Transthoracic needle biopsy of the lung
Introduction
Image guided transthoracic needle aspiration (TTNA) of lung lesions has been a valuable diagnostic tool since it was first described in 1965 (1). Integral to the evolution of the technique has been the type of image guidance used to direct the biopsy tool to the area of abnormality. As imaging technology has advanced, so has the type of guidance used: plain radiograph and fluoroscopy giving way to computed tomography (CT), ultrasound (US) guided procedures (2,3) and CT guided electromagnetic navigational-TTNA (E-TTNA).
A large body of literature has subsequently explored the technique using CT and US. This literature has focused on the diagnostic accuracy of TTNA, modifications to the biopsy tools used, and the complications. The vast majority of the literature is large case series based with periodic pooled analyses, meta-analyses, and structured reviews of the test characteristics reported (4-7). These analyses have focused on the excellent diagnostic performance of TTNA for the diagnosis of peripheral lung cancer and have included an older and heterogeneous group of procedures guided by plain radiograph, fluoroscopy guided, CT guided, and US.
In this review, we summarize the recent available literature on CT guided and US guided TTNA for lung lesions. Furthermore, we report our case series using a novel electromagnetic navigational technology for TTNA (E-TTNA) and explore future directions in the field (8-10).
Methods
MEDLINE was searched from inception to October 2015 for all case series designed to describe the test characteristics and complications of TTNA of lung nodules using combinations of the medical subject headings (MeSH terms) “computed tomography”, “ultrasound”, “transthoracic”, “needle aspiration”, “needle biopsy”, and “peripheral lung nodules”. Bibliographies and related articles of included studies were hand searched for additional reports. Research analyzing TTNA guided by fluoroscopy alone, an inadequate description of the imaging guidance used, inadequate confirmation of diagnosis, and analyses that included lesions from outside the lung parenchyma were excluded from our pooled analysis. Articles designed to compare biopsy techniques or examine the influence of rapid on-site evaluation (ROSE) on diagnostic yield were excluded. Non-English language articles were also excluded (Figure 1).
For the purposes of the pooled analysis, the overall diagnostic accuracy was defined as the number of true positives (true malignancy found on TTNA) and true negatives (confirmed benign lesions found on TTNA) divided by the number of biopsies done, provided that a definitive diagnosis was achieved based on clinical follow up and/or further invasive testing. Patients who underwent repeat biopsies had each biopsy counted separately. The pooled sensitivity and specificity of TTNA for malignancy was also calculated. If the subset of the test characteristics regarding malignancy were not available, overall diagnostic sensitivity and specificity were reported as indicated in the tables. When reports had adequate diagnostic follow up for only a subset of their study population, the diagnostic accuracy, sensitivity for malignancy, and specificity for malignancy used in the pooled analyses were derived only from the subset with follow up. Primary data was extracted manually from each full text article. When articles calculated the test characteristics of TTNA only after excluding failed procedures (aborted or nondiagnostic) this was noted in the table. Similarly, the safety data was manually extracted and pooled from each full text manuscript.
Results
CT guided TTNA
Diagnostic accuracy
The vast majority of the literature focuses on the diagnostic yield of CT guided TTNA. Forty-eight articles using CT guidance met the inclusion and exclusion criteria based on the search strategy described above. The overall pooled diagnostic accuracy was 92.1% (9,567/10,383) and the sensitivity for detecting malignancy was 92.1% (7,343/7,975). The specificity for the diagnosis of malignancy approaches 100% with rare false positives (Table 1). Within each individual study, one factor consistently proposed as influencing the diagnostic accuracy of TTNA was lung lesion size. However, individual studies were mixed in validating lesion size as a predictor of diagnostic failure and were consistently under powered to detect a difference (14,17,20,22,28,30,31,33,36-39,41-44,52,58). When articles restricted to lung nodules ≤2 cm were analyzed with articles that reported diagnostic accuracy stratified by lesion size ≤2 cm, the pooled diagnostic accuracy was still excellent at 92.8% (2,521/2,718) and the pooled sensitivity for detecting malignancy was similarly high at 92.3% (1,497/1,622) (Table 2). When nodules were further stratified into ≤1 cm lesions the test characteristics did not decline significantly with a pooled diagnostic accuracy of 92.6% (638/689), and a pooled sensitivity for detecting malignancy at 88.7% (410/462).
