Determining optimal fluid and air leak cut off values for chest drain management in general thoracic surgery
Chest tubes are sited in the pleural space at the majority of general thoracic procedure to evacuate air and fluid (1). Post-operative chest drain management and decision for safe removal is very much part of routine surgical care, and most surgeons would favour the shortest duration possible that is considered safe in order to minimise the length of hospital stay. Given their widespread use, one would expect that the management of chest tubes to be uniform but in reality, this is far from the truth (2). Most thoracic surgeons manage drains according to limits that they have carried over from their training or variably in an attempt to “personalise” the drain removal criteria for each patient and procedure rather than use a well-researched standardised protocol (3). Perhaps an important reason is the lack of published research on safety.
Acceptable volume of fluid output and the absence of air leakage are the two common denominators in the decision for the removal of chest tubes (4). Whilst easily measured, significant variation exists for maximum daily volume of pleural fluid output considered “acceptable” for drain removal (5). Air leak assessment is more difficult and subjective when based on visual estimation of bubble counts on forced expiration and despite the introduction of digital air leak monitoring (which overcomes observer variability and subjectivity) the question still remains what level of air leak is considered safe before removing a chest tube (6).
The aims of our study is to ascertain the relationship between chest drain duration and length of hospital stay and define the outcomes associated with increasingly permissive fluid volume and air leak criteria as measured objectively by digital drainage to inform on the appropriate criteria for drain removal/management after general thoracic surgery.
Methods
A retrospective study based on prospectively increasing fluid and air leak protocol on a consecutive series of patients undergoing thoracic surgery procedures under a single surgeon at the Royal Brompton Hospital from January 2009 to 2012.
Patient management
The fluid criteria for chest drain removal during this period increased yearly. In 2007 the criteria for removal was up to 3 mL/kg in 24 hours and the absence of air leak (on coughing) for 24 hours. With each year, the fluid criteria increased by 1 mL/kg to up to 7 mL/kg/24 h in 2011 and from 2012 no further fluid volume criteria was applied (as long as the fluid was not considered to be blood or chyle). From 2012, digital drainage was introduced to measure the rate of air leak (Thopaz, Meleda, Switzerland), and with no further fluid criteria, an air leak criteria of less than 20 mL/min for more than 6 hours was the sole criterion for drain removal. Post-operatively, all patients had a daily chest film until drains were removed and twice weekly thereafter if they remained in hospital. In addition, patients would also have a chest film performed if re-intervention was undertaken (e.g., reinsertion of chest drain for progressive pneumothorax).
Data collection
Patient data was obtained from prospectively collected electronic hospital records and variables such as chest drain duration, number of drains required, hospital length of stay and post-drain removal complications such as pleural effusions and pneumothorax was obtained from review of post-operative digital chest films (Miguel Mesa-Guzman). Radiological measurements were undertaken of post-drain removal digital chest films in the presence of a pneumothorax (from apex to cupola) and fluid (distance from apex of the diaphragm to the fluid level). Patients were excluded from this study if they did not have a drain after surgery (e.g., bronchoscopy) and if the digital chest film images were not available.
Statistical analysis
Baseline characteristics were presented as mean and standard deviation (SD) or medians with interquartile ranges (IQR) for normally and non-normally distributed measures respectively. Kruskall-Wallis test was applied to compare the median drain duration and hospital stay across the years. Frequency data was presented as number and proportions and compared using Fisher’s exact test. The influence of drain and hospital stay was evaluated using linear regression. Statistical analyses were performed on Stata 10.0 (Stata Corp, College Station, USA).
Results
From 2009 to 2012, 626 patients were studied. In total, 160 did not require a chest drain and 22 for which data was unavailable, leaving 444 for analysis. The mean age was 57±19 years and 272 (61%) were men.
On regression analysis (Table 1), the most important influencing factor for the length of hospital stay was identified as the duration of the drain (t-statistic value of 10.45, P<0.001).
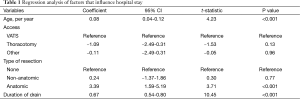
Full table
Using increasing permissive fluid and air leak criteria from 2009-2012, a reduction in the median drain duration from 3 days to 1 day was observed (P<0.001) and accordingly the length of hospital stay from 6 to 4 days (P<0.001) as detailed in Table 2.
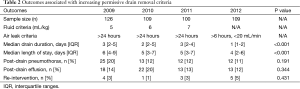
Full table
There was no evidence of increase in the frequency of post-drain removal pneumothoraces (P=0.191), post-drain removal effusions (P=0.344) or re-intervention with drain reinsertion (P=0.431), as increasingly permissive criteria were applied. The mean (SD) size of the post-drain pneumothorax (when present) as measure from the apex of the chest to the top of the lung was 21±13 mm and the mean size of the effusion (when present) as a measure from apex of the diaphragm to the fluid level of 24±12 mm.
Discussion
The result of our study identified the duration of drain as the most important influencing factor for the length of hospital stay. Despite the importance, chest tube management is primarily driven by anecdote rather than scientific evidence (2).
