Effects of different types of antihypertensive agents on arterial stiffness: a systematic review and meta-analysis of randomized controlled trials
Introduction
Hypertension is a major risk factor for cardiovascular diseases and death (1,2). Pathologically, hypertension leads to vascular disease, which represents the key step in the progression to clinical cardiovascular events. In patients with hypertension, increased blood pressure can increase arterial stiffness downstream of increased mechanical stress on vessel walls, endothelial dysfunction, and the excessive activation of the renin-angiotensin-aldosterone system. Furthermore, increased arterial stiffness can cause elasticity loss, reduced compliance, and lowered pressure reflectivity in the arteries, which can further increase the blood pressure, thereby causing a vicious cycle. Significant evidence suggests that the increase in arterial stiffness is an independent risk factor for cardiovascular diseases (3,4), and an ideal antihypertensive agent should both lower blood pressure and improve arterial stiffness.
As methods of monitoring arterial stiffness, pulse wave velocity (PWV) and augmentation index (AI) have been used as indicators in routine arteriosclerosis monitoring. The 2013 guidelines for the management of arterial hypertension by the European Society of Cardiology (ESC) assigned PWV as a new indicator in the risk classification (5), AI was also identified as a risk factor for all-cause mortality and cardiovascular disease in several populations (5). Improvements in PWV have become assessment indicators for the treatment of hypertension (5). Studies have demonstrated that antagonists of angiotensin II receptor, angiotensin converting enzyme inhibitors (ACEIs), beta-blockers and calcium channel blockers (CCBs) may improve arterial stiffness to varying degrees, thereby improving clinical prognosis (6-8).
Previous studies demonstrated that antihypertensive agents of different types or even antihypertensive agents of the same type exhibit differing effects on arterial stiffness (9-11). However, large-scale clinical studies comparing the effect of different types of antihypertensive agents on arterial stiffness are lacking. Thus, this system review and meta-analysis was conducted to systematically review and analyze the clinical benefit of different antihypertensive agents in improving arterial stiffness in hypertensive patients.
Methods
Literature retrieval
The relevant studies published in the PubMed database were retrieved by two of the authors. A Mesh table combined with a keyword search was used as the retrieval method. The Mesh table retrieval formula was as follows: “Pulse Wave Analysis” [Mesh] OR “Vascular Stiffness” [Mesh], “Antihypertensive Agents” [Mesh]. The keyword search included the following terms: arterial stiffness index [Title/Abstract] OR pulse pressure index [Title/Abstract] OR ambulatory pulse pressure index [Title/Abstract] OR arterial stiffness [Title/Abstract] OR artery stiffness [Title/Abstract] OR aortic stiffness [Title/Abstract] OR augmentation index [Title/Abstract] OR pulse wave velocity [Title/Abstract] combined with antihypertensive treatment [Title/Abstract] OR angiotensin-converting enzyme inhibitors [Title/Abstract] OR angiotensin receptor blocker [Title/Abstract] OR beta blockers [Title/Abstract] OR calcium antagonists [Title/Abstract] OR diuretics [Title/Abstract]. The retrieved literature did not include case reports, comments, editorials, letters, or reviews. The language restriction of “English” was added to the search criteria. The reference lists of the included studies were manually searched, and the referenced studies were included in the analysis if they met the inclusion criteria.
Literature screen
The inclusion criteria for the screened literature were as follows: (I) study design: randomized controlled trials (RCTs); (II) study subjects: patients with hypertension; (III) treatment: angiotensin receptor blockers (ARBs) or other types of antihypertensive agents; and (IV) prognostic evaluation of the patients according to improvement in PWV and the AI after receiving different antihypertensive agents. The exclusion criteria for the screened literature were as follows: the presences of diseases other than hypertension, failure to report the research endpoint of the study, and a follow-up time <30 days.
Data extraction
The following data were independently extracted by two authors: first author, year of publication, characteristics of the included subjects, number of enrolled patients, study design, experimental group (number of patients, the used agent and dose), control group (number of patients, the used agent and dose), duration of the intervention treatment, and changes in PWV and the AI. The extracted data were entered into a standard EXCEL file (Microsoft Crop) and were checked by another author. Disagreements in the process of data extraction were resolved by consensus among authors.