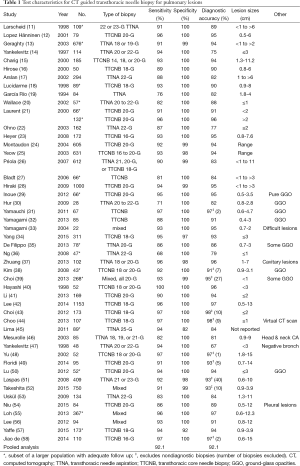
Full table
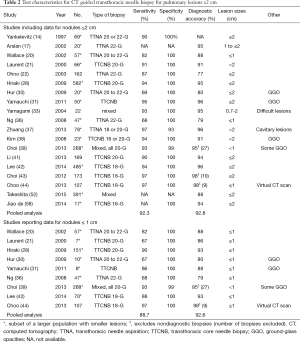
Full table
Another consistent factor proposed as affecting diagnostic yield was the presence of a ground glass opacity (GGO) component to the lesion being biopsied. However, when articles reporting test characteristics of TTNA of GGO were segregated (Table 3), the pooled diagnostic accuracy was still very high at 92.5%, and the pooled sensitivity for detecting malignancy was similar at 91.4% (30-32,35,38,39,50).
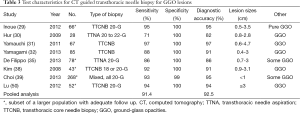
Full table
Several other factors were inconsistently associated with a lower diagnostic yield in univariate and multivariate analyses including lower lobe biopsy site (28,42,52), acquisition of two or fewer specimens (28), malignant lesions (28,52), benign lesions (25), pneumothorax (PTX) during procedure (52), and use of aspiration needle only (39). Regardless of this mixed data (15,23), a high pretest probability of malignancy is a consistent predictor of high diagnostic accuracy as benign lesions were the most difficult to definitively diagnose on TTNA. Articles that studied patients with a lower pretest probability of malignancy reported the lowest diagnostic yield (46,47).
Safety
A sizable amount of case-series data was also available on the safety of CT guided TTNA with seventeen articles identified as specifically describing the complications. Additionally, thirty-six articles designed to describe the test characteristics of CT guided TTNA also provided information on complications encountered (Table 4). Generally, the information regarding the most common complications is dominated by the largest, multi-centered case series with over 15,000 subjects (59).
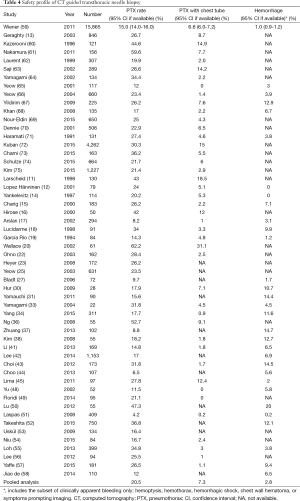
Full table
Overall, PTX is the most common safety issue. PTX occurred with a pooled incidence of 20.5% (6,821/33,306) (Table 4). The overall pooled incidence of chest tube placement for PTX was 7.3% (2,178/29,930) but varied widely (range, 0-31.1%), likely owing to different and evolving management strategies.
Several risk factors for PTX have been proposed in univariate and multivariate analyses including coaxial stabilizing needle size (13,72), age (13,34,57,72,75), smaller lesion size (23,55,60,64,66,69), depth of lesion (22,23,34,41,53,55,60,62-66,69,72-75), wider trajectory angle (41,63), a higher forced vital capacity (22,63), supine position during biopsy (61), longer puncture time (68), needle passing through a pulmonary fissure (69,75), traversing aerated lung (69,71), emphysema within biopsy path (42,43,72,75), presence of emphysema (73,74), number of pleural surfaces crossed (42,72,75), number of punctures (22,34), anterior biopsy approach (72), posterior biopsy approach (72), lateral biopsy approach (34), and a less experienced operator (66). Once a PTX has occurred, several risk factors for chest tube placement have been consistently identified such as age (52,72), supine position during biopsy (52), benign lung lesion on final diagnosis (52), a history of chronic obstructive pulmonary disease (57,59,60,62,72), emphysema within biopsy path (75), presence of emphysema (52,74), smoking history (59), lesion depth (52,63,72), lateral biopsy approach (72), posterior biopsy approach (72), number of pleural surfaces crossed (72), needle passing through a pulmonary fissure (75), and wider trajectory angle (63). However, many of these biologically plausible risk factors are only inconsistently associated with PTX and chest tube placement, likely owing to the heterogeneity of methods and lack of consistent controlling for confounding (15,37,42,56,61,62,67,68,73,74).
