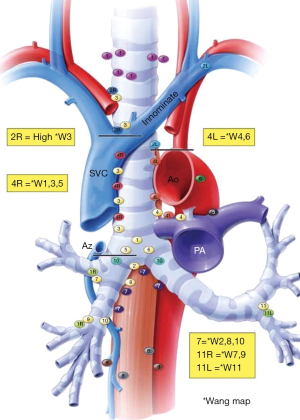
The anatomy and technique for cTBNA are identical to those for EBUS-TBNA. A thorough understanding of lymph node anatomy is critical for both cTBNA and EBUS-TBNA. The first lymph node map was developed by Naruke in 1967, and was initially widely adopted in Japan, North America and Europe. In 1983, the American Thoracic Society (ATS) refined the anatomic descriptors of the Naruke map, which led to the development of the ATS lymph node map. These modifications defined a lymph node anatomy that could be easily identified by mediastinoscopy. In 1994, Wang proposed a chest lymph node map to describe the nomenclature and locations of lymph nodes in the mediastinal and hilar areas on CT scans according to the ATS lymph node map and TBNA technique (18). Wang’s lymph node map has been used to guide TBNA biopsy for the past 20 years, and contains the recommended puncture sites for each lymph node station together with the corresponding airway landmarks (18). The mediastinal and hilar lymph nodes are divided into the following 11 stations: anterior carina lymph nodes (station 1), posterior carina lymph nodes (station 2), right paratracheal lymph nodes (station 3), left paratracheal lymph nodes (station 4), right main bronchus lymph nodes (station 5), left main bronchus lymph nodes (station 6), right upper hilar lymph nodes (station 7), subcarinal lymph nodes (station 8), lower right hilar lymph nodes (station 9), subsubcarinal lymph nodes (station 10), and left hilar lymph nodes (station 11) at four levels: the carina, right main bronchus, bronchus intermedius and left main bronchus (Figure 1) (18). Bronchoscopists can recognize the puncture sites for these lymph node stations using the airway landmarks, which correlate with CT images. Thus cTBNA is not blind, and Wang’s lymph node map enables rapid and accurate identification of puncture sites during EBUS-TBNA.
Others have continued to refine the anatomic descriptors of the Naruke map and elucidate mediastinal lymph node anatomy, which led to the development of other maps such as the Mountain-Dresler modification of the ATS map (MD-ATS), which aimed to unify the Naruke and ATS nodal maps. Although the MD-ATS map had no significant impact on TBNA, it was accepted across North America but was used in Europe only sporadically. In addition, Japanese surgeons and oncologists continued to use the Naruke map, as advocated by the Japan Lung Cancer Society. Important differences in the descriptors of mediastinal lymph nodes exist between the Naruke and MD-ATS lymph node maps. As a result, some tumors staged as N2 according to the MD-ATS map were staged as N1 using the Naruke map. The differences between the Naruke and MD-ATS lymph node maps introduced an irreconcilable discrepancy in data analysis (19). In 2009, a new lung cancer lymph node map was proposed by the International Association for the Study of Lung Cancer (IASLC) to reconcile the differences between the Naruke and the MD-ATS maps and redefine the definitions of the anatomical boundaries of each lymph node station (20); this was incorporated into the seventh edition of the tumor, node, metastasis (TNM) staging system for lung cancer, published by the International Union Against Cancer (UICC) and the American Joint Committee on Cancer (AJCC). In the IASLC lymph-node-mapping system, chest lymph nodes were divided into the following 14 stations: low cervical, supraclavicular and sternal notch nodes (station 1), upper paratracheal nodes (station 2), pre-vascular and retrotracheal nodes (station 3), lower paratracheal nodes (station 4), subaortic lymph nodes (station 5), para-aortic nodes (station 6), subcarinal nodes (station 7), para-esophageal nodes (station 8), pulmonary ligament nodes (station 9), hilar nodes (station 10), interlobar nodes (station 11), lobar nodes (station 12), segmental nodes (station 13) and sub-segmental nodes (station 14) (20). Therefore, the TNM classification according to the IASLC lymph node map is directly related to the treatment and prognosis of lung cancer (21). Wang’s lymph node map plays a pivotal role in TBNA in practice. Thus, it is necessary for the management of lung cancer to understand the differences in, and correlation between, Wang’s map and the IASLC map. Although these differences have been discussed in two preliminary studies (22,23), our understanding of the use of Wang’s lymph node map in the practice of TBNA is incomplete, especially for bronchoscopists in the initial stage of training. If bronchoscopists are not familiar with the lymph node anatomy in Wang’s and the IASLC maps, the yield of TBNA and the staging of lung cancer will be impacted considerably. Thus, it is necessary to investigate the anatomy and correlation of mediastinal and hilar lymph nodes between Wang’s map and the IASLC map.
