Air leakage on the postoperative day: powerful factor of postoperative recurrence after thoracoscopic bullectomy
Introduction
A primary spontaneous pneumothorax (PSP) is a common condition; its prevalence is 24 per 100,000 in men and 9.8 per 100,000 in women (1). A common cause of a PSP is the presence of subpleural bleb or bulla; usually located at the apex (2). Pleural drainage is the first treatment for the first episode of PSP. However, recurrence rate is high because of pathologic change of the visceral pleura. Bullectomy is the most effective treatment modality that can decrease the risk of recurrence. Since 1990s, video-assisted thoracoscopic surgery (VATS) has been widely used and it became a standard treatment choice for PSP; however, the outcome of VATS remains unsatisfactory (3), due to its relatively high recurrence rate. The primary mechanism of recurrence is considered the formation of new bulla near the staple line (4). Various surgical techniques have been employed to decrease the risk of recurrence; they include parietal pleurectomy, mechanical abrasion, chemical pleurodesis, and reinforcing the staple line with synthetic materials (5). However, the efficacy of an additional pleural procedure is controversial. Most important skill is the obliteration of the bulla in VATS bullectomy. Theoretically, air leakage after bullectomy is not common and the advancement of surgical instrument also helped to reduce postoperative air leakage, especially for the simple wedge resection using endo staplers. This study is performed based on the hypothesis that immediate postoperative air leakage may be associated with postoperative recurrence. We reviewed the medical records of the patients with VATS bullectomy and identified risk factors.
Methods
This was a retrospective review that was approved by the Institutional Review Board at Seoul St. Mary’s Hospital (Republic of Korea). Written informed consent was obtained from all the patients. From January 2011 through March 2013, 232 patients underwent surgical management of a pneumothorax. The patients who underwent 3-port VATS bullectomy for PSP with same technique were reviewed. The patients with a secondary pneumothorax, open thoracotomy were excluded and the patients with different technique including pleurectomy, mechanical abrasion, or single port surgery were excluded. A total of 147 patients underwent 3-port VATS bullectomy for PSP, and their medical records were reviewed.
Surgical technique
Preoperatively, high resolution computed tomography (HRCT) was performed. Operative indications were: (I) recurrent pneumothorax; (II) previous history of contralateral pneumothorax; (III) hemopneumothorax; (IV) bilateral pneumothorax; (V) prolonged air leakage (>4 days); (VI) visible bullae (>5 mm in diameter) on HRCT despite being the first episode of PSP.
Under general anesthesia, a double lumen endotracheal tube was placed. After selective lung ventilation, the standard 3 ports were used for the procedure. A 10.5 mm port was placed in the 7th intercostal space at the mid-axillary line for a 10 mm thoracoscope. Another 5 and 12 mm ports were inserted at the anterior and posterior axillary line. Lung inflation with or without under waterseal was performed to identify the bulla. Bullectomy was performed including the visible bulla and surrounding normal lung tissue. The staple line was covered with a polyglycolic acid (PGA) NEOVEIL sheet (Gunze, Ayabe, Japan) and fibrin glue. Pleural abrasion or pleurectomy was not performed. A single chest tube was placed in the thorax. The chest tube was removed when air leakage ceased and the drainage was less than 150 mL per day. The specimen was fixed in formalin and measured.
Statistical analysis
All statistical analyses were conducted using SPSS version 18 (SPSS Inc., Chicago, USA). Patient medical records were reviewed and a telephone survey of the patients was conducted regarding postoperative recurrence. The definition of a recurrence was based on chest X-ray finding and included minimal collapse of the lung, compared with the previous examination, regardless of symptoms. Data was presented as the median (minimum-maximum) or frequencies and percentages, as appropriate. Logistic regression analysis was used to identify the predictors for postoperative recurrence. Multivariate analysis was performed using univariate variables; P<0.05 was considered to be statistically significant.
Results
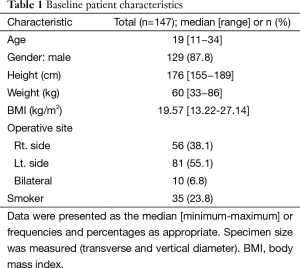
This study reviewed 147 patients who underwent 3-port VATS bullectomy; the baseline characteristics of the patients are presented in Table 1. The median age was 19 years (range, 11−34 years). Males predominated: 129 (87.8%). The median height and weight was 176 cm (range, 155−189 cm) and 60 kg (range, 33−86 kg). The median body mass index (BMI) was 19.57 kg/m2. Ipsilateral apical bullectomy was performed on 137 patients (right:left =56:81). A bilateral bullectomy was performed on ten patients (6.8%). Among these patients, bilateral pneumothorax occurred in three patients and the others had a history of a previous contralateral pneumothorax. Thirty five patients were current smoker.