Clinically significant hemorrhage is the next most common complication with a pooled incidence of 2.8% (609/22,313) when defined as hemoptysis, hemothorax, hypotension, chest wall hematoma, or symptoms prompting imaging. These clinically significant hemorrhages were considerably less common than evidence of hemorrhage on screening post biopsy CT scan (41,56,68), and PTX (Table 4). Proposed risk factors for any hemorrhage included depth of lesion (41,55,68), number of times the pleura was punctured (68), GGO being biopsied (42,43), and size of the lesion (55,68). Other very rare complications such as cardiac or respiratory arrest, shock, seeding of malignant cells in the biopsy tract, and hemothorax have been reported (76-78). The dreaded complication of air-embolism occurs very rarely with an estimated incidence of 0.02% to 0.07% (52,79).
US guided TTNA
Diagnostic accuracy
There is considerably less data available describing US guided TTNA for lung lesions. A total of ten studies met the inclusion and exclusion criteria for the pooled analysis (Table 5). Lesions amenable to US guided TTNA were abutting the pleura such that aerated lung did not reflect the US beams before the lesion was visible. The overall pooled diagnostic accuracy was similarly high at 88.7% (446/503), and the sensitivity for detecting malignancy was 91.5% (366/400). The specificity for the diagnosis of malignancy also approached 100% (Table 5).

Full table
Small lesions were biopsied with only mixed evidence that lesion size affected diagnostic yield (81,89). Pleural adhesion with a lack of lung sliding was also proposed as increasing diagnostic yield (89). As discussed above, a higher pretest probability of malignancy consistently increased the diagnostic yield as benign lesions were more difficult to definitively diagnose (83-89).
Safety
US guided TTNA was generally very well tolerated with a pooled incidence of PTX of 4.4% (22/503). This compared favorably to CT guided TTNA, however, US guided lesions are inherently more peripheral. Therefore, PTX is less likely regardless of biopsy method used. To our knowledge, the only comparison of US guided and CT guided TTNA reported retrospectively by Sconfienza et al. (90) did find a lower PTX rate with US guidance when biopsying consecutive peripheral lung lesions (14.7% vs. 5.8%). Pleural adhesions with a lack of lung sliding were proposed as protective against PTX (89).
Electromagnetic navigational-transthoracic needle aspiration (E-TTNA)
Although CT and US guided TTNA have been proven safe and effective they do not provide mediastinal staging which is essential in providing prognostic information as well as selecting appropriate surgical and oncologic treatment. A novel thoracic navigational system recently developed by Veran Medical Technologies (St Louis, MO, USA) allows operators to perform a virtual CT guided electromagnetic navigational TTNA using a CT scan of the chest obtained prior to the procedure which is virtually paired with the patient using a tracking pad placed on the chest. This allows the operator to perform mediastinal lymph node staging with convex endobronchial ultrasound (EBUS), navigational bronchoscopy if needed and a navigational E-TTNA all in one setting.
Diagnostic accuracy
A single center safety and feasibility trial of 24 patients using the above system was recently completed showing a diagnostic yield of 83% for E-TTNA (91), which is comparable to the above cited yield using real time imaging. Of note, when EBUS TBNA of mediastinal lymph nodes as well as navigational bronchoscopy using the same system was completed in the same study the diagnostic yield was raised to 92%.
Safety
Using the pilot study cited above, safety of E-TTNA appears to be equivalent to conventional CT guided TTNA. There were five pneumothoraces (20%) after the combined procedure with only two patients requiring pigtail chest tube catheters and admission. There was no other incidence of bleeding, hemoptysis, prolonged intubation or other complications reported.
Although this data is promising, the above pilot data only involves a single center with 24 patients. Further multi-centered, randomized trials with larger enrollment need to be completed before drawing conclusions about the diagnostic accuracy and safety of E-TTNA alone and in comparison to conventional image guided TTNA.
Conclusions
Image guided TTNA remains an important modality in the diagnosis of thoracic diseases, particularly malignancies. This review has shown a high overall diagnostic yield, sensitivity and specificity for pulmonary nodules using CT and US guided imaging after analysis of 75 published articles. E-TTNA was also examined using data from a recent single center pilot study that showed similar diagnostic yield to the two previously mentioned imaging modalities. However, as this is a small, single center study, this data must be taken in context, with further large multi-center trials needed before this modality can be accepted as an alternative to CT or US guided TTNA.
