Role of medical thoracoscopy in the treatment of tuberculous pleural effusion
Introduction
Tuberculosis (TB) is a serious health problem in developing countries. In 2013, about 9 million people developed disease in which it had led to 1.5 million people death (1). TB pleurisy, a common manifestation of extra-pulmonary TB (2), accounts for 30–80% of pleural effusions (3). It was considered that delayed hypersensitivity reaction to mycobacterial protein plays an important role in the pathogenesis of tuberculous pleural effusion (TPE) (4). TPE can also be caused by direct spread of subpleural caseous focus in the lung into the pleural space (5) or as a clinic manifestation of reactivation TB (6).
For most of uncomplicated TPE, the recommended therapeutic regimen is as same as the treatment of pulmonary tuberculosis (PTB). Pleural effusion drainage is suggested when patients experience discomfort from dyspnea due to a large effusion and therapeutic thoracentesis or small-bore tube drainage are considered adequate for it. Though residual pleural thickening does not appear to correlate with complete removal of the pleural fluid (7), occurrence is more common if the pleural effusion is initially loculated (8). The development of pleural fibrosis over the visceral pleura separates lung from chest wall, and thus fibrosis develops commonly if the lung could not fully expand (trapped lung) (9). Some studies reported that residual pleural thickening ≥10 mm could cause significant clinical symptoms in patients with TB pleural effusion, with incidences varying from 26.0% to 50.4% (7,10-12). Therefore, it is very important to decrease the incidences and degree of residual pleural thickening, and re-expand the trapped lung as early as possible in clinic.
For loculated TPE, many aggressive approaches, e.g., chest tube drainage, medical thoracoscopy or video-assisted thoracoscopic surgery (VATS), commonly can be used. Some studies suggested that treatment of loculated TPE with drainage and fibrinolytics was effective on the resolution of pleural effusion and decrease the degree of residual pleural thickening (10,11,13). However, this still remains controversial (14,15), and incidences of residual pleural thickening vary from 26.0% to 50.4%. As reported in the British Thoracic Society (BTS), local anaesthetic thoracoscopy was useful for dividing septation and adhesions, thus improving drainage (16). Moreover, high successful rate of medical thoracoscopy on pleural empyema has been reported (17-19). Therefore, studying the role of medical thoracoscopy in the management of an infected pleural disease may provide insights in TB clinic.
In this study, we conducted a retrospective study and analyzed the safety and efficacy of medical thoracoscopy in the treatment of multiloculated and organized TPE.
Study population and methods
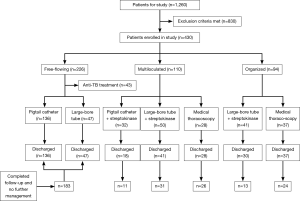
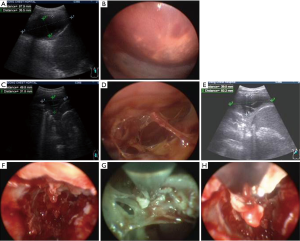
A total of 430 cases with TPE were analyzed from January of 2009 to June of 2014 in the department of TB clinic, Shandong Tuberculosis Control Center, Shandong Chest Hospital, Jinan, China. Ethics approval was obtained from Review Board of Shandong Chest Hospital (Jinan, China). During this period, 1,260 patients were diagnosed with pleural effusion and 430 patients were included in the analysis. All patients were subjected to routine chest radiography, real-time chest ultrasonography and/or thoracic CT in order to determine characteristics of pleural effusion. Among the 430 patients referred with TPE, 43 patients without dyspnea were treated with standard anti-TB treatment, and the other 387 patients underwent ultrasound-guided pigtail catheters, large-bore chest drainage or medical thoracoscopy for diagnosis or therapy. TPE was diagnosed with detection of M. tuberculosis in the pleural fluid, sputum or pleural biopsy specimens, either by microscopy and/or culture, or the histological demonstration of caseating granulomas in the pleura along with or without acid-fast bacilli. Exclusion criteria were: non-TPE; treated with aggressive management (chest tube drainage, medical thoracoscopy, or VATS) before admitted to hospital; lost to follow-up; pleural effusion after pneumonectomy. A total of 430 patients were divided into three different groups primarily based on medical thoracoscopy and/or ultrasonographic examinations: free-flowing effusion presented as anechoic and no or few fibrinous strands (Figure 1A,B); multiloculated effusion presented as fibrinous strands and web-like appearance without fibrous thickening of the pleura (Figure 1C,D); organized effusion presented as intrapleural loculation and fibrous thickening of the pleura (Figure 1E,F).
