Minimally invasive thoracic surgery: news from the 3rd Asian-Pacific VATS Performance & the 6th China Lung Cancer MITS Forum
As one of the largest academic feast in Asian-Pacific area, the 3rd Asian-Pacific VATS Performance & the 6th China Lung Cancer Minimally Invasive Thoracic Surgery (MITS) Forum was held in the 1st Affiliated Hospital of Guangzhou Medical University from 12th Oct to 13th Oct, 2012 (Figure 1). The meeting is hosted by Chinese Medical Doctor Association MITS Group, Journal of Thoracic Disease (JTD), State Key Laboratory of Pulmonary Disease and Guangdong Mingyi Medical Charity Fund. More than 420 VATS experts and practitioners had participated in the meeting and discussed about the updated development of MITS in lung cancer.

The annual meeting has gained a great reputation since its first forum in 2006. The 6th forum proposed a new concept of “Rapid Recovery, Accurate Resectomy & Intra-tumor Radiotherapy” in MITS. “It has been 20 years since MITS was born as a new surgery therapy of thoracic diseases”, Prof. Jianxing He, chairman of the meeting said, “Nowadays, we do not just stay in being satisfied with small incision, but focus on maximally reducing physical and psychical trauma. Therefore, we are going to demonstrate a newly full-range MITS called ‘3-Division MITS’ to the world. Besides VATS, we also apply non-intubated anesthesia, from which patients can gain rapid recovery. Some of our patients even could walk and eat on the same day after the surgery. Moreover, the intra-tumor radiotherapy was also considered to be applied during the surgery, which decreases the radiation amount to reduce injury and complications of normal tissue by precisely targeting the tumor.” From October 2011 to October 2012, surgical group of Prof. He has accomplished more than 200 VATS under non-intubated anesthesia, including lobectomy, segmentomy and sleeve lobectomy. Patients had not only gained rapid recovery from less airway trauma but also saved a lot of money by abandoning muscle relaxant.
In order to promote this new concept, 12 VATS surgeries, including 5 non-intubated aneasthisia cases and 1 intra-tumor radiotherapy case were demonstrated in the performance. “The annual meeting always catches the updated techniques of VATS”, said Prof. T. Agathian from Singapore National Cancer Center, “Every VATS expert from Asian-Pacific Area takes participating and performing in the forum as a great honor and a golden opportunity to learn and communicate”.
“This meeting had successfully concluded 20 years’ experience in VATS,” said Prof. Nanshan Zhong, the Academician of Chinese Engineering Academy, “Based on this experience, it also makes a great progress. As a doctor, we should consider all aspects for patients. This concept of 3-D MITS can maximally take down the negative influence of surgery, directing to a better quality of life. That is the ultimate goal of each medical practitioner and patient.”
Since the first national symposium on thoracoscopy on 12nd April 1994, the first affiliated hospital of Guangzhou Medical college have held 1-2 symposium or workshop every year, discussing various minimally invasive techniques. 30 conferences on minimally invasive thoracic surgery have been sponsored or co-organized so far, making great contributions to the development of minimally invasive thoracic surgery in China (Table 1).
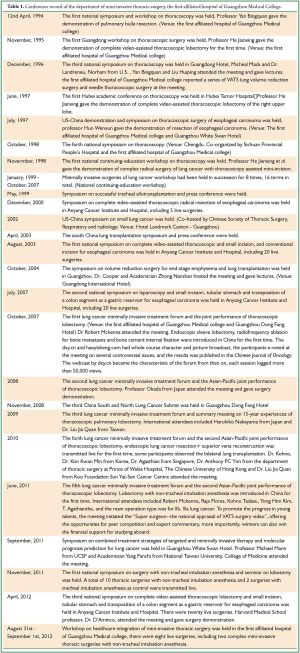
Full table
In this conference, we are honored to have an interview with Prof. Jianxing He.
With a scalpel and a “mirror” in one hand, detector in another, a surgeon can practically get all a patient’s internal bio-information by extracting and examining partly his deep tissue
JTD editor: good morning, Prof. He. Right in the invitation letter, you mentioned that the impediment in how to perform regular lobectomy and dissection of mediastinal lymphoma under C-VATS is taken down technically. This conference is to discuss how to perform difficult thoracic surgery under C-VATS. Which fields do you think entail further exploration and improvement? What is recent progress in these fields?