Regarding safety, both CT and US guidance were extremely safe with the two most common complications reported being PTX, a large proportion of which can be managed conservatively with observation rather than tube thoracostomy, as well as hemorrhage. Serious complications including hemothorax, air embolism, or cardiopulmonary arrest have been reported, but are extremely rare. There is a higher reported PTX rate using CT guided imaging as compared to US guidance. This is likely secondary to the fact that US guided biopsies are only performed on nodules and masses that are directly abutting the pleura. E-TTNA also appears to have an equivalent safety profile compared to CT guided TTNA, but again this data must be taken in context as discussed above.
One disadvantage with percutaneous biopsy of potential lung malignancies is the inability to simultaneously stage the mediastinum as is possible with bronchoscopic lung biopsy with simultaneous convex EBUS trans-bronchial needle aspiration of mediastinal lymph nodes. However, as diagnostic yield for bronchoscopic biopsies of peripheral lung nodules remains significantly lower than with CT guided TTNA even under navigational guidance (92), a combined modality of performing EBUS staging, attempted bronchoscopic biopsy and if unsuccessful E-TTNA biopsy of the suspected nodule may provide an efficient and convenient pathway to lung cancer diagnosis and staging for patients in the near future.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Nordenström B. A new technique for transthoracic biopsy of lung changes. Br J Radiol 1965;38:550-3.
- Sheth S, Hamper UM, Stanley DB, et al. US guidance for thoracic biopsy: a valuable alternative to CT. Radiology 1999;210:721-6. [PubMed]
- Birchard KR. Transthoracic needle biopsy. Semin Intervent Radiol 2011;28:87-97. [PubMed]
- Lacasse Y, Wong E, Guyatt GH, et al. Transthoracic needle aspiration biopsy for the diagnosis of localised pulmonary lesions: a meta-analysis. Thorax 1999;54:884-93. [PubMed]
- Rivera MP, Mehta AC, Wahidi MM. Establishing the diagnosis of lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e142S-65S.
- Schreiber G, McCrory DC. Performance characteristics of different modalities for diagnosis of suspected lung cancer: summary of published evidence. Chest 2003;123:115S-128S. [PubMed]
- Rivera MP, Mehta AC. Initial diagnosis of lung cancer: ACCP evidence-based clinical practice guidelines (2nd ed). Chest 2007;132:131S-148S.
- Arias S, Lee H, Semaan R, et al. Use of Electromagnetic Navigational Transthoracic Needle Aspiration (E-TTNA) for Sampling of Lung Nodules. J Vis Exp 2015.e52723. [PubMed]
- Wada H, Anayama T, Hirohashi K, et al. Thoracoscopic ultrasonography for localization of subcentimetre lung nodules. Eur J Cardiothorac Surg 2015. [Epub ahead of print].
- Liu S, Li C, Yu X, et al. Diagnostic accuracy of MRI-guided percutaneous transthoracic needle biopsy of solitary pulmonary nodules. Cardiovasc Intervent Radiol 2015;38:416-21. [PubMed]
- Larscheid RC, Thorpe PE, Scott WJ. Percutaneous transthoracic needle aspiration biopsy: a comprehensive review of its current role in the diagnosis and treatment of lung tumors. Chest 1998;114:704-9. [PubMed]
- Lopez Hänninen E, Vogl TJ, Ricke J, et al. CT-guided percutaneous core biopsies of pulmonary lesions. Diagnostic accuracy, complications and therapeutic impact. Acta Radiol 2001;42:151-5. [PubMed]
- Geraghty PR, Kee ST, McFarlane G, et al. CT-guided transthoracic needle aspiration biopsy of pulmonary nodules: needle size and pneumothorax rate. Radiology 2003;229:475-81. [PubMed]
- Yankelevitz DF, Henschke CI, Koizumi JH, et al. CT-guided transthoracic needle biopsy of small solitary pulmonary nodules. Clin Imaging 1997;21:107-10. [PubMed]
