From 200 BC to 2015 AD: an integration of robotic surgery and Ayurveda/Yoga
Introduction
India has a very rich history of traditional medicines. The various branches of medicine that have been around for centuries include Ayurveda & Yoga, Unani, Siddha and Homeopathy (AYUSH). Among these Ayurveda, Yoga and Siddha are medical systems, which follow the Panchamahabhoota siddhanta, or theory of the five mahabhootas (basic functional elements), which represents ‘mass’, ‘attraction’, ‘heat’, ‘movement’ and ‘space’ of every “thing” in the universe. These medical sciences explain ‘life’ as the structured interactions of these elements, within a defined system, guided by ‘Consciousness’ or ‘Atman’ (1). Among the traditional systems of medicine practiced all over the world, Ayurveda and Yoga has a documented history dating back to 1500 BCE (2,3). Ayurveda deals with the art of surgery and had developed it as a specialty named Salyatantra. Sushruta, considered as the father of plastic surgery (4), was a very famous Salyatantra expert whose treatise on Ayurveda, the “Sushruta Samhita” provides a surgical perspective to patient care. Sushruta Samhita is propounded to have had its first edition in BCE 1000. It is the first written document explaining care of a surgical patient, specialized surgical instruments, caustics, cautery, blood-letting, plastic reconstruction, management of fractures and dislocations, surgical management of vesical calculus, fistula-in-ano, intestinal obstruction, intestinal perforations, ascites, surgical management of malposition and death of fetus, wounds and ulcers, and deep-seated abscesses (5).
Indian patients readily accept this treatment methodology, as these practices are socially prevalent since long and culturally relevant to the Indian psyche. To promote development of education and focused research in these specialties, The Indian government established a ministry of AYUSH in March 1995.
Integrative medicine is one of the ways to provide safe, efficient, cost effective and patient centric health care (6). It is broadly defined as the process of bringing different systems of medicine together to offer best modalities of prevention, cure, care, and management in healthcare (7). In short, integrative medicine combines alternative medical practices with evidence based allopathic medicine. It is also called as integrated medicine or integrative health in United Kingdom. Proponents claim that it focuses on the ‘whole’ patient (mind, body and spirit) rather than treating disease and emphasizes a patient-physician relationship.
However, modern biomedicine practitioners are very skeptical of these traditional medical practices. There is a general sense of disbelief among the biomedicine physician regarding therapeutic benefits and safety of these systems. It is not helped by the exaggerated and unscientific claims made by some certified traditionalists and innumerable quacks, who lay claim to such traditional medical knowledge by virtue of their ‘place of birth’, ‘genetic lineage’ and often enough ‘divine intervention’.
We set out to share our experience of the therapeutic benefits of combining cutting edge 21st century technologies like robotic thoracic surgery and age-old medicines like Yoga and Ayurveda.
The combination has synergistic benefits for the patient. They provide a holistic approach to medical care of very sick patients undergoing ultra-major surgeries for a variety of diseases like cancer, tuberculosis and aspergilloma to name a few.
Methods
Four hundred and fifty-eight consecutive patients undergoing major thoracic surgery between June 2013 and December 2015 were included in the study population.
The diagnosis of these patients included tuberculosis empyema, pyogenic empyema, lung cancer, aspergilloma, bronchiectasis, giant bulla, thymic hyperplasia associated with myasthenia gravis, thymoma, bronchogenic cyst, lymphangioma, pericardial cyst, pneumothorax secondary to bullae, diaphragmatic eventration, thoracic outlet tumours, neurogenic tumours (schwannoma, neuroganglioma).
All patients were reviewed in the surgical outpatient clinics with a detailed interview and discussion of risks and benefits of surgical therapy. Routine blood investigations, echocardiograms, electrocardiography, pulmonary function tests were performed. Pre-anesthetic evaluation was performed for fitness for surgery following the European guidelines for fitness for thoracic surgery (8).
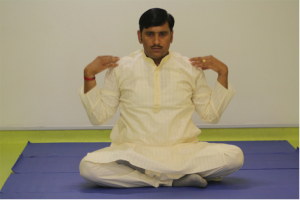
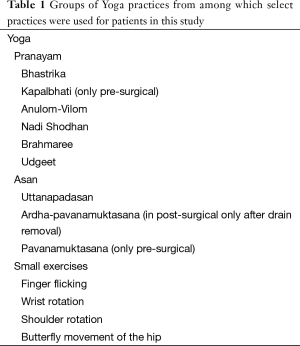
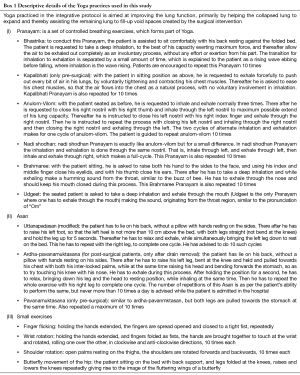
In general, all patients undergoing minimally invasive thoracic surgery (video assisted or robotic) were referred to the Integrative Medicine Department for integrative addition of Yoga. Yoga exercises were taught to the patient in the pre-operative clinic. These included practices such as Pranayam (breathing exercises) Anulom Vilom, Asans (physical postures), and Sookshma Vyayam (small exercises involving the wrist, shoulder and feet) (9) (Figures 1-4) (Table 1) (Box 1). Patients were given a free choice to opt out of the program if they so desired.