Understanding of physiology and pathophysiology of pleural fluid turnover and lung mechanics is important, considering that information provided in academic textbooks are outdated and can be misleading (7). The pleural space of each hemithorax normally contains 0.130±0.6 mL/kg (8) of hypo-oncotic fluid (composition of a microvascular filtrate with a protein content of approximately 1 gd/L) (9,10). Pleural fluid is produced at parietal pleural level, mainly in the less dependent regions of the cavity and is drained by the lymphatic network in the most dependent part of the cavity, on the diaphragmatic surface and in the mediastinal regions (7). Its volume is a function of the equilibrium achieved between production and reabsorption rates for which normal values have been estimated at 0.01 to 0.02 mL/kg/h (11).
Pleural fluid may also be generated from the visceral pleural, interstitial spaces of the lung or the peritoneal cavity in pathologic states (12). Animal studies have shown that the pleural surfaces are able to increase absorption of fluid from the pleural space in the event of increased production (13,14). Due to this increased rate of absorption, a 10-fold increase in filtration rate results in only 15-20% increase in steady-state pleural fluid volume (15). Extension of these findings to humans suggests that a 70 kg adult should normally be able to reabsorb 470 mL of pleural fluid from each hemithorax per day while the rate of reabsorption in further human studies, in patients with pleural effusions, has been estimated as 0.11 and 0.36 mL/kg/h per hemithorax (16,17). However, it remains unknown how exactly pathophysiologic conditions and medical interventions impact the maximal rate of reabsorption and whether the output of a tube situated in the chest following thoracic procedures provides a realistic measure of the rate at which pleural fluid would otherwise accumulate (12).
If chest tubes remain situated for a prolonged period, it could eventually lead to an undesired inconvenience to patients and risk for infection or other complications. Correct timing of tube removal is essential to patients’ recuperation (18). Patients are usually not discharged from hospital with a chest tube in situ and chest tubes are more frequent than not the cause for a delayed discharge (19). Chest tubes can induce pain and discomfort (20,21), increased risk of infection (22) and hinder pulmonary mechanics (23,24). Conversely, premature removal of chest drains may lead to complications such as pneumothorax and effusion, requiring further management.
We tested the prevailing belief that there is a maximum “safe” fluid criterion for drain removal to prevent the incidence of post-drain removal pleural effusion, and put away the concept that there is a maximum acceptable threshold. A very important caveat is that we ensure that the “fluid” is neither blood nor chyle, and if so, the patients are not managed with the drain removal protocol.
Most physicians typically leave chest tubes in place for at least 24-48 h and until air leak resolves. However, there is less uniformity regarding how (25) and even whether (26) the rate at which fluid is draining through the tube should determine when to remove the tube. Some would go as far as to advocate no chest drains for minimally invasive procedures (27). The introduction of minimal invasive thoracic surgery is probably one of the main reasons for the increased interest in chest tube management since it has managed to lower postoperative pain thus resulting to pain caused by drainage of the chest becoming more prominent (19). It has been reported that with good patient selection, a significant proportion of thoracic surgery can be performed is day surgery units safely and effectively, without the need for chest drainage in the majority of cases (28).
As we have not (yet) moved to the concept of day-case surgery, none of our patients that have an intrathoracic intervention would be discharged on the day of surgery. Moreover, the majority of the drains are removed on the first post-operative day giving rise to a median duration of the drain of 1 day. Therefore the air leak criteria fit our current post-operative management strategy (e.g., we apply effective intercostal blocks and screen for patients who develop pain on the first post-operative day as the blocks wear off).
Digital drainage has made a significant contribution to reducing our post-operative length of stay by changing the paradigm from removing the drain only after a period of absence of air leak on coughing as assessed by underwater seal. This method can be unreliable an occasional “bubble” may be noted by different members of the multi-disciplinary team leading to a further 24 hours of drain duration. The digital output allows the visual confirmation of the presence and rate of air leak per minute, the wave form for the reduction in the size of the leak as it reduces to zero, confirm the duration in which the air leak has stopped and differentiate between no air-leak and a blocked drain. Perhaps the most important contribution is the paradigm shift that allows the drain to safely remove in the presence of a continuing (small) air-leak.
Conclusions
In our study we demonstrate that progressively redesigning our drain removal protocol, and challenging prevailing concepts, allowed the objective removal of drains earlier, reducing hospital length stay for patients and costs for the hospital without increasing post-drain removal complications.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. Lim reports personal fees from Abbott Molecular, Glaxo Smith Kline, Pfizer, Norvatis, Covidien, Roche, Lily Oncology, Boehringer Ingelheim, Medela, grants and personal fees from Medela, ScreenCell; outside the submitted work he is the founder of Informative Genomics, a blood based molecular diagnostic company in London. Other authors have no conflicts of interest to declare.