- Charig MJ, Phillips AJ. CT-guided cutting needle biopsy of lung lesions--safety and efficacy of an out-patient service. Clin Radiol 2000;55:964-9. [PubMed]
- Hirose T, Mori K, Machida S, et al. Computed tomographic fluoroscopy-guided transthoracic needle biopsy for diagnosis of pulmonary nodules. Jpn J Clin Oncol 2000;30:259-62. [PubMed]
- Arslan S, Yilmaz A, Bayramgürler B, et al. CT- guided transthoracic fine needle aspiration of pulmonary lesions: accuracy and complications in 294 patients. Med Sci Monit 2002;8:CR493-7. [PubMed]
- Lucidarme O, Howarth N, Finet JF, et al. Intrapulmonary lesions: percutaneous automated biopsy with a detachable, 18-gauge, coaxial cutting needle. Radiology 1998;207:759-65. [PubMed]
- García Río F, Díaz Lobato S, Pino JM, et al. Value of CT-guided fine needle aspiration in solitary pulmonary nodules with negative fiberoptic bronchoscopy. Acta Radiol 1994;35:478-80. [PubMed]
- Wallace MJ, Krishnamurthy S, Broemeling LD, et al. CT-guided percutaneous fine-needle aspiration biopsy of small (< or =1-cm) pulmonary lesions. Radiology 2002;225:823-8. [PubMed]
- Laurent F, Latrabe V, Vergier B, et al. CT-guided transthoracic needle biopsy of pulmonary nodules smaller than 20 mm: results with an automated 20-gauge coaxial cutting needle. Clin Radiol 2000;55:281-7. [PubMed]
- Ohno Y, Hatabu H, Takenaka D, et al. CT-guided transthoracic needle aspiration biopsy of small (< or = 20 mm) solitary pulmonary nodules. AJR Am J Roentgenol 2003;180:1665-9. [PubMed]
- Heyer CM, Reichelt S, Peters SA, et al. Computed tomography-navigated transthoracic core biopsy of pulmonary lesions: which factors affect diagnostic yield and complication rates? Acad Radiol 2008;15:1017-26. [PubMed]
- Montaudon M, Latrabe V, Pariente A, et al. Factors influencing accuracy of CT-guided percutaneous biopsies of pulmonary lesions. Eur Radiol 2004;14:1234-40. [PubMed]
- Yeow KM, Tsay PK, Cheung YC, et al. Factors affecting diagnostic accuracy of CT-guided coaxial cutting needle lung biopsy: retrospective analysis of 631 procedures. J Vasc Interv Radiol 2003;14:581-8. [PubMed]
- Priola AM, Priola SM, Cataldi A, et al. Accuracy of CT-guided transthoracic needle biopsy of lung lesions: factors affecting diagnostic yield. Radiol Med 2007;112:1142-59. [PubMed]
- Bladt O, De Wever W. Additional value of CT-fluoroscopic biopsy of pulmonary lesions: a retrospective study of 69 patients. JBR-BTR 2006;89:298-302. [PubMed]
- Hiraki T, Mimura H, Gobara H, et al. CT fluoroscopy-guided biopsy of 1,000 pulmonary lesions performed with 20-gauge coaxial cutting needles: diagnostic yield and risk factors for diagnostic failure. Chest 2009;136:1612-7. [PubMed]
- Inoue D, Gobara H, Hiraki T, et al. CT fluoroscopy-guided cutting needle biopsy of focal pure ground-glass opacity lung lesions: diagnostic yield in 83 lesions. Eur J Radiol 2012;81:354-9. [PubMed]
- Hur J, Lee HJ, Nam JE, et al. Diagnostic accuracy of CT fluoroscopy-guided needle aspiration biopsy of ground-glass opacity pulmonary lesions. AJR Am J Roentgenol 2009;192:629-34. [PubMed]
- Yamauchi Y, Izumi Y, Nakatsuka S, et al. Diagnostic performance of percutaneous core needle lung biopsy under multi-CT fluoroscopic guidance for ground-glass opacity pulmonary lesions. Eur J Radiol 2011;79:e85-9. [PubMed]
- Yamagami T, Yoshimatsu R, Miura H, et al. Diagnostic performance of percutaneous lung biopsy using automated biopsy needles under CT-fluoroscopic guidance for ground-glass opacity lesions. Br J Radiol 2013;86:20120447. [PubMed]
- Yamagami T, Kato T, Iida S, et al. Percutaneous needle biopsy for small lung nodules beneath the rib under CT scan fluoroscopic guidance with gantry tilt. Chest 2004;126:744-7. [PubMed]
