A new approach for video-assisted thoracoscopic lobectomy “the caudal position”
Introduction
Video-assisted thoracoscopic lobectomy (VATS-Lobectomy) was first reported by Roviaro in the 1992 (1). Initially the surgeons’ community has several doubts about the feasibility and oncological radicality that this technique could guarantee. Nowadays, we know that VATS lobectomy gain comparable results with the open lobectomy and thus the number of patients underwent VATS lobectomy has increasing every year (2,3). We describe a new patient’s position and surgical approach to perform VATS-lobectomy.
Materials and Methods
Preoperatively patients were studied with spirometry and carbon monoxide diffusion capacity. Lung cancer staging was performed with total body contrast-enhanced computed tomography, positron emission tomography and EBUS guided bronchoscopy and/or mediastinoscopy. All patients were scheduled for minimally invasive approach if the nodule dimension was less than 5-cm without clear signs of major infiltration of mediastinal structures and chest wall or proximal disease requiring pneumonectomy.
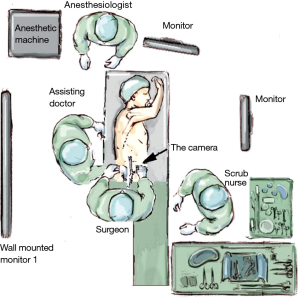
Under general anesthesia and double-lumen intubation, the patient is placed in a lateral decubitus position, and the padded arms are placed unsupported in the “prayer” position in front of the face. Both legs are positioned together flexed like in a sitting position and padded with pillows. One of the inferior components of the surgical table is removed to allow the first surgeon working from the caudal side of the patient (Figure 1). The table is arched at the level of xiphoid process to open the intercostals space maximally. The first monitor is positioned over the head of the patient directly in front of the surgeon who’s performing surgical procedure in a bimanual fashion. The assistant stays on the dorsal side of the patient, watching the second monitor on the opposite side holding and moving the camera. The scrub nurse stays on the ventral side of the patient, watching the first monitor (Figure 2).
Surgery was performed through three ports. We always use a 30° 10 mm video-camera. The first port “4-cm utility port” was made on the 4th intercostal space between the latissimus-dorsi and the anterior-axillary line, the second “1-cm camera-port” on the 7th/8th-intercostal space on the posterior-axillary line, the third “1cm operative port” on 7th/8th-intercostal space more posteriorly over the hypothetical line down from the scapula (Figure 1). During the procedure the configuration of the instrument position remains the same even during lymphadenectomy. The stapler is always introduced from the first port. During lymphadenectomy the camera is switched in the 3th-port and the instrument like grasper or electrothermal bi-polar sealings-system place in the 2th-port. During the procedure the surgical bed position is modified as follow. The surgical table was tilted from 0 to 30° on the right to have a better vision of the posterior aspect of the hilum or to perform station 7, 8, 9 lymph node dissection, on the contrary the bed was tilted from 0 to 30° on the left to have optimal control of the anterior aspect of the pulmonary hilum (Figure 3). The bed was then moved in anti-Trendelenburg position to have optimal vision of the fissures and during paratracheal or pulmonary window lymph node dissection. Indeed, Trendelenburg position was used to have a better access to the pulmonary ligament and thus inferior pulmonary vein (Figure 4). The normal sequence of dissection during VATS-lobectomy is: first the pulmonary ligament, pulmonary vein (inferior or superior or middle), pulmonary artery, bronchus and fissures. Just in case of middle lobectomy we perform after the vein the bronchus first and the n the artery. The vascular structures are dissected and sealed following an anterior approach (6,7), instead the bronchus is approached following a posterior approach (3).


From January 2015 we perform 23 “caudal VATS-lobectomy” for NSCLC. We performed 6 inferior-right-lobectomy, 6 superior-right-lobectomy, 4 inferior-left-lobectomy, 4 superior-left-lobectomy and 3 middle-lobectomy. We had no intraoperative complications. The mean operative-time was 152.4±37 min. We had no prolonged air leak, and the chest tube was removed after a mean of 2.2±1.5 days post-operatively. All patients were discharged in good general condition after a mean of 5.36±1.9 days.