The correlation of the right mediastinal and hilar lymph nodes between Wang’s map and the IASLC map
The right lymph nodes include stations 1, 3, 5, 7 and 9 in Wang’s lymph node map. Station 1, 3, and 5 lymph nodes are in the mediastinum in Wang’s map (18). Stations 7 and 9 belong to hilar lymph nodes, defined respectively as the right upper and right lower hilar lymph nodes in Wang’s map (18). In the IASLC mapping system, station 1 lymph nodes are defined as low cervical, supraclavicular, and sternal notch nodes, and station 3 lymph nodes are pre-vascular and retrotracheal nodes (20,24). Thus, station 2R, 4R, and 11R lymph nodes in the new IASLC map are correlated with the right lymph nodes in Wang’s map.
The locations of the right lymph nodes in Wang’s map on CT imaging and the puncture sites for TBNA
Station 1 lymph nodes
Station 1 lymph nodes, named anterior carina lymph nodes in Wang’s map, are in front of the intersection of the left and right main bronchi. The lymph nodes can be punctured and sampled at about the 12 o’clock position between the first and second tracheal cartilage rings from the lower trachea.
Station 3 lymph nodes
Station 3 lymph nodes, named as right paratracheal lymph nodes in Wang’s map, are above the azygous arch, and in front of the anterolateral to lower trachea. The lymph nodes range from the lower border of the brachiocephalic vein or the upper border of the aortic arch to the upper margin of the azygous arch. The IASLC 2R is included in station 3 lymph nodes in Wang’s map, and termed upper lymph nodes of station 3. The lymph nodes can be punctured and sampled at about the 1-2 o’clock position between the second and fourth tracheal cartilage rings from the lower trachea.
Station 5 lymph nodes
Station 5 lymph nodes, named the right main bronchus lymph nodes in Wang’s map, are in front of the proximal right main bronchus. The lower border of the lymph nodes is the lower margin of the azygous arch. The lymph nodes can be punctured and sampled at about the 12 o’clock position in the first or second intercartilaginous interspace from the proximal right main bronchus.
Station 7 lymph nodes
Station 7 lymph nodes, named right upper hilar lymph nodes in Wang’s map, are in front of and between the right upper lobe and the bronchus intermedius. The puncture sites for the right upper hilar lymph nodes are at the anterior portion of the right upper bronchus ridge.
Station 9 lymph nodes
Station 9 lymph nodes, named right lower hilar lymph nodes in Wang’s map, are located in the area beside the bronchus intermedius, and include all lymph nodes beside the bronchus intermedius and near the ridge of the right middle lobe and right lower lobe. The puncture sites for the right lower hilar lymph nodes are at the lateral or anterior wall of the bronchus intermedius at about the 3 or 12 o’clock position, near or at the level of the right middle lobe orifice.
The differences in and correlation between the right lymph nodes in Wang’s map and the IASLC map
Station 4R in the IASLC map, named right lower paratracheal lymph nodes, includes the right paratracheal lymph nodes and pretracheal lymph nodes, extending to the left lateral border of the trachea. The upper border of station 4R is the intersection of the caudal margin of the innominate vein with the trachea. The middle line between stations 4R and 4L extends to the left border of the trachea, and the lower border of station 4R extends downward to the lower border of the azygous arch in the IASLC map. Therefore, station 4R in the IASLC map includes stations 1, 3, and 5 in Wang’s map (Figure 2), which are mediastinal lymph nodes. The lymph nodes in the upper region of the right paratracheal are also termed upper lymph nodes of station 3 in Wang’s map, and correspond to station 2R lymph nodes in the IASLC map.