Prof. He: currently, it is sufficient to have a “mirror” in one hand and scalpel in anther for a thoracic surgeon to operate. It is likely that in the future, a surgeon performs surgery with the “mirror” and scalpel in one hand and samples like tissues or cells are available in another to be examined in order to make a better treatment strategy. As surgeons, we will care more about the bioinformation of our patients, such as the information from cells and tissues, based on the change of which we can treat the disease.
The other concept I want to lay stress on is that local and systemic treatment should be incorporated in a cancer treatment regimen. By local treatment, we intend surgical treatment with a “mirror” and scalpel, while systemic treatment entails the use of agents, such as molecular targeting agents, gene drugs, chemotherapeutic agents, which are closely related to the genetic information of cells. A recent paper in Nature points out that there are 130 chemotherapeutic agents in total, most of which work through genes. By emphasizing efficiency in surgery, we will select agents that are effective with minor side effect so as to reduce the side effect in systemic treatment. Minor side effect may turn out to be major when the treatment is effectual and vice verse. Also, the minor side effect manifests easily when a patient’s immune system is weakened. Patient with cancer should be stratified according to the staging of cancer and given different treatment. That is exactly what we do to patients with lung cancer in our daily practice. Local treatment is preferable in early stage of cancer while systemic treatment in advanced stage.
Ninety percent of our surgeons have to deal with data. We need to collect the bioinformation of our patients, including those related to cancer, drug therapy and the genetic information related to metabolism. With a scalpel and “mirror” in one hand, detector in another, surgeons can get the internal bio-information of their patient by extracting their deep tissue for examination in the future. Nevertheless, it is easier said than done. This technique requires some expertise, as there is great variety in ways of collecting different samples. Some tissues may need to be collected more than once and only after you become well-versed can you do it with more accuracy. “Small but effective sampling”, the very idea of minimally invasive surgery, poses a challenge for all our surgeons.
Non-intubated anesthesia can bring a good effect with little trauma for it can reduce the impairment in physiological function caused by mechanical ventilation, intubation, and muscle relaxants
JTD editor: since the hospital promotes non-intubated anesthesia nationally in 2011, controversies over this method never cease to grow. However, by the end of September 2012, 300 cases of non-anesthesia have been performed nationally. Could you give some comments on the current use of this method? What will be the trend in its future development?
Prof. He: non-anesthesia complies to the idea of rapid recovery. Although regular intubation often works well, which is still practiced on many patients, there is the trend that patients will be stratified and given different anesthesia. First, intubated anesthesia entails the use of muscle relaxants when the trachea remains open, so blood volume needs to be maintained through fluid infusion, which can cause damage to the lung. Second, mechanical ventilation effected by intubation can cause barotrauma and volutrauma. Third, intubation renders tracheal tissue vulnerable to mechanical injury as the front of laryngoscope can be blurred and blind intubation can injure the airway. On the contrary, non-intubated anesthesia can generate a good outcome with little injury for: (I) It reduces the injury to physiological function, produced by mechanical ventilation, intubation, and muscle relaxants. (II) By maintaining the complete defensive function of the respiratory tract, it reduces the chance of pulmonary infection. (III) It also protects the lung from injury produced by mechanical ventilation by encouraging spontaneous respiration. (IV) Bronchospasm was reduced. (V) No side effect brought by muscle relaxants: early postoperative respiration was seen with powerful expectoration. (VI) Occurrence of sore throat and irritable cough due to mechanical injury followed by intubation is reduced. (VII) It enables patients to take food four hours after operation and take general activity early, thus realizing the idea of rapid recovery.
In June 2011, we began to popularize lobectomy under non-intubated anesthesia and up to September this year, 206 cases of lobectomy have been performed, 26 of which are performed under non-intubated anesthesia. Dongguan hospital in Guangdong and hospitals in other provinces follow suit, and it is proven that VATS under non-intubated anesthesia is feasible.
It is a swirl development from standardization to individualization, to standardization of treatment
JTD editor: some doctors think that non-intubated anesthesia is bound to be contentious considering its difficulty in practice. What is your opinion?
Prof. He: it surely takes time to learn, as non-intubated anesthesia is a technique developed slowly. Just like the stratification in patients with cancer, minimally invasive surgery tends towards individualization in its development, not only of incision but of treatment, including surgery, anesthesia, nursing etc. Individualized treatment is a progress based on the previous standardized treatment. However, as local situations vary, so does the development mode. For example, some regions are ill-prepared in terms of technology and physical infrastructure. In this case, these regions reach standardization first before individualization. Under current circumstances without enough knowledge in every aspects, patients must be given standard treatment before receiving individualized treatment according to their stratification. A good collection of individualized practice helps to bring about the new standardization. It is a swirl development from standardization to individualization, to standardization of treatment.