The main indicators in this study were improvements of PWV and AI before and after treatment with antihypertensive agents.
Quality evaluation
The two authors who screened the RCTs independently assessed the studies using the Cochrane risk-of-bias tool (12). We assigned a value of low, unclear or high risk of bias according the following domains: random sequence generation, allocation concealment, participants and personnel blinding, outcome assessment blinding, incomplete outcome data, selective reporting and other bias. Disagreements were resolved by consensus.
Statistical methods
Because some studies only provided the mean and standard deviation of the detected indicators in the two groups of patients before and after the treatment (i.e., did not provide the mean and standard deviation of the therapeutic effect), the data were processed as follows, based on the recommendation of Cochrane Handbook: (I) for the studies that only provided the mean and standard deviation of the indicators before and after randomization, the baseline characteristics were assumed to be equal, and the standardized mean difference (SMD) method was directly applied to combine the mean and standard deviation of various indicators after the treatment; (II) for the studies providing the mean and standard deviation of the change of the indicators before and after randomization, the weighted mean difference (MD) method was applied to combine the mean and standard deviation of the therapeutic effect. The therapeutic effect was defined as follows: the results after the treatment-the result before the treatment. The differences were presented as relative risks (RRs) with 95% confidence intervals (CIs) for dichotomous outcomes and as MDs with 95% CIs for continuous outcomes. Heterogeneity across the studies was tested by the I2 statistic, which is a quantitative measure of inconsistency across studies. Studies with an I2 statistic of 25–50% were considered to have low heterogeneity, those with an I2 statistic of 50–75% were considered to have moderate heterogeneity, and those with an I2 statistic of 75% or greater were considered to have high heterogeneity (13). A random effects model was used, regardless of the heterogeneity. A P value <0.05 was considered statistically significant, except where otherwise specified. All statistical analyses were performed using Review Manager Software (Rev Man version 5.2; Nordic Cochrane Centre, Cochrane Collaboration).
Results
The included studies
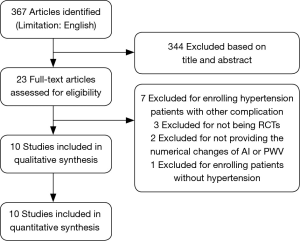
A total of 367 articles were obtained by the search, 344 articles of which were excluded based on the title and abstract. The full text of the remaining 23 articles was reviewed, and 13 articles were excluded. Seven of the articles (14-20) were excluded because they involved the patients with hypertension and other associated diseases, one study (21) included non-hypertensive patients, three studies (22-24) were not RCT studies, and two studies (25,26) did not provide AI or PWV values. No study meeting the inclusion criteria was obtained by the manual searching. Eventually, a total of 10 RCT studies (6,8,27-34) met the inclusion criteria and were included in this meta-analysis. The literature retrieval process is presented in Figure 1.
Characteristics of the selected studies
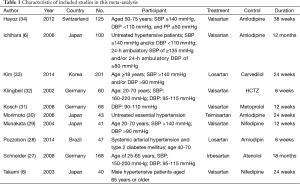
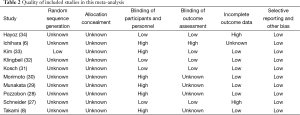
The characteristics of the 10 included RCT studies are presented in Table 1. These RCT studies were published between 2002 and 2014. The number of included subjects was in the range of 40–201 (total: 893). Among the 10 included RCT studies, 7 studies (6,8,29-31,33,34) reported the improvement of PWV with the hypertensive patients randomly assigned to the control group and the experimental (valsartan) group, of which four studies (8,29,33,34) reported the changes of PWV before and after the drug intervention and four studies (6,30,31,33) reported the pre-treatment and post-treatment PWV levels. The improvement in the AI after the randomized treatment was reported in four studies (27,28,32,33), of which three studies (27,32,33) reported the changes of AI before and after the drug intervention, and two studies (28,33) provided the post-treatment AI levels. The evaluation of the quality of the included studies is presented in Table 2.
Full table
Full table
The change in PWV values before and after the treatment
Four studies (8,29,33,34) provided the changes in PWV before and after the drug intervention. Considering the substantial heterogeneity among these studies, a random effect model was used to combine the results. Although the ability of ARB to reduce PWV was superior to other antihypertensive agents (MD: 125.76, 95% CI: −78.70 to 330.23), the difference was not statistically significant (P=0.23), as shown in Figure 2A.