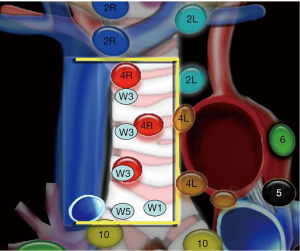
The lymph nodes in front of the proximal right main bronchus, named the right main bronchus lymph nodes (station 5) in Wang’s map, are mediastinal lymph nodes. The lower border of station 4R extends to the lower border of the azygous arch in the IASLC map, and the lymph nodes between the lower rim of the azygous arch and interlobar region on the right are defined as station 10R lymph nodes in the IASLC map. Therefore, the lymph nodes in front of the right main bronchus include some of the station 4R and 10R lymph nodes in the IASLC map. Whether 10R lymph nodes are in the mediastinum in the IASLC map is controversial (20,25). However, there are few patients with lung cancer in which only station 10R lymph nodes are enlarged without enlargement of the proximal right main bronchus lymph nodes. Thus, if there is involvement of a higher station, the practical value of determining the exact boundary for 10R lymph nodes defined on the IASLC map by EBUS in the diagnosis and staging of lung cancer is minimal. In contrast, if station 4R lymph nodes in the IASLC map are subdivided into three groups—anterior carina lymph nodes, right paratracheal lymph nodes and right main bronchus lymph nodes—in Wang’s map, those lymph nodes could be punctured and accurately sampled by TBNA in stations 3, 1, and 5, respectively.
Station 11R lymph nodes are divided into station 11s and 11i lymph nodes in the IASLC map. Station 11s lymph nodes in the IASLC map, which are located between the upper lobe bronchus and bronchus intermedius on the right, coincide with station 7 lymph nodes in Wang’s map, also called right upper hilar lymph nodes. Station 9 lymph nodes in Wang’s map are located in the area beside the bronchus intermedius and near the ridge of the right middle lobe and right lower lobe. Thus, station 9 lymph nodes in Wang’s map include station 11i lymph nodes, which are between the middle and lower lobe bronchi on the right in the IASLC map.
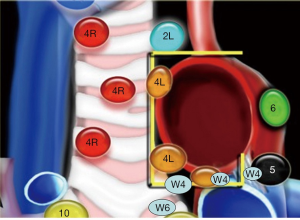
Comparison and correlation of the left mediastinal and hilar lymph nodes between Wang’s map and the IASLC map
The left lymph nodes include stations 4, 6, and 11 in Wang’s lymph node map (Figure 3). Station 4 and 6 lymph nodes are in the mediastinum in Wang’s map (18). Station 11 lymph nodes are classified as hilar lymph nodes and are termed left hilar lymph nodes in Wang’s map (18). Station 6 lymph nodes in the new IASLC map, defined as lymph nodes anterior and lateral to the ascending aorta and aortic arch (20), are different from station 4 lymph nodes in Wang’s map. However, stations 5, 10L, and 11L lymph nodes in the new IASLC map correlate to the left lymph nodes in Wang’s map.
The locations of the left lymph nodes in Wang’s map and their puncture sites for TBNA
Station 4 lymph nodes
Station 4 lymph nodes, named left paratracheal lymph nodes or aortic pulmonary (A-P) window lymph nodes, are left lateral to the trachea near the tracheobronchial angulation, or at the left side of the proximal left main bronchus or tracheobronchial angulation. Lymph nodes between the aortic arch and left pulmonary artery are also called A-P window lymph nodes, and include all lymph nodes medial or lateral to the ligmentum arteriosum. These lymph nodes can be punctured and sampled at about the 9 o’clock position in the first or second intercartilaginous interspace from the left side of the lower trachea.
Station 6 lymph nodes
Station 6 lymph nodes, named left main bronchus lymph nodes, are in front of the proximal left main bronchus. The puncture sites for left main bronchus lymph nodes are at about the 12 o’clock position between the first and second tracheal cartilage rings from the proximal left main bronchus.
Station 11 lymph nodes
Station 11 lymph nodes, named left hilar lymph nodes, are between the left upper lobe and left lower lobe of the bronchus. The puncture sites for left hilar lymph nodes are at the lateral wall of the left lower lobe of the bronchus at about the 9 o’clock position, proximal to the left dorsal bronchus orifice.
The differences in and correlations of left lymph nodes between Wang’s map and the IASLC map
Station 4 lymph nodes in Wang’s map are situated between the space of the aortic arch and left pulmonary artery (i.e., the A-P window), and include the IASLC lower part of 4L and 5. The lymph nodes in the inner window are IASLC 4L, in the mid window are sub-aortic, and in the outer window are IASLC 5 (Figure 3). Station 4 lymph nodes in Wang’s map are located at the left lateral wall of the lower trachea or proximal left main bronchus, or in-between at the tracheobronchial junction. The puncture sites for station 4 lymph nodes in Wang’s map coincide with those for station 4L and 5 lymph nodes in the IASLC map. Stations 4L and 5 lymph nodes in the IASLC map can be sampled in the same direction by adjusting the length of the puncture needle.
