Electromagnetic navigation bronchoscopy guided injection of methylene blue combined with hookwire for preoperative localization of small pulmonary lesions in thoracoscopic surgery
Introduction
The current review confirms that video-assisted thoracoscopic surgery (VATS) is a superior procedure than open lobectomy in lung resection (1). However, the accurate localization prior to VATS is very significant to the resection of small lung lesions (2). There are a variety of clinical methods, such as placing hookwire, coil, dye marking, fiducial marker placement and so on (3-7), to localize small lesions at present. While each method has its benefits as well as its limitations, a combined method that utilizes the advantages of different fashions might result in more accurate in the localization of small lung lesions and a rare incidence of complications. We describe a modality using an electromagnetic navigation bronchoscopy (ENB) guided injection of methylene blue combined with percutaneous hookwire to localize the small lung lesions. To our knowledge, it is the first publication describing localization of small pulmonary lesion by using ENB guided injection of methylene blue combined with hookwire.
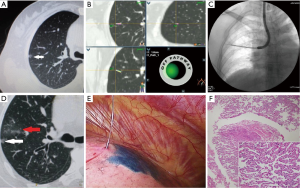
Case presentation (Figures 1,2)

A 50-year-old female patient presented to our hospital complaining of finding a lung shadow of the right upper lobe in physical examination 6 months ago. There was no fever, cough, hemoptysis and other symptoms. She was healthy previously and no smoking history. So no measures were taken but the patient was asked to follow-up. She was received a reexamination in our hospital and the chest computed tomography (CT) scan showed that there was a small ground glass opacity with the size of about 0.6 cm × 0.5 cm in the subpleural area of the right upper lobe. The ground glass opacity had a mild lobulation and an uneven density (Figure 1A). The patient received two weeks’ anti-inflammatory treatment and came to our hospital. A CT scan was performed in order to confirm the effect. But it showed that there was no significant change compared with the previous one. Relevant inspections including blood test, coagulation function, lung function and electrocardiogram were all normal. The patient required to perform surgical operation to identify the diagnosis. The lesion located in the subpleural area and had a mild leaf and an uneven density. It was considered to be an early adenocarcinoma in situ according to the multidisciplinary consultation. Given that the patient strongly demanded to undergo surgery, we decided to give the patient an accurate preoperative localization followed by VATS. So the method of ENB guided injection of methylene blue combined with percutaneous hookwire was selected to localize the lesion.
ENB (superDimension, Covidien, USA) was performed under local anesthesia and moderate sedation with midazolam and fentanyl. Keep the patient’s venous channel available and continue to offer oxygen. Vital signs were monitored constantly. A bronchoscope (BF-1T260, Olympus, Japan) together with the navigational system was used as previously described in the literature (9). Electromagnetic navigation system created an electromagnetic field around the patient’s chest. The locatable guide (LG) was inserted the bronchoscope through the extended working channel (EWC). Once the sensor probe of the LG was placed within the electromagnetic field, its position in the X, Y, and Z planes, as well as its orientation (roll, pitch, and yaw movements) were captured by the electromagnetic navigation system. This information was then displayed on a monitor in real time. The monitor displayed a graphic depiction of the sensor probe’s position superimposed on reconstructed 3-D CT images of the patient’s anatomy in coronal, sagittal and axial. The sensor probe and the EWC were successfully steered to the lesion with the guidance of 3-D CT images and the “tip-view” orientation. The closest distance between the sensor probe and the targeted lesion was 1.0 cm (Figure 1B). The video of the registration and navigation of ENB could be available in Figure 2. Once the targeted lesion was reached, the sensor probe and the EWC were observed with the fluoroscopy to insure them in the optimal position. The LG was withdrawn from the EWC. While the EWC was left in situ with a 21-gauge needle (NA-2C-1, Olympus) got through it. Approximately 0.6 mL of methylene blue was then injected at the location through the needle under the guidance of X fluoroscopy (Figure 1C). It took about 14 minutes and 15 seconds to complete the procedure, which was a little shorter than the time reported by Bolton et al. (10). The patient was given an immediate chest CT scan after the injection, which showed that some floccules like cloud occurred above the lesion (Figure 1D). The patient was asked to lie left position and a chest CT scan was carried out to determine the optimal needle path, angle and length. After sterilization of skin around the puncture site and local anesthesia, the hookwire (Breast Localization Needle; Bard Peripheral Vascular, Inc., Reynosa, Tamaulipas, Mexico) was inserted through the chest wall and placed as close as possible to the lesion. The horn of the hookwire was released when the outer cannula needle was withdrawn. A CT scan was performed to confirm that the horn was below the lesion, and to identify that there were no complications, particularly for pneumothorax and hemorrhage. The hookwire extending outside the chest wall was positioned carefully on the skin under gauze dressings. This procedure took about 16 minutes. The patient was then transferred to the operating room within one hour for VATS. The lesion could be seen located in the region between methylene blue and hookwire (Figure 1E). There was no significant diffusion of methylene blue and the thoracic cavity was not contaminated. Thoracoscopic wedge resection of the right lung lobe was performed and it only took 10 minutes of the whole operation. We didn’t have observed any complications of the patient after the operation. The pathological result was adenocarcinoma in situ (Figure 1F). Methylene blue and hookwire did not affect the observation of pathology. The patient recovered well after VATS.