- Yang W, Sun W, Li Q, et al. Diagnostic Accuracy of CT-Guided Transthoracic Needle Biopsy for Solitary Pulmonary Nodules. PLoS One 2015;10:e0131373. [PubMed]
- De Filippo M, Saba L, Concari G, et al. Predictive factors of diagnostic accuracy of CT-guided transthoracic fine-needle aspiration for solid noncalcified, subsolid and mixed pulmonary nodules. Radiol Med 2013;118:1071-81. [PubMed]
- Ng YL, Patsios D, Roberts H, et al. CT-guided percutaneous fine-needle aspiration biopsy of pulmonary nodules measuring 10 mm or less. Clin Radiol 2008;63:272-7. [PubMed]
- Zhuang YP, Wang HY, Zhang J, et al. Diagnostic accuracy and safety of CT-guided fine needle aspiration biopsy in cavitary pulmonary lesions. Eur J Radiol 2013;82:182-6. [PubMed]
- Kim TJ, Lee JH, Lee CT, et al. Diagnostic accuracy of CT-guided core biopsy of ground-glass opacity pulmonary lesions. AJR Am J Roentgenol 2008;190:234-9. [PubMed]
- Choi SH, Chae EJ, Kim JE, et al. Percutaneous CT-guided aspiration and core biopsy of pulmonary nodules smaller than 1 cm: analysis of outcomes of 305 procedures from a tertiary referral center. AJR Am J Roentgenol 2013;201:964-70. [PubMed]
- Hayashi N, Sakai T, Kitagawa M, et al. CT-guided biopsy of pulmonary nodules less than 3 cm: usefulness of the spring-operated core biopsy needle and frozen-section pathologic diagnosis. AJR Am J Roentgenol 1998;170:329-31. [PubMed]
- Li Y, Du Y, Yang HF, et al. CT-guided percutaneous core needle biopsy for small (≤20 mm) pulmonary lesions. Clin Radiol 2013;68:e43-8. [PubMed]
- Lee SM, Park CM, Lee KH, et al. C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of lung nodules: clinical experience in 1108 patients. Radiology 2014;271:291-300. [PubMed]
- Choi JW, Park CM, Goo JM, et al. C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of small (≤ 20 mm) lung nodules: diagnostic accuracy and complications in 161 patients. AJR Am J Roentgenol 2012;199:W322-30. [PubMed]
- Choo JY, Park CM, Lee NK, et al. Percutaneous transthoracic needle biopsy of small (≤ 1 cm) lung nodules under C-arm cone-beam CT virtual navigation guidance. Eur Radiol 2013;23:712-9. [PubMed]
- Lima CD, Nunes RA, Saito EH, et al. Results and complications of CT-guided transthoracic fine-needle aspiration biopsy of pulmonary lesions. J Bras Pneumol 2011;37:209-16. [PubMed]
- Mesurolle B, Mignon F, Meingan P, et al. Head and neck cancer patients with pulmonary nodules: value and role of CT-guided transthoracic needle aspiration biopsies. Head Neck 2003;25:889-94. [PubMed]
- Yankelevitz DF, Henschke CI, Koizumi J, et al. CT-guided transthoracic needle biopsy following indeterminate fiberoptic bronchoscopy in solitary pulmonary nodules. Clin Imaging 1998;22:7-10. [PubMed]
- Yu LS, Deheinzelin D, Younes RN, et al. Computed tomography-guided cutting needle biopsy of pulmonary lesions. Rev Hosp Clin Fac Med Sao Paulo 2002;57:15-8. [PubMed]
- Floridi C, Muollo A, Fontana F, et al. C-arm cone-beam computed tomography needle path overlay for percutaneous biopsy of pulmonary nodules. Radiol Med 2014;119:820-7. [PubMed]
- Lu CH, Hsiao CH, Chang YC, et al. Percutaneous computed tomography-guided coaxial core biopsy for small pulmonary lesions with ground-glass attenuation. J Thorac Oncol 2012;7:143-50. [PubMed]
- Laspas F, Roussakis A, Efthimiadou R, et al. Percutaneous CT-guided fine-needle aspiration of pulmonary lesions: Results and complications in 409 patients. J Med Imaging Radiat Oncol 2008;52:458-62. [PubMed]
- Takeshita J, Masago K, Kato R, et al. CT-guided fine-needle aspiration and core needle biopsies of pulmonary lesions: a single-center experience with 750 biopsies in Japan. AJR Am J Roentgenol 2015;204:29-34. [PubMed]
- Uskül BT, Türker H, Gökçe M, et al. CT-guided transthoracic fine needle aspiration of pulmonary lesions: accuracy and complications in 134 cases. Tuberk Toraks 2009;57:177-85. [PubMed]