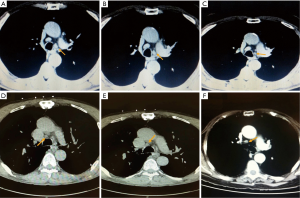
It is important to point out that vessel location in relation to the airway can vary. Station 4 lymph nodes in Wang’s map and station 4L lymph nodes in the IASLC map are often below the upper border of the left pulmonary artery, which results in a risk of down-staging of the patient if vessels are used as landmarks. As shown in Figure 4A-C, the lymph nodes on the left are below the upper margin of the left pulmonary artery, so should be 10L in the IASLC map. However, these are in the mediastinum and are designated as station 4 and 6 lymph nodes in Wang’s map. Use of the IASLC map would result in down-staging of the patient. In Figure 4D,E, the lymph nodes on the right are below the azygous arch, and so they should be classified as 10R. In fact, they are in the mediastinum, as 4R in the IASLC map or stations 1 and 5 in Wang’s map. In such cases, patients would be down-staged if vessels are used as landmarks. In contrast, as shown in Figure 4F, the right lesion is located at about the end of the azygous arch so could be mistaken for 4R if vessels are used as landmarks for staging. In fact, the lesion is at the level of the lumen of the right upper lobe of the bronchus, which is at the distal end of the right main bronchus, and so should be classified as 10R. If only vessels were visualized, the patient would be up-staged. Again, this emphasizes the importance of Wang’s endobronchial landmarks in combination with EBUS visualization of vessels for more accurate staging of lung cancer.
Station 6 lymph nodes in Wang’s map are in the mediastinum, which is anterior to the proximal left main bronchus. Station 10L lymph nodes in the IASLC map include those from the upper rim of the pulmonary artery to the interlobar region. Thus station 6 lymph nodes in Wang’s map are included as station 10L lymph nodes in the IASLC map, including those anterior or lateral to the proximal portion of the left main bronchus.
Station 11L lymph nodes in the IASLC map—including those between the origins of the lobar bronchi, named interlobar lymph nodes—coincide with station 11 lymph nodes, which are designated left hilar lymph nodes in Wang’s map.
The correlation between, and significance of, the central mediastinal lymph nodes in Wang’s map and the IASLC map
The central lymph nodes include stations 2, 8, and 10 in Wang’s lymph node map. All station 2, 8 and 10 lymph nodes are in the mediastinum in Wang’s map (18). Station 7 lymph nodes in the IASLC map, named subcarinal lymph nodes, include those from the carina of the trachea to the lower border of the bronchus intermedius on the right or the upper border of the lower lobe of the bronchus on the left (20). Station 8R lymph nodes in the IASLC map lie adjacent to the wall of the esophagus and to the right of the midline, excluding the subcarinal nodes (20). Station 9 lymph nodes in the IASLC map are defined as pulmonary ligament nodes lying within the pulmonary ligament. The pulmonary ligament nodes have little practical value in the diagnosis of lung cancer. Thus, station 7 and 8R lymph nodes in the new IASLC map are related to the central mediastinal lymph nodes in Wang’s map.
The locations of the central lymph nodes in Wang’s map and the puncture sites for TBNA
Station 2 lymph nodes
Station 2 lymph nodes, named posterior carina lymph nodes, are behind the intersection of the left and right main bronchi, or directly behind the right main bronchus. The lymph nodes range from the intersection of the left and right main bronchi to the upper border of the right upper lobe bronchus orifice on CT imaging. The lymph nodes can be punctured and sampled in the posterior portion of the carina at about the 5-6 o’clock position, and are sometimes closer to the right main bronchus.
Station 8 lymph nodes
Station 8 lymph nodes, named subcarinal lymph nodes, are between the right and left main bronchi, ranging from the upper border of the right upper lobe of the bronchus orifice to the bronchus intermedius orifice. When the right upper lobe bronchus orifice can be seen, the lymph nodes are categorized as subcarinal lymph nodes according to the corresponding CT scan image. The puncture sites for subcarinal lymph nodes are at about the 9 o’clock position in the medial wall of the right main bronchus, proximal to the right upper lobe orifice. If the lesion is punctured inward and backward, the needle tip can reach the level of the orifice of the right upper lobe of the bronchus.