Discussion
With the advent of VATS, thoracotomy is no longer required for the excision of peripheral lung lesions. However, VATS is limited to lesions which can be seen or palpated by the surgeon. Failure to visualize or palpate a lesion can lead to conversion thoracotomy rates of up to 46% according to the report by Suzuki et al. (11). So it is very significant to explore effective preoperative localization method.
The existing literatures suggest that preoperative localization of small nodules can contribute to the surgery. Hookwire localization is commonly used in preoperative localization on account of its simple and feasible feature. The success rate of hookwire localization for small nodules can reach 58% to 97% according to the ACCP guidelines (2). However, the incidence of the complications such as pneumothorax, hemorrhage, pleural reaction is high because of its percutaneous puncture technique. Furthermore, the hookwire had a dislodgement rate ranging from 2.9% to 7.5% in the previous studies (3,4,7), which will lead to the localization failure.
ENB appeared in 2005 as a new diagnosis of peripheral lung lesions technology. For the small peripheral lung lesions, the probe of ENB can reach the fourth order of bronchi or beyond that is unreachable by conventional bronchoscopy (12). ENB system can monitor the distance between the LG and the lesion in real time, which can guide the LG reaching the desired area. Bolton et al. (10) reported that small lung lesions can be positioned with dye marking under the guidance of ENB before VATS, which effectively solved the localization problem of small peripheral lung lesions. Krimsky et al. (7) reported a prospective and multi-center study that the small lesions can be preoperative positioned under the guidance of ENB. The success rate could reach 81% (17 of 21) using indigo carmine dye or methylene blue marking nodules. ENB can reach those bronchi that are unreachable by conventional bronchoscopy through natural orifice, which effectively decreases the incidence of the bleeding and pneumothorax. As was reported by Gex et al. (13), the occurance rate of pneumothorax was about 10 times lower than transthoracic needle biopsy. The dose of methylene blue that we used was very low and can be metabolized quickly. So it didn’t have side effects to the patient. But the technology that located the lesions via the injection of methylene blue under the guidance of ENB has some defects. The diagnostic yield of ENB can reach 79% (30/38) in patients with bronchus sign on the CT imaging, while it only reach 31% (4/13) without bronchus sign in the clinical study of Seijo et al. (14). So the success of the technology was largely dependent on the presence of bronchus sign. ENB is expensive and time-consuming. In addition, methylene blue is water soluble and easy to spread. If the duration time between dye maker placement and operation was too long, it would result in the failure of the localization (7).
Previous studies have pointed out that CT-guided hookwire combined with methylene blue localization has a higher success rate compared with a separate localization of hookwire or dye marking. And the incidence of complications was similar to either technology using alone (15). But the localization accuracy of this approach depended on the accuracy of the puncture needle. Because both the hookwire and injection of methylene blue were performed through the puncture needle. We used ENB guided injection of methylene blue through bronchus, which greatly improved the accuracy of the localization. The lesion of the patient was difficult to localize through percutaneous puncture owing to its small size and the hookwire was easily to dislodge on account of its superficial location. Given the lesion had bronchus leading to, we chose the method to localize the lesion. This was just one example of our exploration. More cases should be expanded in the future to compare the effects of the percutaneous localization, ENB guided localization and combined with these two methods. Our major concern of the modality is that it will not suitable for the lesions that don’t have bronchus signs. We reckon that its advantages outweigh its disadvantages and recommend using this method to localize the lesions in those patients that have bronchi leading to.