- Niu XK, Bhetuwal A, Yang HF. CT-guided core needle biopsy of pleural lesions: evaluating diagnostic yield and associated complications. Korean J Radiol 2015;16:206-12. [PubMed]
- Loh SE, Wu DD, Venkatesh SK, et al. CT-guided thoracic biopsy: evaluating diagnostic yield and complications. Ann Acad Med Singapore 2013;42:285-90. [PubMed]
- Lee WJ, Chong S, Seo JS, et al. Transthoracic fine-needle aspiration biopsy of the lungs using a C-arm cone-beam CT system: diagnostic accuracy and post-procedural complications. Br J Radiol 2012;85:e217-22. [PubMed]
- Yaffe D, Koslow M, Haskiya H, et al. A novel technique for CT-guided transthoracic biopsy of lung lesions: improved biopsy accuracy and safety. Eur Radiol 2015;25:3354-60. [PubMed]
- Jiao de C, Li TF, Han XW, et al. Clinical applications of the C-arm cone-beam CT-based 3D needle guidance system in performing percutaneous transthoracic needle biopsy of pulmonary lesions. Diagn Interv Radiol 2014;20:470-4. [PubMed]
- Wiener RS, Schwartz LM, Woloshin S, et al. Population-based risk for complications after transthoracic needle lung biopsy of a pulmonary nodule: an analysis of discharge records. Ann Intern Med 2011;155:137-44. [PubMed]
- Kazerooni EA, Lim FT, Mikhail A, et al. Risk of pneumothorax in CT-guided transthoracic needle aspiration biopsy of the lung. Radiology 1996;198:371-5. [PubMed]
- Nakamura M, Yoshizako T, Koyama S, et al. Risk factors influencing chest tube placement among patients with pneumothorax because of CT-guided needle biopsy of the lung. J Med Imaging Radiat Oncol 2011;55:474-8. [PubMed]
- Laurent F, Michel P, Latrabe V, et al. Pneumothoraces and chest tube placement after CT-guided transthoracic lung biopsy using a coaxial technique: incidence and risk factors. AJR Am J Roentgenol 1999;172:1049-53. [PubMed]
- Saji H, Nakamura H, Tsuchida T, et al. The incidence and the risk of pneumothorax and chest tube placement after percutaneous CT-guided lung biopsy: the angle of the needle trajectory is a novel predictor. Chest 2002;121:1521-6. [PubMed]
- Yamagami T, Nakamura T, Iida S, et al. Management of pneumothorax after percutaneous CT-guided lung biopsy. Chest 2002;121:1159-64. [PubMed]
- Yeow KM, See LC, Lui KW, et al. Risk factors for pneumothorax and bleeding after CT-guided percutaneous coaxial cutting needle biopsy of lung lesions. J Vasc Interv Radiol 2001;12:1305-12. [PubMed]
- Yeow KM, Su IH, Pan KT, et al. Risk factors of pneumothorax and bleeding: multivariate analysis of 660 CT-guided coaxial cutting needle lung biopsies. Chest 2004;126:748-54. [PubMed]
- Yildirim E, Kirbas I, Harman A, et al. CT-guided cutting needle lung biopsy using modified coaxial technique: factors effecting risk of complications. Eur J Radiol 2009;70:57-60. [PubMed]
- Khan MF, Straub R, Moghaddam SR, et al. Variables affecting the risk of pneumothorax and intrapulmonal hemorrhage in CT-guided transthoracic biopsy. Eur Radiol 2008;18:1356-63. [PubMed]
- Nour-Eldin NA, Alsubhi M, Emam A, et al. Pneumothorax Complicating Coaxial and Non-coaxial CT-Guided Lung Biopsy: Comparative Analysis of Determining Risk Factors and Management of Pneumothorax in a Retrospective Review of 650 Patients. Cardiovasc Intervent Radiol 2015. [Epub ahead of print]. [PubMed]
- Dennie CJ, Matzinger FR, Marriner JR, et al. Transthoracic needle biopsy of the lung: results of early discharge in 506 outpatients. Radiology 2001;219:247-51. [PubMed]
- Haramati LB, Austin JH. Complications after CT-guided needle biopsy through aerated versus nonaerated lung. Radiology 1991;181:778. [PubMed]
- Kuban JD, Tam AL, Huang SY, et al. The Effect of Needle Gauge on the Risk of Pneumothorax and Chest Tube Placement After Percutaneous Computed Tomographic (CT)-Guided Lung Biopsy. Cardiovasc Intervent Radiol 2015;38:1595-602. [PubMed]