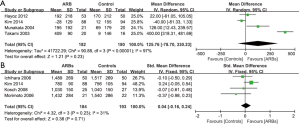
Four studies (6,30,31,33) provided pre-treatment and post-treatment PWV levels, and the PWV values after the treatment were combined using the SMD method. Because the heterogeneity among studies was minor, a fixed effect model was applied. Compared with other antihypertensive agents, the ability of ARB to reduce the PWV was not significant (SMD: 0.04, 95% CI: −0.16 to 0.24, P=0.71), as shown in Figure 2B.
The range of AI variation before and after the treatment
Three studies (27,32,33) provided the changes of AI before and after the drug intervention. Considering the substantial heterogeneity among these studies, a random effect model was used to combine the results. The ability of ARB to lower the level of the AI was superior to other antihypertensive agents (MD: 8.94, 95% CI: 2.18–5.71, P=0.01), as shown in Figure 3A.
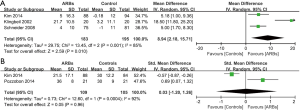
Two studies (28,33) provided the AI values after the treatment, and the studies were combined using SMD method. The abilities of ARB and other anti-hypertensive agents to improve the AI were similar (SMD: 0.03, 95% CI: −1.20 to 1.26, P=0.06), as shown in Figure 3B.
Discussion
This study is a meta-analysis of ten RCT studies to assess the changes in arterial stiffness in patients with hypertension after treatment with the drugs of the ARB class or other types of antihypertensive agents. In the present study, two indicators, PWV and the AI, were used to assess the arteries stiffness. The ability of ARB to improve the PWV level was not observed to be superior to other types of antihypertensive agents, but the ability of ARB to improve the AI level was superior to other types of antihypertensive agents.
Although many clinical studies have reported that compared with other types of antihypertensive agents, the ARB class of antihypertensive agents may improve the arterial stiffness levels in the patients with hypertension. To the best of our knowledge, this is the first meta-analysis to compare the effect of the ARB class of drugs and other types of antihypertensive agents on the improvement of arterial stiffness in the patients with hypertension. The relevant clinical studies included cohort studies and RCTs. To ensure the quality of our study, only the RCTs were included in our meta-analysis.
In this study, the ability of ARB to improve the AI level was superior to other types of antihypertensive agents, but no significant advantage of ARB was observed in improving the PWV compared with other types of antihypertensive agents. The potential reasons for the results are list as follows. First, the antihypertensive drugs in control group include CCB, diuretics, β-blocker, all of these drugs can have effect on heart rate. Although PWV and AI are both indicators for arterial stiffness, the impact factors of the two indicators are different. The biggest difference is that PWV was not influenced by heart rate, whereas AI was influenced by heart rate. Second, the study population in the included studies is different, some study only included elder patients, some studies didn’t set limitation on ages. Considering different kinds of patients have different respond to those kinds of antihypertensive drugs, this heterogeneity may have influence on the results. Third, on purely statistical grounds, as shown in Figure 2A, the actual degree of PWV improvement by ARB was higher than that by other antihypertensive agents. The difference was not statistically significant, primarily due to the small sample size and poor statistical power, suggesting that future research in this area of research is necessary. In addition, Figure 2A presented the results of the meta-analysis based on the changes of PWV in the control group and the ARB group before and after the treatment, which take into consideration the baseline values, whereas Figure 2B is based on the statistics of the PWV values of the ARB group and the control group after the treatment only (the baseline PWV values were assumed to be the same); therefore, the results presented in Figure 2A are more convincing than those presented in Figure 2B.
The peripheral wave reflection was evaluated by the AI, and the AI is an indicator reflecting the amplitude and duration of the global reflected wave (3). PWV can affect the AI by increasing the velocity of the forward and reflected waves. Because the ARB class of drugs was not superior to other types of antihypertensive agents in the improvement of PWV, we can further assess the effect of antihypertensive drugs on arterial stiffness by studying the improvement in the AI. In this study, although the ARB class of drugs was not superior to other antihypertensive agents in the improvement of PWV, the ARB class of antihypertensive drugs was superior to other types of antihypertensive agents in improving the AI. Overall, ARB is superior to other antihypertensive agents in improving arterial stiffness.