Conclusions
This approach provides a more safe and effective method to localize small lung lesions prior to VATS, which can shorten the operation time of VATS and is worthy of further clinical study.
Acknowledgements
Funding: This work was supported by Shanghai Chest Hospital key project (2014YZDC20200), Shanghai Municipal Hospitals’ Rising and Leading Technology Program (SHDC12010101), Scientific Research Program by Science and Technology Commission of Shanghai Municipality (134119a6001) & Shanghai Municipal Health Bureau (20124270).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Begum S, Hansen HJ, Papagiannopoulos K. VATS anatomic lung resections-the European experience. J Thorac Dis 2014;6 Suppl 2:S203-10. [PubMed]
- Gould MK, Donington J, Lynch WR, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e93S-120S.
- Ciriaco P, Negri G, Puglisi A, et al. Video-assisted thoracoscopic surgery for pulmonary nodules: rationale for preoperative computed tomography-guided hookwire localization. Eur J Cardiothorac Surg 2004;25:429-33. [PubMed]
- Chen S, Zhou J, Zhang J, et al. Video-assisted thoracoscopic solitary pulmonary nodule resection after CT-guided hookwire localization: 43 cases report and literature review. Surg Endosc 2011;25:1723-9. [PubMed]
- Liu L, Zhang LJ, Chen B, et al. Novel CT-guided coil localization of peripheral pulmonary nodules prior to video-assisted thoracoscopic surgery: a pilot study. Acta Radiol 2014;55:699-706. [PubMed]
- Andrade RS. Electromagnetic navigation bronchoscopy-guided thoracoscopic wedge resection of small pulmonary nodules. Semin Thorac Cardiovasc Surg 2010;22:262-5. [PubMed]
- Krimsky WS, Minnich DJ, Cattaneo SM, et al. Thoracoscopic detection of occult indeterminate pulmonary nodules using bronchoscopic pleural dye marking. J Community Hosp Intern Med Perspect 2014.4. [PubMed]
- Sun J, Mao X, Xie F, et al. Video of the registration and navigation of ENB. Asvide 2015;2:172. Available online: http://www.asvide.com/articles/750
- Leong S, Ju H, Marshall H, et al. Electromagnetic navigation bronchoscopy: A descriptive analysis. J Thorac Dis 2012;4:173-85. [PubMed]
- Bolton WD, Howe H 3rd, Stephenson JE. The utility of electromagnetic navigational bronchoscopy as a localization tool for robotic resection of small pulmonary nodules. Ann Thorac Surg 2014;98:471-5; discussion 475-6. [PubMed]
- Suzuki K, Nagai K, Yoshida J, et al. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest 1999;115:563-8. [PubMed]
- Mahajan AK, Patel S, Hogarth DK, et al. Electromagnetic navigational bronchoscopy: an effective and safe approach to diagnose peripheral lung lesions unreachable by conventional bronchoscopy in high-risk patients. J Bronchology Interv Pulmonol 2011;18:133-7. [PubMed]
- Gex G, Pralong JA, Combescure C, et al. Diagnostic yield and safety of electromagnetic navigation bronchoscopy for lung nodules: a systematic review and meta-analysis. Respiration 2014;87:165-76. [PubMed]
- Seijo LM, de Torres JP, Lozano MD, et al. Diagnostic yield of electromagnetic navigation bronchoscopy is highly dependent on the presence of a Bronchus sign on CT imaging: results from a prospective study. Chest 2010;138:1316-21. [PubMed]
- Zhan BC, Chen L, Zhu Q, et al. The application of CT guided injection of methylene blue combined with Hookwire in the preoperative localization of thoracoscopic surgery of solitary pulmonary nodule resection. Chin J Clinicians (Electronic Edition) 2011;5:2713-6.