Chest ultrasound examination was performed and used to determine insertion site by experienced pulmonologists. Pigtail catheters (12F) or large-bore chest tubes (28F) were inserted into the pleural space under local anesthesia. Pigtail catheters were connected to a one-way valve drainage bag and large-bore chest tubes were attached to underwater seal suction with negative pressure suction of 20 cmH2O.
Medical thoracoscopy was performed with the lateral decubitus position under local anesthesia with 2% lidocaine. Insertion site was determined by chest ultrasound examination. A 10-mm trocar was inserted into the appropriate pleural space. A video-thoracoscope (Storz, Wolf, Germany) provided with a 0° optical telescope was used. In the group of multilocula ted effusion, the adhesions or the fibrinous strands between the lung and chest wall were carefully separated (Figure 1G). In the group of organized effusion, the fibrin, the caseous necrosis, the fibrous thickening pleura and other organized components were removed as much as possible (Figure 1H), and in the end of the procedure, the pleural space was rinsed with plenty of saline and a large-bore chest tube was introduced via the insertion site connected to one underwater seal suction with negative pressure suction of 20 cmH2O.
All the patients were treated with the standard anti-TB treatment: four drugs isoniazid, rifampicin, pyrazinamide, and ethambutol for first 2 months, and isoniazid and rifampicin for next 4 months. Pleural drainage or medical thoracoscopy was administered on the patients in the multiloculted and organized groups and those experienced dyspnea due to a large effusion in the free-flowing group once TPE was diagnosed. Among the 226 patients in the free-flowing group, 43 patients without dyspnea were treated with standard anti-TB treatment. Patients with free-flowing effusion and those treated with medical thoracoscopy underwent intrapleural injection with 50 mL saline. Patients with multiloculated and organized effusions those were treated with chest drainage combined intrapleural injection with solutions containing 50 mL saline and 250,000 IU dissolved streptokinase (Aventis, Germany). Intrapleural injection was performed once daily since the following day of pleural drainage for 3 days consecutively. After injection, the tube was clamped for 3 hours before opened for drainage. The pigtail catheter or chest tube was removed when net drainage was <50 mL in the previous 24 hours. After that, the patients were observed for 2 days and discharged.
The successful treatment was defined upon tube duration and time from treatment to discharge days. Success was also defined as improvement in the pleural effusion by image findings (ultrasound examination or chest X-ray) and/or clinical symptoms without requiring further managements. Failure was defined as the persistence or exacerbation of clinical and/or laboratory findings related to pleural loculated effusion or required for insertion of large-bore chest tube, medical thoracoscopy, VATS or open operation.
Data are expressed as mean ± SD (range) or no. (%), and were analysed using one-way ANOVA followed by post hoc test for multiple comparisons among the means of the three groups. Two-tailed Student t-test was used for comparisons of the means between two groups. Categorical variables between groups were examined using the Chi-squared test, as appropriate. P≤0.05 was considered statistically significant.
Results
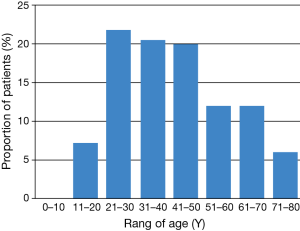
In the study, 1,260 patients were diagnosed with pleural effusion and 430 patients were included in the analysis (Figure 2). Mean of age for 430 patients was 41±16.6 years (range, 15–75 years) and 274 (63.7%) patients were male; the patients with right pleural effusion (54.9%) were slightly higher than those with left side. Patients with TPE tended to be young generation (Figure 3).
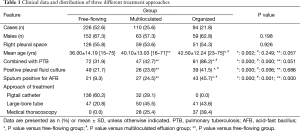
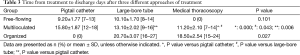
All patients were divided into three groups: free-flowing for 226 patients (52.6%), multiloculated for 110 patients (25.6%) and organized for 94 patients (21.8%). The clinical data and distribution of three different approaches of treatment are shown in Table 1. No differences of sex and right side of pleural space were found among the three groups (P=0.198, P=0.926; respectively). Significant differences were found among the three groups in terms of mean age, combined with PTB, positive pleural fluid culture, and sputum positive for acid-fast bacillus (AFB) (P<0.05). Post hoc comparisons using the LSD test indicated that the mean age of organized group was significantly higher than that of free-flowing group (P=0.002), but there is no difference between organized and multiloculated group, and no difference between multiloculated and free-flowing group either. Incidence of effusion combined with PTB and the rate of positive pleural fluid culture of organized effusion was significantly higher than that of the other two groups respectively, but there was no difference between the free-flowing and multiloculated groups.