Most existing studies have demonstrated that the ARB class of antihypertensive agents is superior to other antihypertensive agents in improving arterial stiffness. The ARB class of antihypertensive agents may improve arterial stiffness due, in part, to its antihypertensive effect; furthermore, ARB drugs can relax the vascular smooth muscle, improve endothelial function and reduce the thickness and collagen content of the arteries, thereby reversing cell hypertrophy in the smooth muscle (35-37). A study had demonstrated that (23) the short term application of the ARBs can improve arterial stiffness, and therefore the improvement of arterial stiffness by the ARBs may be related to the improvement of not only vascular structure but also vascular function. In addition, an in vitro study (38) indicated that angiotensin II can significantly inhibit the expression of adipocyte adiponectin in human, and the ARB class of drugs may improve arterial stiffness by increasing the concentration of serum adiponectin. Furthermore, ARB can reduce the concentration of TNF-α in skeletal muscle and mononuclear cells (although this function has not yet been confirmed), and TNF-α can inhibit the expression and secretion of 3T3-L1 adipocyte adiponectin; therefore, the ARB class of drugs may also enhance the expression and secretion of adipocyte adiponectin through this pathway (39,40).
The clinical studies included in this meta-analysis are all RCTs and the selected articles for this meta-analysis were published between 2002 and 2014, which ensured, to some extent, that the findings of this study are applicable to current clinical practice. Nevertheless, the following limitations still exist in this study. First, the follow-up periods in the different studies are not the same, and previous studies have demonstrated that the mechanism of short-term and long-term drug therapy on arterial stiffness is not the same. Therefore, different follow-up periods may affect the results of the studies. Second, this meta-analysis didn’t compare ARB with different kinds of antihypertensive drugs (such as CCB, diuretic, β-blockers). As mentioned before those antihypertensive drugs have different impact on heart rate, and the impacts of heart rate on PWV and AI are different. Third, this meta-analysis did not assess the improvement of blood pressure by different types of antihypertensive agents. Previous studies have demonstrated that blood pressure and arterial stiffness are correlated. Because the improvement of blood pressure was not assessed in this study, the correlation between the improvement of blood pressure and the improvement of arterial stiffness by different antihypertensive agents could not be analyzed. In addition, whether there are other factors independent of blood pressure in the change of the arterial stiffness by different antihypertensive drugs could not be analyzed. Last but not least, considering the heterogeneity in the included studies (study population and definition of hypertension), the results may be influenced to some degree.
Future research may further assess the change of arterial stiffness by different types of antihypertensive agents from the following aspects. First, future studies can further assess the changes of arterial stiffness by different types of antihypertensive agents with different treatment durations and further analyze the mechanism of these changes in short-term and long-term antihypertensive agent treatment. Second, whether different types of antihypertensive agents can affect arterial stiffness independent of blood pressure changes can be further assessed, and the corresponding mechanism can be further investigated. Finally, the existing studies analyzed hypertensive patients whose clinical conditions were complicated by dialysis, diabetes or obesity, suggesting that the ARB class of drugs may also improve arterial stiffness in these patients. Future studies may further evaluate the change of arterial stiffness by different antihypertensive agents in hypertension patients complicated with other risk factors.
Conclusions
The effect of ARB on the improvement of the PWV level is not superior to other types of antihypertensive agents, but ARB is superior to other types of antihypertensive agents for improving the AI level. Overall, to improve of arterial stiffness, ARB maybe is superior to other antihypertensive agents.