Station 10 lymph nodes
Station 10 lymph nodes, named subsubcarinal lymph nodes, are between the bronchus intermedius and left main bronchus, ranging from the upper to the lower borders of the bronchus intermedius. The puncture sites for subsubcarinal lymph nodes are at about the 9 o’clock position in the medial wall of the bronchus intermedius. Subsubcarinal lymph nodes are widely distributed, and can be punctured and sampled at the upper, middle and lower levels of the bronchus intermedius.
Subsubcarina distal lymph nodes
Station 10 lymph nodes can extend below RML opening, also named subsubcarinal lymph nodes. Thus, station 10 lymph nodes include both the distal portion of station 7 and proximal portion of station 8 in IASLC system. These lymph nodes are located in the region from the entire bronchus intermedius to near the medial basal segment orifice of the right lower lobe. Thus distal subsubcarinal lymph nodes, often on the right side of the esophagus, are located in the area from the distal bronchus intermedius to near the medial basal segment orifice of the right lower lobe. These lymph nodes can be punctured and sampled at the medial posterior wall of the distal bronchus intermedius, proximal to the level of the right lower lobe orifice.
The differences in and significance of the central lymph nodes in Wang’s map and the IASLC map
Station 2, 8 and 10 lymph nodes in Wang’s map belong to the central mediastinal lymph nodes, and coincide with station 7 and proximal 8R lymph nodes in the IASLC map (Figure 5). Subsubcarina distal lymph nodes, also named subsubcarinal lymph nodes, coincide with the proximal part of 8R lymph nodes in the IASLC map. The anatomy of the mediastinal lymph nodes was unclear in the earlier international classification. Subcarinal lymph nodes (station 7) in the past were defined as those from the caudal segment of the carina to the right upper lobe of the bronchus orifice, while the lymph nodes below the bronchus intermedius orifice were defined as interlobar (station 11) or lobar (station 12) lymph nodes. Patients with these nodes are referred for surgery. However, those lymph nodes were located in the mediastinum, and the tumors were staged as at least N2, and stage IIIA in practice. These points have been revised in the new IASLC map. The lower border of station 7 lymph nodes on the right in the new IASLC map extends to the lower border of the bronchus intermedius. Thus, station 7 lymph nodes in the new IASLC map coincide with posterior carina lymph nodes (station 2), subcarinal lymph nodes (station 8), and subsubcarinal lymph nodes (station 10) in Wang’s map, excluding the distal subsubcarina lymph nodes (Figure 5).
Station 2, 8, and 10 lymph nodes in Wang’s map are included as station 7 lymph nodes in the IASLC map (Figure 5). Therefore, the puncture sites for station 7 lymph nodes in the IASLC map are too extensive to ascertain whether station 2, 8, or 10 lymph nodes in Wang’s map were sampled. Meanwhile, the para-esophageal lymph nodes are enlarged in few patients with lung cancer. Consequently, it is not necessary to diagnose and stage lung cancer using only transesophageal needle aspiration (TENA). Thus, the practical value of sampling the more distal station 8 lymph nodes in the IASLC map for the staging of lung cancer is negligible. Moreover, the proximal part of the 8R lymph nodes in the IASLC map can be sampled by puncturing at the distal end of the bronchus intermedius.
Conclusions
TBNA plays a key role in the diagnosis and staging of lung cancer. Identification of the mediastinal and hilar lymph node anatomy, as well as the bronchoscopist’s skill, greatly affects the yield of TBNA. The enlarged lymph nodes may not be single, but rather are arrayed as a chain, or like a string of beads. Unquestionably, an understanding of lymph node anatomy would benefit bronchoscopists. Wang’s lymph node map is a cornerstone for the development of TBNA. The anatomy of the mediastinal and hilar lymph nodes in the IASLC map is directly related to TNM staging of lung cancer. Therefore, we have outlined the important differences between Wang’s map and the IASLC lymph node map in TNM staging to allow bronchoscopists to better understand and correlate these in the prognosis and staging of lung cancer using cTBNA or EBUS-TBNA.