Full table
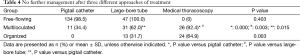
Clinical outcomes of three types of approaches in different groups are summarised in Tables 2,3 and 4. As for the treatment of free-flowing effusion group, there was no significant difference in the tube duration, the time from treatment to discharge days and the rate of no further management between the pigtail catheter and large-bore tube. However, compared with pigtail catheter or large-bore tube, medical thoracoscopy showed significantly shorter time in the drainage and mean duration of hospital stay, also showed higher rate in the no further management during therapeutic and follow-up of multiloculated and organized effusion (P<0.05).

Full table
Full table
Full table
No chronic morbidity and mortality related to complications was observed. Pain was the most complaint, specifically in the cases treated with medical thoracoscopy. Of note, two patients (2/65, 3.1%) treated with medical thoracoscopy had subcutaneously tuberculous abscess at insertion site after 2 months of treatment.
Discussion
TPE, the most frequent form of extrapulmonary TB, is commonly seen in some developing countries (20). Like in the treatment of bacterial empyema, antimicrobial chemotherapy, drainage and expand the trapped lung completely as earlier as possible are also used to treat complicated TPE. Medical thoracoscopy has been introduced to treat TB by repeated adhesiolysis without complications since the first half of the 20th century in Europe (21,22). Most of studies have been focused on the treatment of pleural infection, demonstrating promising results in the clinic (17-19,23). However, few studies were seen in the treatment of TPE. This study has shown that most of multiloculated and organized TPE could be treated safely and successfully with medical thoracoscopy, and ultrasound guided pigtail catheter insertion was considered as the best application in the initial treatment of the patients experienced dyspnea due to a large free-flowing TPE.
In the study, the age distribution of the patients with TPE tended to be younger. Mean of the age (41±16.6 years) and involved gender (63.7% for male) was as same as reported in the earlier study (24). Patients with organized effusion were older than those with free-flowing effusion (P=0.002) and there was no difference between free-flowing effusion and multiloculated effusion. This could be explained as: (I) TPE can be a manifestation of both primary infection and TB reactivation and the latter is the most common disease in developing countries (25). Also, the patients with free-flowing effusion in our study may be mainly primarily infected and this infection usually takes place in young generation; (II) part of organized effusion resulted from direct spread of pulmonary TB, and the patients with parenchymal TB were older than those with pleural effusion caused by primary infection.
Sputum smears were positive in 12% of 84 patients with TB pleuritis (26). In our study, sputum positive for AFB was low in free-flowing effusion group (9.3%) and increasing with the severity of pleural effusion (multiloculated effusion, 24.5%; organized effusion, 45.7%). It has also been reported that mycobacterial culture of pleural fluid had low sensitivity with a range from 12% to 70% (27). This is in line with the data from organized effusion group (41.5%) in our study. Therefore, it is important to obtain sputum test on the diagnosis of patients with suspected TPE.
The guidelines of treating TPE are basically as same as treatment of PTB: four drugs isoniazid, rifampicin, pyrazinamide, and ethambutol for first 2 months, and isoniazid and rifampicin for next 4 months (2HRZE/4HR) (28). Though pleural effusion drainage was performed when patients experienced dyspnea due to a large effusion (29), it was not recommended (7). Some studies have shown that therapeutic thoracentesis and small-bore tube drainage were considered adequate for pleural effusion (7,30). Medical thoracoscopy was used to aspirate the pleural liquid, divide multiple loculations and remove the fibrinous adhesion (31), as well as place the chest tube optimally through a minimal aggressive access (32). Though combination therapy of pleural drainage and fibrinolytics was effective on treatment of loculated TPE, this remains controversial. In our study, patients with multiloculated and organized effusion were treated with medical thoracoscopy showing successful effective treatment, and most of patients needed no further management. Pigtail catheter drainage was good enough for treating the patients with free-flowing TPE. As for the treatment of multiloculated effusion, only 34.4% of patients treated with pigtail catheter drainage and streptokinase irrigation needed no further management. Compared with the pigtail catheter group, medical thoracoscopy and combination therapy of large-bore tube drainage and streptokinase irrigation showed significantly greater improvement in the tube duration, duration of hospital stay and in the number of patients with no further managements. However, large-bore tube and streptokinase irrigation showed poor effect on the treatment of organized effusion and only 31.7% patients needed no further management, which was significantly lower than that of medical thoracoscopy. The results are in accordance with previous studies for the application of medical thoracoscopy on the patients with pleural empyema (17,33).