Acknowledgements
Novartis Pharma China supported this meta-analysis by reference searching and collecting.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kannel WB. Historic perspectives on the relative contributions of diastolic and systolic blood pressure elevation to cardiovascular risk profile. Am Heart J 1999;138:205-10. [PubMed]
- Kannel WB. Elevated Systolic Blood Pressure as a Cardiovascular Risk Factor. Am J Cardiol 2000;85:251-5. [PubMed]
- Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006;27:2588-605. [PubMed]
- Najjar SS, Scuteri A, Shetty V, et al. Pulse wave velocity is an independent predictor of the longitudinal increase in systolic blood pressure and of incident hypertension in the Baltimore Longitudinal Study of Aging. J Am Coll Cardiol 2008;51:1377-83. [PubMed]
- Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013;34:2159-219. [PubMed]
- Ichihara A, Kaneshiro Y, Takemitsu T, et al. Effects of amlodipine and valsartan on vascular damage and ambulatory blood pressure in untreated hypertensive patients. J Hum Hypertens 2006;20:787-94. [PubMed]
- Karalliedde J, Smith A, DeAngelis L, et al. Valsartan improves arterial stiffness in type 2 diabetes independently of blood pressure lowering. Hypertension 2008;51:1617-23. [PubMed]
- Takami T, Shigemasa M. Efficacy of various antihypertensive agents as evaluated by indices of vascular stiffness in elderly hypertensive patients. Hypertens Res 2003;26:609-14. [PubMed]
- Ong KT, Delerme S, Pannier B, et al. Aortic stiffness is reduced beyond blood pressure lowering by short-term and long-term antihypertensive treatment: a meta-analysis of individual data in 294 patients. J Hypertens 2011;29:1034-42. [PubMed]
- Protogerou AD, Stergious GS, Vlachopoulos C, et al. The effect of antihypertensive drugs on central blood pressure beyond peripheral blood pressure. Part II: Evidence for specific class-effects of antihypertensive drugs on pressure amplification. Curr Pharm Des 2009;15:272-89. [PubMed]
- Koumaras C, Tzimous M, Stavrinou E, et al. Role of antihypertensive drugs in arterial 'de-stiffening' and central pulsatile hemodynamics. Am J Cardiovasc Drugs 2012;12:143-56. [PubMed]
- Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [PubMed]
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [PubMed]
- Spanos G, Kalaitzidis R, Karasavvidou D, et al. Efficacy of aliskiren and valsartan in hypertensive patients with albuminuria: a randomized parallel-group study. J Renin Angiotensin Aldosterone Syst 2013;14:315-21. [PubMed]
- Frimodt-Møller M, Kamper AL, Strandgaard S, et al. Beneficial effects on arterial stiffness and pulse-wave reflection of combined enalapril and candesartan in chronic kidney disease--a randomized trial. PLoS One 2012;7:e41757. [PubMed]
- Nedogoda SV, Ledyaeva AA, Chumachok EV, et al. Randomized trial of perindopril, enalapril, losartan and telmisartan in overweight or obese patients with hypertension. Clin Drug Investig 2013;33:553-61. [PubMed]
- Peters CD, Kjaergaard KD, Jensen JD, et al. No significant effect of angiotensin II receptor blockade on intermediate cardiovascular end points in hemodialysis patients. Kidney Int 2014;86:625-37. [PubMed]
- Mitsuhashi H, Tamura K, Yamauchi J, et al. Effect of losartan on ambulatory short-term blood pressure variability and cardiovascular remodeling in hypertensive patients on hemodialysis. Atherosclerosis 2009;207:186-90. [PubMed]
- Miyashita Y, Miyashita Y, Saiki A, et al. Effects of olmesartan, an angiotensin II receptor blocker, and amlodipine, a calcium channel blocker, on Cardio-Ankle Vascular Index (CAVI) in type 2 diabetic patients with hypertension. J Atheroscler Thromb 2009;16:621-6. [PubMed]
- Shigenaga A, Tamura K, Dejima T, et al. Effects of angiotensin II type 1 receptor blocker on blood pressure variability and cardiovascular remodeling in hypertensive patients on chronic peritoneal dialysis. Nephron Clin Pract 2009;112:c31-40. [PubMed]