Acknowledgements
Funding: This work was supported by grants from the National Natural Science Foundation of China (No. 81470241, No. 81570018, and No. 81470109) and The Foundation of Science and Technology Department of Zhejiang Province (No. 2014C37022).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [PubMed]
- Wang KP, Terry P, Marsh B. Bronchoscopic needle aspiration biopsy of paratracheal tumors. Am Rev Respir Dis 1978;118:17-21. [PubMed]
- Wang KP, Terry PB. Transbronchial needle aspiration in the diagnosis and staging of bronchogenic carcinoma. Am Rev Respir Dis 1983;127:344-7. [PubMed]
- Wang KP, Brower R, Haponik EF, et al. Flexible transbronchial needle aspiration for staging of bronchogenic carcinoma. Chest 1983;84:571-6. [PubMed]
- Bilaçeroğlu S, Cağiotariotaciota U, Günel O, et al. Comparison of rigid and flexible transbronchial needle aspiration in the staging of bronchogenic carcinoma. Respiration 1998;65:441-9. [PubMed]
- Wang KP, Selcuk ZT. A comparative study of the Wang 21-gauge and 20-gauge needles for bronchoscopic use. J Bronchology 1997;4:201-4.
- Wang KP, Selcuk ZT, Erozan Y. Transbronchial needle aspiration for cytology specimens. Monaldi Arch Chest Dis 1994;49:265-7. [PubMed]
- Haponik EF, Cappellari JO, Chin R, et al. Education and experience improve transbronchial needle aspiration performance. Am J Respir Crit Care Med 1995;151:1998-2002. [PubMed]
- Wang KP, Haponik EF, Britt EJ, et al. Transbronchial needle aspiration of peripheral pulmonary nodules. Chest 1984;86:819-23. [PubMed]
- White CS, Templeton PA, Hasday JD. CT-assisted transbronchial needle aspiration: usefulness of CT fluoroscopy. AJR Am J Roentgenol 1997;169:393-4. [PubMed]
- Shannon JJ, Bude RO, Orens JB, et al. Endobronchial ultrasound-guided needle aspiration of mediastinal adenopathy. Am J Respir Crit Care Med 1996;153:1424-30. [PubMed]
- Diken ÖE, Karnak D, Çiledağ A, et al. Electromagnetic navigation-guided TBNA vs conventional TBNA in the diagnosis of mediastinal lymphadenopathy. Clin Respir J 2015;9:214-20. [PubMed]
- Herth FJ, Eberhardt R, Vilmann P, et al. Real-time endobronchial ultrasound guided transbronchial needle aspiration for sampling mediastinal lymph nodes. Thorax 2006;61:795-8. [PubMed]
- Medford AR, Agrawal S, Free CM, et al. A prospective study of conventional transbronchial needle aspiration: performance and cost utility. Respiration 2010;79:482-9. [PubMed]
- Izumo T, Sasada S, Chavez C, et al. Endobronchial ultrasound elastography in the diagnosis of mediastinal and hilar lymph nodes. Jpn J Clin Oncol 2014;44:956-62. [PubMed]
- Wang KP. EBUS-TBNA of lesions in mediastinum. J Thorac Dis 2010;2:124. [PubMed]
- Huang JA, Browning R, Wang KP. Counterpoint: Should endobronchial ultrasound guide every transbronchial needle aspiration of lymph nodes? No. Chest 2013;144:734-7. [PubMed]
- Wang KP. Staging of bronchogenic carcinoma by bronchoscopy. Chest 1994;106:588-93. [PubMed]
- Rusch VW, Crowley J, Giroux DJ, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the N descriptors in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2007;2:603-12.
- Rusch VW, Asamura H, Watanabe H, et al. The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2009;4:568-77.
- Gu J, Lu C, Guo J, et al. Prognostic significance of the IASLC/ATS/ERS classification in Chinese patients-A single institution retrospective study of 292 lung adenocarcinoma. J Surg Oncol 2013;107:474-80. [PubMed]
- Xia Y, Wang KP. Transbronchial needle aspiration: where are we now? J Thorac Dis 2013;5:678-82. [PubMed]
- Zhang Y, Wang KP. Evolution of transbronchial needle aspiration - a hybrid method. J Thorac Dis 2013;5:234-9. [PubMed]
- Lynch R, Pitson G, Ball D, et al. Computed tomographic atlas for the new international lymph node map for lung cancer: A radiation oncologist perspective. Pract Radiat Oncol 2013;3:54-66. [PubMed]
- Irion KL, Fewins H, Binukrishnan S. Comments on the proposed new international lymph node International Association for the Study of Lung Cancer map. J Thorac Oncol 2009;4:1445; author reply 1445-6. [PubMed]