JTD editor: the first national symposium on surgery under non-intubated anesthesia and seminar on lobectomy was held in November last year. Do you anticipate any of such symposiums in the future?
Prof. He: non-intubated anesthesia was one of the themes of this symposium. The topic most widely talked about earlier is minimally invasive lobectomy which is now under the trial of wide use. For the time being, non-intubated anesthesia are rising as a new technique for thoracic surgery. Therefore, symposium as such will and should be held for further study and popularization of the technique.
Minimally invasive internal radiotherapy becomes a landmark in the combination of minimally invasive technique and radiotherapy
JTD editor: minimally invasive internal radiotherapy was brought into the limelight in this year’s symposium. What are the advantages of this technique? How far is it going?
Prof. He: minimally invasive internal radiotherapy nowadays plays a critical role in cancer treatment, considering the limitation of the position and time of traditional radiotherapy for lung cancer. First, it is hard to pinpoint the position of the lung during the respiratory movement. Generally speaking, the focus should be targeted in radiation but this is not necessarily the case. The molds used in many hospitals, which the patients are asked to lie on cannot guarantee that focus is targeted. Second, radiation can cause severe side effect. Though widely used in radiotherapy, the “Gamma knife”, a beam-like procedure in which the radiation comes from a machine that the patient is placed inside, may not penetrate the focus deep enough, resulting in lesions in peripheral tissues. In short, external radiation is a far less direct method compared against surgery.
Minimally invasive internal radiotherapy is born as a landmark in the combination of minimally invasive technique and radiotherapy. Internal radiation is a newer and more pinpointed procedure in which the radiation is implanted in or near the tumor to give it the highest amount of radiation possible, with very little exposure or damage to surrounding tissues. It is a form of radiotherapy in which the source of irradiation is placed close to the tumor or inside a body cavity. In internal radiotherapy, the radioactive source is delivered directly inside the tumor by hollow needles, seeds or wires and may be used alone or with external beam radiation. The radioactive source may be permanently implanted, removed after the required dose or repeated as necessary. Therefore, there is no residual effect of beams, and the position of radiation does not change during respiratory movement. In this sense, it is real-time radiation. As it can work implanted inside the tumor in low dose, it avoids the distant high-energy radiation, transmission and scattering, thus improving the efficiency while reducing the side effect. Moreover, minimally invasive internal radiotherapy correspond to the multidisciplinary development, where surgery, oncology, radiology play a role. The cooperation of so many divisions undoubtedly excels the specialty of one division.
We expect fewer unnecessary resection of normal tissue through precise targeting — the very heard of “minimally invasive”
JTD editor: it has been 20 years since the modern VATS was born. Outstanding experts on VATS from all over the world will assemble in the academic conference to be held in Edinburgh on Nov. 11. Could you please introduce the development of VATS in China?
Prof. He: the history of VATS development can date back to a hundred years ago. It is first found in a medical record from Edinburgh that surgery was done with the help of such video techniques. According the medical record, the operation was performed on Nov. 1, thus the day when the academic conference in Edinburgh is held. It was not until 1994 did the development of VATS begin to take shape as 10 or 20 cases of surgery have been performed in our country, the same time when I started running the workshop. The first workshop was presided over by Prof. Bingquan Yan with the department of urological surgery and department of general surgery as the co-organizer. Our department (the department of thoracic surgery) is responsible for the teaching content, from which we truly understand the idea of minimally invasive and become more convinced of the development of minimally invasive VATS.
In October 1994, the Chinese Journal of Surgery gave a brief introduction on the development of VATS. Articles as such came from several hospitals. Apart from those from our hospital, there are those from the First Hospital of Peking University and other hospitals while our hospital tops others in the number of surgeries undergone.