- Chami HA, Faraj W, Yehia ZA, et al. Predictors of pneumothorax after CT-guided transthoracic needle lung biopsy: the role of quantitative CT. Clin Radiol 2015;70:1382-7. [PubMed]
- Schulze R, Seebacher G, Enderes B, et al. Complications in CT-Guided, Semi-Automatic Coaxial Core Biopsy of Potentially Malignant Pulmonary Lesions. Rofo 2015;187:697-702. [PubMed]
- Kim JI, Park CM, Lee SM, et al. Rapid needle-out patient-rollover approach after cone beam CT-guided lung biopsy: effect on pneumothorax rate in 1,191 consecutive patients. Eur Radiol 2015;25:1845-53. [PubMed]
- Tomiyama N, Yasuhara Y, Nakajima Y, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol 2006;59:60-4. [PubMed]
- Voravud N, Shin DM, Dekmezian RH, et al. Implantation metastasis of carcinoma after percutaneous fine-needle aspiration biopsy. Chest 1992;102:313-5. [PubMed]
- Müller NL, Bergin CJ, Miller RR, et al. Seeding of malignant cells into the needle track after lung and pleural biopsy. Can Assoc Radiol J 1986;37:192-4. [PubMed]
- Bou-Assaly W, Pernicano P, Hoeffner E. Systemic air embolism after transthoracic lung biopsy: A case report and review of literature. World J Radiol 2010;2:193-6. [PubMed]
- Knudsen DU, Nielsen SM, Hariri J, et al. Ultrasonographically guided fine-needle aspiration biopsy of intrathoracic tumors. Acta Radiol 1996;37:327-31. [PubMed]
- Targhetta R, Bourgeois JM, Marty-Double C, et al. Peripheral pulmonary lesions: ultrasonic features and ultrasonically guided fine needle aspiration biopsy. J Ultrasound Med 1993;12:369-74. [PubMed]
- Yuan A, Yang PC, Chang DB, et al. Ultrasound-guided aspiration biopsy of small peripheral pulmonary nodules. Chest 1992;101:926-30. [PubMed]
- Yang PC, Luh KT, Sheu JC, et al. Peripheral pulmonary lesions: ultrasonography and ultrasonically guided aspiration biopsy. Radiology 1985;155:451-6. [PubMed]
- Chen CC, Hsu WH, Huang CM, et al. Ultrasound-guided fine-needle aspiration biopsy of solitary pulmonary nodules. J Clin Ultrasound 1995;23:531-6. [PubMed]
- Chen CC, Hsu WH, Huang CM, et al. Ultrasound-guided fine needle aspiration biopsy of small pulmonary nodules abutting to the chest wall. Zhonghua Yi Xue Za Zhi (Taipei) 1996;57:106-11. [PubMed]
- Dallari R, Gollini C, Barozzi G, et al. Ultrasound-guided percutaneous needle aspiration biopsy of peripheral pulmonary lesions. Monaldi Arch Chest Dis 1999;54:7-10. [PubMed]
- Khosla R, Rohatgi PK, Seam N. Ultrasound-guided fine needle aspiration biopsy of pleural-based intrathoracic lesions. J Bronchology Interv Pulmonol 2009;16:87-90. [PubMed]
- Hsu WH, Chiang CD, Wang RC, et al. Apical malignancies diagnosed by ultrasound-guided fine needle aspiration biopsy. J Formos Med Assoc 1993;92:983-7. [PubMed]
- Meena N, Bartter T. Ultrasound-guided percutaneous needle aspiration by pulmonologists: a study of factors with impact on procedural yield and complications. J Bronchology Interv Pulmonol 2015;22:204-8. [PubMed]
- Sconfienza LM, Mauri G, Grossi F, et al. Pleural and peripheral lung lesions: comparison of US- and CT-guided biopsy. Radiology 2013;266:930-5. [PubMed]
- Yarmus L, Semaan R, Arias S, et al. Combined Navigational Transthoracic Needle Aspiration and Bronchoscopy for the Diagnosis of Peripheral Pulmonary Nodule: A prospective Human Study. CHEST, Interventional Pulmonary Posters. 2015, Montreal, QC. Available online: http://journal.publications.chestnet.org/article.aspx?articleid=2456700&resultClick=3
- Ost DE, Ernst A, Lei X, et al. Diagnostic Yield and Complications of Bronchoscopy for Peripheral Lung Lesions: Results of the AQuIRE Registry. Am J Respir Crit Care Med 2015. [Epub ahead of print]. [PubMed]