References
- Laws D, Neville E, Duffy J, et al. BTS guidelines for the insertion of a chest drain. Thorax 2003;58 Suppl 2:ii53-9. [PubMed]
- Brunelli A, Beretta E, Cassivi SD, et al. Consensus definitions to promote an evidence-based approach to management of the pleural space. A collaborative proposal by ESTS, AATS, STS, and GTSC. Eur J Cardiothorac Surg 2011;40:291-7. [PubMed]
- Lee JS, Urschel DM, Urschel JD. Is general thoracic surgical practice evidence based? Ann Thorac Surg 2000;70:429-31. [PubMed]
- Cerfolio RJ, Bryant AS, Skylizard L, et al. Optimal technique for the removal of chest tubes after pulmonary resection. J Thorac Cardiovasc Surg 2013;145:1535-9. [PubMed]
- Tang A, Hooper T, Hasan R. A regional survey of chest drains: evidence-based practice? Postgrad Med J 1999;75:471-4. [PubMed]
- Cerfolio RJ, Bryant AS. The quantification of postoperative air leaks. Multimed Man Cardiothorac Surg 2009;2009:mmcts.2007.003129.
- Miserocchi G. Physiology and pathophysiology of pleural fluid turnover. Eur Respir J 1997;10:219-25. [PubMed]
- Noppen M, De Waele M, Li R, et al. Volume and cellular content of normal pleural fluid in humans examined by pleural lavage. Am J Respir Crit Care Med 2000;162:1023-6. [PubMed]
- Miserocchi G, Agostoni E. Contents of the pleural space. J Appl Physiol 1971;30:208-13. [PubMed]
- Negrini D. Integration of capillary, interstitial and lymphatic function in the pleural space. In: Reed RK, McHale NG, Bert JL, et al. eds. Interstitium Connective Tissues and Lymphatics. London: Portland Press, 1995:283-99.
- Wiener-Kronish JP, Albertine KH, Licko V, et al. Protein egress and entry rates in pleural fluid and plasma in sheep. J Appl Physiol Respir Environ Exerc Physiol 1984;56:459-63. [PubMed]
- Utter GH. The rate of pleural fluid drainage as a criterion for the timing of chest tube removal: theoretical and practical considerations. Ann Thorac Surg 2013;96:2262-7. [PubMed]
- Broaddus VC, Wiener-Kronish JP, Berthiaume Y, et al. Removal of pleural liquid and protein by lymphatics in awake sheep. J Appl Physiol (1985) 1988;64:384-90. [PubMed]
- Bodega F, Agostoni E. Contribution of lymphatic drainage through stomata to albumin removal from pleural space. Respir Physiol Neurobiol 2004;142:251-63. [PubMed]
- Miserocchi G, Venturoli D, Negrini D, et al. Model of pleural fluid turnover. J Appl Physiol (1985) 1993;75:1798-806. [PubMed]
- Leckie WJ, Tothill P. Albumin turnover in pleural effusions. Clin Sci 1965;29:339-52. [PubMed]
- Stewart PB. The rate of formation and lymphatic removal of fluid in pleural effusions. J Clin Invest 1963;42:258-62. [PubMed]
- Abramov D, Yeshayahu M, Tsodikov V, et al. Timing of chest tube removal after coronary artery bypass surgery. J Card Surg 2005;20:142-6. [PubMed]
- Göttgens KW, Siebenga J, Belgers EH, et al. Early removal of the chest tube after complete video-assisted thoracoscopic lobectomies. Eur J Cardiothorac Surg 2011;39:575-8. [PubMed]
- Sienel W, Mueller J, Eggeling S, et al. Early chest tube removal after video-assisted thoracoscopic surgery. Results of a prospective randomized study. Chirurg 2005;76:1155-60. [PubMed]
- Mueller XM, Tinguely F, Tevaearai HT, et al. Impact of duration of chest tube drainage on pain after cardiac surgery. Eur J Cardiothorac Surg 2000;18:570-4. [PubMed]
- Eren S, Esme H, Sehitogullari A, et al. The risk factors and management of posttraumatic empyema in trauma patients. Injury 2008;39:44-9. [PubMed]
- Nomori H, Horio H, Suemasu K. Early removal of chest drainage tubes and oxygen support after a lobectomy for lung cancer facilitates earlier recovery of the 6-minute walking distance. Surg Today 2001;31:395-9. [PubMed]
- Refai M, Brunelli A, Salati M, et al. The impact of chest tube removal on pain and pulmonary function after pulmonary resection. Eur J Cardiothorac Surg 2012;41:820-2; discussion 823. [PubMed]
- Cerfolio RJ, Bryant AS. Results of a prospective algorithm to remove chest tubes after pulmonary resection with high output. J Thorac Cardiovasc Surg 2008;135:269-73. [PubMed]
- Ozdemir A, Misirlioglu AK, Kutlu CA. Does the amount of fluid really matter for drain removal after lung resection? J Thorac Cardiovasc Surg 2008;136:535-6. [PubMed]
- Satherley LK, Luckraz H, Rammohan KS, et al. Routine placement of an intercostal chest drain during video-assisted thoracoscopic surgical lung biopsy unnecessarily prolongs in-hospital length of stay in selected patients. Eur J Cardiothorac Surg 2009;36:737-40. [PubMed]
- Ghosh-Dastidar MB, Deshpande RP, Rajagopal K, et al. Day surgery unit thoracic surgery: the first UK experience. Eur J Cardiothorac Surg 2011;39:1047-50. [PubMed]