Minimally invasive thoracic surgery went through 19 years of development from being a treatment for benign lesion to being applied to treat malignant disease, finally to being widely used. The inspiration of curing lung cancer via minimally invasive surgery also came from the lobectomy under C-VATS performed in 1994, which was gradually developed to minimally invasive lobectomy featuring radical video-assisted minithoracotomy (VAMT) and hybrid surgery in 1998. As VATS technique was approved by the Guideline of NCCN in 2005, minimally invasive radical operation for lung cancer again pervaded in 2006 and C-VATS become popular again. After 2009, great progress was made in C-VATS from being a treatment for peripheral lung cancer to central bronchogenic carcinoma, with the technical problem solved.
Currently, segmentectomy is the center of research interest. We believe it is necessary to differentiate the stages of oncology, as well as the condition of patients, and accordingly give them the appropriate surgical treatment as no specific surgical treatment is the panacea. Segmentectomy is the threshold for exact excision. It is our goal for the “minimally invasive” to minimize unnecessary resection of normal intrathoracic tissue by pinpointing the location for surgery with E-BUS, magnetic navigation techniques, and staging of lung cancer.
JTD editor: since the first national symposium and seminar on thoracoscopy in April 1994, 30 conferences on minimally invasive thoracic surgery have been sponsored or co-organized by the affiliated hospital of Guangzhou Medical college so far, making great contributions to the development of minimally invasive thoracic surgery in China. Could you share with us the story along the way?
Prof. He: since the first national symposium and seminar on thoracoscopy was held on April 12, 1994, the first affiliated hospital of Guangzhou Medical College has held 1 to 2 symposiums or workshops every year - discussing various minimally invasive techniques. The first national symposium and seminar on thoracoscopy in 1994 featured lung bullae resection under thoracoscopy demonstrated by Prof. Bingquan Yan in the first affiliated hospital of Guangzhou Medical University. The second national symposium and seminar on thoracoscopy was hosted by Zhejiang People’s Hospital in November 1995, the first conference ever to bring in esophageal surgery under thoracoscopy and many delicate thoracoscopic surgery such as resection of mediastinal tumor, and surgery for patent ductus arteriosus (PDA), surgery for pulmonary hydatid cyst, while our hospital presented lobectomy under thoracoscopy. In December 1996, the third national symposium and seminar was held in Guangdong Haller, which witnessed the participation of Dr Micheal Mack, Dr. Norham Landreneu from USA, signifying the academic communication between China and the world in this field. In this conference, our hospital for the first time reported a set of Lung Volume Reduction Surgery (LVRS) under VATS and mini-laparoscopic surgery. The first three years lay a foundation for the development of thoracoscopic surgery, opening up a prospect for thoracoscopic surgery.
Thereafter, conferences on the progress of technique of general thoracic surgery and thoracoscopic surgery was held on a regular basis, helping us keep up with the latest technical development and get more inspiration. In October 2007, the first symposium on minimally invasive treatment for lung cancer and the joint performance of thoracoscopic lobectomy in Asian-pacific area was successfully held. Dr Robert Mckenna, the internationally renowned expert in thoracic surgery, was invited to the symposium. He owns the publication of most cases of thoracic surgery, about 1,100 cases in total. Endoscopic sleeve lobectomy, radiofrequency ablation for bone metastases and bone cement internal fixation came to publicity in China for the first time, promoted electronically by the dxy.cn. The webcast by dxy.cn became the characteristic of the forum from then on, with the earned rate of each issue exceeding 50,000.
The fifth symposium on minimally invasive treatment for lung cancer and the second Asian-Pacific joint performance of thoracoscopic lobectomy was held in June 2011. In November, the first national symposium on surgery with non-tracheal intubation anesthesia and seminar on lobotomy was held. A total of 10 thoracic surgeries with non-tracheal intubation anesthesia and 2 surgeries with tracheal intubation anesthesia as control were transmitted live. Symposium on combined treatment strategies of targeted and minimally invasive therapy and molecular prognosis prediction for lung cancer was held in Guangzhou White Swan Hotel. Professor Michael Mann from UCSF and Academician Panchi Yang from National Taiwan University, College of Medicine attended the meeting. Then in August 2012, we have workshop on healthcare integration of minimally invasive thoracic surgery, where training of doctor and nurse was incorporated with a view to improve the professionalization of nurse, thus increasing the efficiency while reducing the complications.
In the near future, we appeal for more symposium or conference as such to share the achievement and improve with each other. Together we can promote the technical development of general minimally invasive thoracic surgery.
JTD editor: thank you very much for having this interview with us!
Acknowledgements
We acknowledge DXY.CN’s authorization to publish the interview article.
Disclosure: The author declare no conflict of interest.