Full table
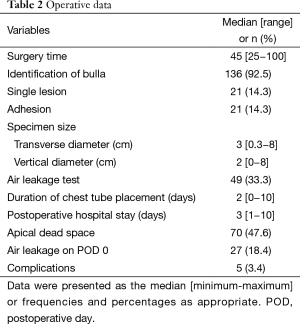
The operative data and postoperative outcomes were demonstrated in Table 2. The median operative time was 45 mins (range, 25−100 mins). The bulla was identified in the 136 patients (92.5%) during operations. For 11 patients, bulla was not found during the operation and apical stapling was performed to the patients. A total of 21 patients (14.3%) had a single bulla, the others had multiple bulla. Mild pleural adhesion was noted in the 14.3% of patients. A total of 49 patients were underwent air leakage test under water seal after bullectomy by the surgeon’s preference.
Full table
The specimen was fixed in the formalin and the size was measured. The median transverse and vertical diameter was 3 and 2 cm. A total of 70 patients (47.6%) showed apical dead space on the immediate postoperative chest X-ray. A total of 27 patients (18.4%) showed air leakage on the postoperative day.
The median postoperative duration of chest tube drainage was 2 days; the median postoperative hospital stay was 3 days.
Complications were developed in five patients.
Among them, one patient had lung injury during the port placement due to the presence of adhesions, and required primary repair.
One other patient, had hemopneumothorax, required a transfusion due to hemorrhage.
Prolonged air leakage (>5 days) occurred in one patient. This patient was discharged on postoperative day 10; however, recurrent PSP was noted a month later and the patient underwent a repeat procedure. There was no ruptured bulla at the first operation for this patient but for the second operation, small sized ruptured bleb was identified. The lesion was removed and the patient was discharged on postoperative day 3.
Lung injury during double stapling was another complication for one patient and a primary repair was performed.
One patient, discharged without complications on postoperative day 3, complained chest pain and purulent sputum 2 weeks after discharged day; Right upper lobe pneumonia was found through a chest X-ray, and the patient underwent antibiotic treatment.
Median follow-up period was 39 months (range, 21−53 months). Postoperative recurrence was developed in the 24 patients (16.3%; median disease free interval: 12 months). Reoperation was conducted in seven patients and closed thoracostomy in eight patients. The others showed minimal pneumothorax and are recovered without treatment. In the patients with minimal recurrent pneumothorax, nine patients had no symptoms. However, apical visceral pleural line was minimally collapsed on the routine follow-up chest X-ray. They were categorized as recurrence group.
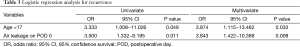
With univariate analysis, gender, height, weight, BMI and smoker were not risk factors for recurrence. Single lesion versus multiple lesion, pleural adhesion, specimen size, air leakage test after bullectomy and apical dead space were not risk factors for recurrence. Younger age less than 17 years and immediate postoperative air leakage were significant risk factors for postoperative recurrence by univariate and multivariate analysis (Table 3).
Full table
Discussion
A VATS bullectomy for PSP has become popular worldwide. It results in a shorter hospital stay, less postoperative pain, and less postoperative respiratory dysfunction (6,7). However, one meta-analysis revealed that the incidence of postoperative recurrence after VATS bullectomy was 4 times higher than that of an open procedure among similar cases (3). According to the historical studies, the recurrence rate has been reported to range from 10% to 24.5% (4,8,9). The main cause of postoperative recurrence is new bulla formation near the staple line; therefore, various techniques have been introduced to avoid postoperative recurrence in PSP. Apical pleural abrasion and/or a pleurectomy were classical additional procedures performed after a bullectomy. These procedures create a pleural symphysis between the visceral pleura and parietal pleura. However, they may result in severe postoperative pain, bleeding, disturbance of normal pleural physiology, and an obstacle to future thoracic surgery (5,10). Furthermore, the efficacy of additional procedures is controversy. A prospective randomized trial showed that there was no difference between staple line coverage and mechanical pleurodesis in postoperative recurrence (11). A covering procedure of the staple line is less invasive than a pleural abrasion or a pleurectomy (12) so there is no universally accepted surgical procedure for PSP. In our hospital, coverage technique is the routine procedure in VATS bullectomy.
Gaunt et al. found that 30% of patients had postoperative apical dead space, which was associated with postoperative recurrence (13). In our experience, many patients (47.6%) have an apical dead space on the postoperative chest X-ray, and this apical dead space is found to have been obliterated several months postoperatively. Apical dead space may be associated with the resected lung volume. Tsuboshima et al. demonstrated new bulla formation was associated with resected lung weight (14). However, bulla does not always locate at the apex. Although the specimen was fixed in the formalin, the specimen cannot always be measured. The specimen size and weight was different according to the degree of the lung collapse at the time of surgery so apical dead space and specimen size was not reliable variable. In our study, these variables were not significant risk factors.
Some risk factors for postoperative recurrence were known in PSP including younger age, and prolonged air leakage (15,16). However, most important surgical skill is complete resection of bulla because single bulla is not common in PSP. In our study, only 14.3% of patients had single lesion and recurrence free interval was too short (median: 12 months). Are we sure all of bulla could be resected?
We hypothesized that remaining apical lung tissue is capable of expansion. It can result in emphysematous changes, tension on the staple line. If tiny bleb or bulla is missed, overlooked small bleb or bulla may rupture following postoperative lung hyperinflation or become sizable bulla on the staple line.