- Rajagopalan S, Kariisa M, Dellegrottaglie S, et al. Angiotensin receptor blockade improves vascular compliance in healthy normotensive elderly individuals: results from a randomized double-blind placebo-controlled trial. J Clin Hypertens (Greenwich) 2006;8:783-90. [PubMed]
- Eguchi K, Hoshide S, Ishikawa S, et al. Aggressive blood pressure-lowering therapy guided by home blood pressure monitoring improves target organ damage in hypertensive patients with type 2 diabetes/prediabetes. J Clin Hypertens (Greenwich) 2012;14:422-8. [PubMed]
- Agata J, Nagahara D, Kinoshita S, et al. Angiotensin II receptor blocker prevents increased arterial stiffness in patients with essential hypertension. Circ J 2004;68:1194-8. [PubMed]
- Rehman A, Rahman AR, Rasool AH. Effect of angiotensin II on pulse wave velocity in humans is mediated through angiotensin II type 1 (AT(1)) receptors. J Hum Hypertens 2002;16:261-6. [PubMed]
- Jekell A, Malmqvist K, Wallén NH, et al. Markers of inflammation, endothelial activation, and arterial stiffness in hypertensive heart disease and the effects of treatment: results from the SILVHIA study. J Cardiovasc Pharmacol 2013;62:559-66. [PubMed]
- Park JB, Intengan HD, Schiffrin EL. Reduction of resistance artery stiffness by treatment with the AT(1)-receptor antagonist losartan in essential hypertension. J Renin Angiotensin Aldosterone Syst 2000;1:40-5. [PubMed]
- Schneider MP, Delles C, Klingbeil AU, et al. Effect of angiotensin receptor blockade on central haemodynamics in essential hypertension: results of a randomised trial. J Renin Angiotensin Aldosterone Syst 2008;9:49-56. [PubMed]
- Pozzobon CR, Gismondi RA, Bedirian R, et al. Functional Vascular Study in Hypertensive Subjects with Type 2 Diabetes Using Losartan or Amlodipine. Arq Bras Cardiol 2014;103:51-9. [PubMed]
- Munakata M, Nagasaki A, Nunokawa T, et al. Effects of valsartan and nifedipine coat-core on systemic arterial stiffness in hypertensive patients. Am J Hypertens 2004;17:1050-5. [PubMed]
- Morimoto S, Yano Y, Maki K, et al. Renal and vascular protective effects of telmisartan in patients with essential hypertension. Hypertens Res 2006;29:567-72. [PubMed]
- Kosch M, Levers A, Lang D, et al. A randomized, double-blind study of valsartan versus metoprolol on arterial distensibility and endothelial function in essential hypertension. Nephrol Dial Transplant 2008;23:2280-5. [PubMed]
- Klingbeil AU, John S, Schneider MP, et al. AT1-receptor blockade improves augmentation index: a double-blind, randomized, controlled study. J Hypertens 2002;20:2423-8. [PubMed]
- Kim EJ, Song WH, Lee JU, et al. Efficacy of losartan and carvedilol on central hemodynamics in hypertensives: a prospective, randomized, open, blinded end point, multicenter study. Hypertens Res 2014;37:50-6. [PubMed]
- Hayoz D, Zappe DH, Meyer MA, et al. Changes in aortic pulse wave velocity in hypertensive postmenopausal women: comparison between a calcium channel blocker vs angiotensin receptor blocker regimen. J Clin Hypertens (Greenwich) 2012;14:773-8. [PubMed]
- Levy BI, Michel JB, Salzmann JL, et al. Remodeling of heart and arteries by chronic converting enzyme inhibition in spontaneously hypertensive rats. Am J Hypertens 1991;4:240S-5S. [PubMed]
- Isobe N, Taniguchi K, Oshima S, et al. Candesartan cilexetil improves left ventricular function, left ventricular hypertrophy, and endothelial function in patients with hypertensive heart disease. Circ J 2002;66:993-9. [PubMed]
- Barra JG, Levenson J, Armentano RL, et al. In vivo angiotensin II receptor blockade and converting enzyme inhibition on canine aortic viscoelasticity. Am J Physiol 1997;272:H859-68. [PubMed]
- Sharma AM, Janke J, Gorzelniak K, et al. Angiotensin blockade prevents type 2 diabetes by formation of fat cells. Hypertension 2002;40:609-11. [PubMed]
- Maeda N, Takahashi M, Funahashi T, et al. PPARgamma ligands increase expression and plasma concentrations of adiponectin, an adipose-derived protein. Diabetes 2001;50:2094-9. [PubMed]
- Togashi N, Ura N, Higashiura K, et al. The contribution of skeletal muscle tumor necrosis factor-alpha to insulin resistance and hypertension in fructose-fed rats. J Hypertens 2000;18:1605-10. [PubMed]