Compared with VATS and open operation, medical thoracoscopy was considered as an effective approach in the treatment of the patients with multiloculated or organized pleural empyema, especially for those who are under high risk with general anesthesia. However, some studies did not recommend medical thoracoscopy as an alternative to surgical intervention in the presence of loculation (34). In our study, 64.9% patients of organized effusion treated with medical thoracoscopy needed no further intervention. The success was lower than the overall success of 85.4% for the patients with multiloculated and organized thoracic empyema (33). In the treatment of the multiloculated effusion group, 92.4% patients needed no further treatment and that was significantly higher than those treated with large-bore tube and streptokinase irrigation. Therefore, medical thoracoscopy is recommended to the patients with multiloculated pleural effusion as initial treatment as well as to those with organized effusion.
Regarding complications, mortality is 0.35% (16). In our 430 patients, no mortality and chronic morbidity was observed. Pain was the most common complaint and specifically for the patients treated with medical thoracoscopy. Of note, two patients (2/65, 3.1%) treated with medical thoracoscopy had subcutaneously tuberculous abscess at the insertion sites after two months. Interestingly, both abscess occurred at the trocar insertion site that was used as the chest tube position. Tuberculous abscess was not observed when chest tube and trocar insertion sites were not at the same position. However, more clinical data should be collected to identify whether the insertion site of tube could cause subcutaneous infection.
An important limit to the study is that it is not prospective, but we are confident that treatment efficacy is reliable. To date, few studies have been focused on multiloculated and organized TPE. The effectiveness of treatment should be assessed by more outcome measures such as the time required for clinical resolution of fever and dyspnea, pulmonary function test and measurement of residual pleural thickening. Multicenter trials are needed to investigate the role of medical thoracoscopy on organized or multiloculated TPE.
To our knowledge, this is the first retrospective study with a large pool of the enrollment of patients to summarize the application of ultrasound guided pigtail catheter, large-bore tube drainage and medical thoracoscopy with or without streptokinase irrigation in the treatment of TPE. The data demonstrated that ultrasound guided pigtail catheter insertion had played as the best application in the initial treatment on the patients with free-flowing TPE. Medical thoracoscopy can be recommended to treat most of the patients with multiloculated and organized TPE and can minimize the application of VATS or open operation on such patients.
Acknowledgements
J Wang is supported by Special Foundation for Taishan Scholars (tshw201502056) and the Norwegian Centre for International Cooperation in Education (Project no. UTF-2014/10047).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Pai M, Denkinger CM, Kik SV, et al. Gamma interferon release assays for detection of Mycobacterium tuberculosis infection. Clin Microbiol Rev 2014;27:3-20. [PubMed]
- Su SB, Qin SY, Guo XY, et al. Assessment by meta-analysis of interferon-gamma for the diagnosis of tuberculous peritonitis. World J Gastroenterol 2013;19:1645-51. [PubMed]
- Udwadia ZF, Sen T. Pleural tuberculosis: an update. Curr Opin Pulm Med 2010;16:399-406. [PubMed]
- Light RW. Update on tuberculous pleural effusion. Respirology 2010;15:451-8. [PubMed]
- Chakrabarti B, Davies PD. Pleural tuberculosis. Monaldi Arch Chest Dis 2006;65:26-33. [PubMed]
- Antoniskis D, Amin K, Barnes PF. Pleuritis as a manifestation of reactivation tuberculosis. Am J Med 1990;89:447-50. [PubMed]
- Lai YF, Chao TY, Wang YH, et al. Pigtail drainage in the treatment of tuberculous pleural effusions: a randomised study. Thorax 2003;58:149-51. [PubMed]
- Han DH, Song JW, Chung HS, et al. Resolution of residual pleural disease according to time course in tuberculous pleurisy during and after the termination of antituberculosis medication. Chest 2005;128:3240-5. [PubMed]