In our study, immediate postoperative air leakage was a significant risk factor for recurrence. The cause of postoperative air leakage may be due to lung injury during manipulation or overlooked small bulla or new bulla around staple line. However, lung injury rarely occurs during thoracoscopic bullectomy in PSP. During operation, 49 patients underwent air leakage test after bullectomy under water seal and there was no air leakage during operation. However, eight patients (recurrence in four patients) showed post-operative air leakage (16.3%). Air leakage test under thoracoscopy may be unreliable for detection of air leakage (17). We cautiously speculated that it might be incomplete resection of unlooked bleb or bulla as a cause of postoperative recurrence of PSP.
This study was a retrospective analysis with a short duration of follow-up period, therefore it has limited outcome. The recurrence rate is relative high but recurrence is determined only imaging studies with or without symptoms.
Conclusions
The pathogenesis of postoperative recurrence may be complex. However, immediate postoperative air leakage is common in VATS bullectomy and associated with postoperative recurrence. Immediate post-operative air leakage increases the risk of recurrence; further study will be required whether air leakage is associated with postoperative recurrence.
Acknowledgements
This manuscript has been edited by native English-speaking experts of BioMed Proofreading.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Melton LJ 3rd, Hepper NG, Offord KP. Incidence of spontaneous pneumothorax in Olmsted County, Minnesota: 1950 to 1974. Am Rev Respir Dis 1979;120:1379-82. [PubMed]
- MacDuff A, Arnold A, Harvey J, et al. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii18-31. [PubMed]
- Barker A, Maratos EC, Edmonds L, et al. Recurrence rates of video-assisted thoracoscopic versus open surgery in the prevention of recurrent pneumothoraces: a systematic review of randomised and non-randomised trials. Lancet 2007;370:329-35. [PubMed]
- Muramatsu T, Ohmori K, Shimamura M, et al. Staple line reinforcement with fleece-coated fibrin glue (TachoComb) after thoracoscopic bullectomy for the treatment of spontaneous pneumothorax. Surg Today 2007;37:745-9. [PubMed]
- Muramatsu T, Nishii T, Takeshita S, et al. Preventing recurrence of spontaneous pneumothorax after thoracoscopic surgery: a review of recent results. Surg Today 2010;40:696-9. [PubMed]
- Waller DA, Forty J, Morritt GN. Video-assisted thoracoscopic surgery versus thoracotomy for spontaneous pneumothorax. Ann Thorac Surg 1994;58:372-6; discussion 376-7. [PubMed]
- Freixinet JL, Canalís E, Juliá G, et al. Axillary thoracotomy versus videothoracoscopy for the treatment of primary spontaneous pneumothorax. Ann Thorac Surg 2004;78:417-20. [PubMed]
- Horio H, Nomori H, Fuyuno G, et al. Limited axillary thoracotomy vs video-assisted thoracoscopic surgery for spontaneous pneumothorax. Surg Endosc 1998;12:1155-8. [PubMed]
- Nakanishi K. An apical symphysial technique using a wide absorbable mesh placed on the apex for primary spontaneous pneumothorax. Surg Endosc 2009;23:2515-21. [PubMed]
- Leo F, Pastorino U, Goldstraw P. Pleurectomy in primary pneumothorax: is extensive pleurectomy necessary? J Cardiovasc Surg (Torino) 2000;41:633-6. [PubMed]
- Lee S, Kim HR, Cho S, et al. Staple line coverage after bullectomy for primary spontaneous pneumothorax: a randomized trial. Ann Thorac Surg 2014;98:2005-11. [PubMed]
- Cho S, Ryu KM, Jheon S, et al. Additional mechanical pleurodesis after thoracoscopic wedge resection and covering procedure for primary spontaneous pneumothorax. Surg Endosc 2009;23:986-90. [PubMed]
- Gaunt A, Martin-Ucar AE, Beggs L, et al. Residual apical space following surgery for pneumothorax increases the risk of recurrence. Eur J Cardiothorac Surg 2008;34:169-73. [PubMed]
- Tsuboshima K, Nagata M, Wakahara T, et al. Relationship between postoperative bulla neogenesis at the staple line and the resected lung volume in primary spontaneous pneumothorax. Gen Thorac Cardiovasc Surg 2015;63:572-5. [PubMed]
- Imperatori A, Rotolo N, Spagnoletti M, et al. Risk factors for postoperative recurrence of spontaneous pneumothorax treated by video-assisted thoracoscopic surgery†. Interact Cardiovasc Thorac Surg 2015;20:647-51; discussion 651-2. [PubMed]
- Noh D, Lee S, Haam SJ, et al. Recurrence of primary spontaneous pneumothorax in young adults and children. Interact Cardiovasc Thorac Surg 2015;21:195-9. [PubMed]
- Uramoto H, Tanaka F. Natural air leak test without submergence for spontaneous pneumothorax. J Cardiothorac Surg 2011;6:165. [PubMed]