Discussion
Nowadays VATS-lobectomy is becoming a routine procedure for selected patients with lung cancer and VATS-lobectomy has spread around the world. Previous studies demonstrated oncological results comparable with the open approach, moreover the VATS technique have some advantages in particular, less post-operative pain, better preservation of the pulmonary function, shorter hospital stay and obviously better cosmesis (2,3,6). Nevertheless VATS-lobectomy does not translate into a unique standardized surgical technique. In these years numerous technical variations have been described in literature. The main difference are about the number of the ports, triportal, biportal, monoportal and the side from which the hilar structures of the lung was managed, anteriorly or posteriorly (7-11). On the basis of that the first surgeon need to work from the back (3) or in front of the patient (7). To date nobody demonstrate clear benefits and superior results with a technique over another. The choice of which technique is used perform VATS-lobectomy depends on the preferences and experience of each individual surgeons. In our department we start the VATS program using the anterior three portal approaches (7). After we gaining a good expertise with VATS-lobectomy we begun to change the starting technique to improve some technical aspects that in our hands made the procedure less comfortable and challenging. We studied a position in which the operator stays from the inferior side of the thorax, positioning the patients in a lateral sitting position (Figure 1). In this way, the lung apex corresponding to the north of an imaginary compass, the base of the lung is the south, the anterior hilum the east and the posterium hilum the west. This spatial correspondence between the anatomy of the chest, the limbs and tools in the hands of the surgeon makes in our opinion his movements very intuitive and natural. This inferior position ensures the operator to enjoy all the benefits of the anterior and posterior VATS approach limiting the disadvantages of both. Indeed we have an optimal surgical window on the anterium and posterium hilum, a complete control of the fissures anteriorly and posteriorly. This approach also makes it very easy and intuitive lymphadenectomy. The surgeon maneuvers are further assisted and simplified by the movement of the surgical bed (Figures 3,4). In fact, the rotation of the bed to the left of the operator facilitates the vision and dissection of the anterior hilum, while the rotation to the right facilitates the management of the posterior hilum. Again tilting the bed in Trendelenburg position facilitates the control of the inferior structures of the chest like pulmonary ligament or the inferior pulmonary vein or the lymphadenectomy of station 8 and 9. Contrariwise, placing the bed in anti- Trendelenburg position can gain an optimal vision of the major fissure, pulmonary apex and paratracheal space or pulmonary window space. Until now we perform caudal-VATS approach with three ports as describe above. We had no conversion to open surgery or surgical complications in particular related with the position of the patient, the operative time was acceptable for a VATS-lobectomy. We never change our approach, during surgery, from the caudal to the anterior or posterior one. Probably, in the future, the acquisition of greater experience with this new approach will make us able to correctly perform lobectomy with bi-portal or maybe single-portal technique.
In conclusion we think that our new position could be considered a further effective technical variation to perform VATS-lobectomy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- Whitson BA, Groth SS, Duval SJ, et al. Surgery for early-stage non-small cell lung cancer: a systematic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg 2008;86:2008-16; discussion 2016-8.
- Walker WS, Codispoti M, Soon SY, et al. Long-term outcomes following VATS lobectomy for non-small cell bronchogenic carcinoma. Eur J Cardiothorac Surg 2003;23:397-402. [PubMed]
- Dolci G, Dell’Amore A, Daddi N. Surgical table adjustment for anterior and posterior dissection of the pulmonary hilum and lymphadenectomy. Asvide 2015;2:159. Available online: http://www.asvide.com/articles/737
- Dolci G, Dell’Amore A, Daddi N. Surgical table adjustment for dissection of the upper and inferior structures of the chest and lung fissures. Asvide 2015;2:160. Available online: http://www.asvide.com/articles/738
- Petersen RH, Hansen HJ. Learning thoracoscopic lobectomy. Eur J Cardiothorac Surg 2010;37:516-20. [PubMed]
- Hansen HJ, Petersen RH, Christensen M. Video-assisted thoracoscopic surgery (VATS) lobectomy using a standardized anterior approach. Surg Endosc 2011;25:1263-9. [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [PubMed]
- Gonzalez-Rivas D. VATS lobectomy: surgical evolution from conventional VATS to uniportal approach. Scientific World Journal 2012;2012:780842.
- Rocco G, Internullo E, Cassivi SD, et al. The variability of practice in minimally invasive thoracic surgery for pulmonary resections. Thorac Surg Clin 2008;18:235-47. [PubMed]
- Rocco G. One-port (uniportal) video-assisted thoracic surgical resections--a clear advance. J Thorac Cardiovasc Surg 2012;144:S27-31. [PubMed]