- Sahn SA. Pleural thickening, trapped lung, and chronic empyema as sequelae of tuberculous pleural effusion: don't sweat the pleural thickening. Int J Tuberc Lung Dis 2002;6:461-4. [PubMed]
- Kwak SM, Park CS, Cho JH, et al. The effects of urokinase instillation therapy via percutaneous transthoracic catheter in loculated tuberculous pleural effusion: a randomized prospective study. Yonsei Med J 2004;45:822-8. [PubMed]
- Cases Viedma E, Lorenzo Dus MJ, González-Molina A, et al. A study of loculated tuberculous pleural effusions treated with intrapleural urokinase. Respir Med 2006;100:2037-42. [PubMed]
- Bolliger CT, de Kock MA. Influence of a fibrothorax on the flow/volume curve. Respiration 1988;54:197-200. [PubMed]
- Chung CL, Chen CH, Yeh CY, et al. Early effective drainage in the treatment of loculated tuberculous pleurisy. Eur Respir J 2008;31:1261-7. [PubMed]
- Maskell NA, Davies CW, Nunn AJ, et al. U.K. Controlled trial of intrapleural streptokinase for pleural infection. N Engl J Med 2005;352:865-74. [PubMed]
- Schiza S, Siafakas NM. Clinical presentation and management of empyema, lung abscess and pleural effusion. Curr Opin Pulm Med 2006;12:205-11. [PubMed]
- Rahman NM, Ali NJ, Brown G, et al. Local anaesthetic thoracoscopy: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii54-60. [PubMed]
- Brutsche MH, Tassi GF, Györik S, et al. Treatment of sonographically stratified multiloculated thoracic empyema by medical thoracoscopy. Chest 2005;128:3303-9. [PubMed]
- Solèr M, Wyser C, Bolliger CT, et al. Treatment of early parapneumonic empyema by "medical" thoracoscopy. Schweiz Med Wochenschr 1997;127:1748-53. [PubMed]
- Colt HG. Thoracoscopy. A prospective study of safety and outcome. Chest 1995;108:324-9. [PubMed]
- Valdés L, Alvarez D, Valle JM, et al. The etiology of pleural effusions in an area with high incidence of tuberculosis. Chest 1996;109:158-62. [PubMed]
- Tschopp JM, Boutin C, Astoul P, et al. Talcage by medical thoracoscopy for primary spontaneous pneumothorax is more cost-effective than drainage: a randomised study. Eur Respir J 2002;20:1003-9. [PubMed]
- Tschopp JM, Brutsche M, Frey JG. Treatment of complicated spontaneous pneumothorax by simple talc pleurodesis under thoracoscopy and local anaesthesia. Thorax 1997;52:329-32. [PubMed]
- Medford AR. Medical thoracoscopy in multiloculated and organised empyema. Respiration 2013;85:87. [PubMed]
- Valdés L, Ferreiro L, Cruz-Ferro E, et al. Recent epidemiological trends in tuberculous pleural effusion in Galicia, Spain. Eur J Intern Med 2012;23:727-32. [PubMed]
- Wiwanitkit V. Medical thoracoscopy for undiagnosed pleural effusions: experience from a tertiary care hospital in North India. Indian J Chest Dis Allied Sci 2011;53:192-author reply 192. [PubMed]
- Conde MB, Loivos AC, Rezende VM, et al. Yield of sputum induction in the diagnosis of pleural tuberculosis. Am J Respir Crit Care Med 2003;167:723-5. [PubMed]
- Gopi A, Madhavan SM, Sharma SK, et al. Diagnosis and treatment of tuberculous pleural effusion in 2006. Chest 2007;131:880-9. [PubMed]
- González-Martín J, García-García JM, Anibarro L, et al. Consensus document on the diagnosis, treatment and prevention of tuberculosis. Arch Bronconeumol 2010;46:255-74. [PubMed]
- Wyser C, Walzl G, Smedema JP, et al. Corticosteroids in the treatment of tuberculous pleurisy. A double-blind, placebo-controlled, randomized study. Chest 1996;110:333-8. [PubMed]
- Cartaxo AM, Vargas FS, Salge JM, et al. Improvements in the 6-min walk test and spirometry following thoracentesis for symptomatic pleural effusions. Chest 2011;139:1424-9. [PubMed]
- Kern L, Robert J, Brutsche M. Management of parapneumonic effusion and empyema: medical thoracoscopy and surgical approach. Respiration 2011;82:193-6. [PubMed]
- Light RW. Parapneumonic effusions and empyema. Proc Am Thorac Soc 2006;3:75-80. [PubMed]
- Ravaglia C, Gurioli C, Tomassetti S, et al. Is medical thoracoscopy efficient in the management of multiloculated and organized thoracic empyema?. Respiration 2012;84:219-24. [PubMed]
- Tassi GF, Davies RJ, Noppen M. Advanced techniques in medical thoracoscopy. Eur Respir J 2006;28:1051-9. [PubMed]