Full table
Full table
There were three criteria followed to choose the suitable Yoga procedures for a patient, which were based on the (I) patients’ surgical status (pre-/post-operative); (II) type of surgery; and (III) severity of the clinical condition, generally assessed based on the physical location of the patient, within the hospital. Thus in general the Yoga interventions provided could be classified as (I) pre-surgical Yoga, which was after admission and before surgery and (II) post-surgical Yoga, which were administered at different locations in the hospital, at post-surgical recovery, ICU, and in-patient ward, and out-side the hospital as post-discharge advise. Yoga procedures administered to a patient were tailor-made for individual patients but from a selection of Yoga techniques (Table 1), considering the above criteria.
Surgical techniques
Patient underwent major thoracic surgery intervention by using minimally invasive techniques. Advanced video assisted thoracic surgery (VATS) technique using three ports or single port was employed for 262 patients. The remaining 192 patients were operated using the three ports robotic surgery technique. This involved using a four arm Da Vinci robot (Intuitive Surgical HD Si).
The surgery included resection of mediastinal tumours and cysts, lobectomy, segmentectomy, sleeve resection, bullectomy and pleurectomy, diaphragmatic plication, metastasectomy, drainage of empyema, decortication, drainage of pleural effusion and pleurodesis.
A single drain was inserted into the chest to drain the pleural fluid, blood and air. Drains were connected to Medela Thopaz digital suction device (Medela Healthcare, Switzerland).
Postoperative care
No epidural catheters were inserted. Pain control was achieved by using one or more appropriate combination of extrapleural catheter, thoracic intercostal block, patient controlled analgesia, use of buprenorphine or fentanyl transdermal patch and oral analgesia.
Post-surgery, the patients were referred for integrative medicine review soon after surgery in the post-surgical recovery ward for early chest wall mobilization and lung capacitation, through Pranayam based Yoga procedures.
The Yoga integrative medicine physician and Yoga therapist visited the patient within 6 hours of surgery in the postoperative room or the intensive care unit. Patients were reassured about the outcomes of the surgery. The patients were encouraged to perform specific Yoga (Pranayam, and Sookshma Vyayam), as trained pre-surgically, under the guidance of the Yoga expert and were mobilized out of bed to encourage chest physiotherapy and endobronchial toilet. They were encouraged to perform deep breathing Yoga and to expectorate the phlegm. An incentive spirometer was used to encourage the patient and give him a visual feedback. Patients performed incentive spirometry once every hour. A specialist pain team was also involved to control pain and administer appropriate pain medications. Standard dose of oral medication was tablet paracetamol 1 g 4 hourly and tablet tramadol 500 mg three times a day. If pain was still persistent then a transdermal buprenorphine patch (5 µg/hour) was applied.
A routine postoperative chest X-ray was performed to ensure appropriate drain placement and ensure absence of pneumothorax before starting Yoga therapy.
Next morning the surgical team reassessed the patient. A Yoga session of Pranayam (Bhastrika, Anulom-Vilom and Nadi Shodhan) was given prior to chest drain removal. If there was no air leak and lung expansion was confirmed on chest X-ray the drain was removed. We were very liberal with amount of fluid drained. Drainage up to 400–500 mL was tolerated. No patient needed reinsertion of drain.
Yoga was administered with progressive intensity of breathing and physical mobilization, through the post-surgical admission, and continued daily and regularly until discharge.
Pranayam exercises were performed to help the lungs expand slowly and steadily rather than induce sudden forceful expansion. This is to prevent any internal injury, bleeding and breaking of any stitches of surgery. The focus was on slow, sustained inhalation and forceful exhalation, and involuntary filling up of the lungs by naturally mediated inhalation.
Only select few Yoga interventions were included in the protocol considering patient safety and compliance. Very few patients were taught Kapalbhati, a Pranayam, and it was administered only pre-surgically, in order to improve the abdominal muscles and chest wall movements. Kapalbhati, was not administered for 90 days post-surgically, as post-surgical patients invariably had thoracic drains and Kapalbhati could cause severe pain and even possible internal tissue injury.
Pain scores were tabulated. Patient was mobilised into the ward corridors. Patient was then taken outdoors to a roof top garden growing medicinal plants used in Ayurveda, accompanied by the Yoga therapist. The garden has a collection of aromatic and medicinal plants such as ocimum sanctum, vitex negundo, ricinus communis, withania somnifera, asparagus racemosus, tinospora cordifolia, rauvolfia serpentina, adhatoda vasica, rosa chinensis, hibiscus rosa-sinensis, cymbopogon citratus, cynodon dactylon, phyllanthus amarus, vernonia cinerea, bacopa monnieri, mentha piperita, piper longum etc, many of which are used as fresh herbs in the Integrative treatment program offered by the hospital (Figure 5).
In most cases, patients were discharged home the next day with a detailed plan outlining the Yoga exercises, which they were expected to continue for life (all Pranayams, while excluding Kapalbhati for 3 months). Patients were reviewed in the postoperative clinic at 10 days and 6 weeks when a pain score was maintained. Postoperative pulmonary function test was performed to document recovery of pulmonary function. A patient satisfaction questionnaire was also documented. If patients were not satisfied with therapy, they were offered the option to drop out of the therapy program.
Post-discharge the patients were advised to continue with the Yoga procedure on a regular basis at home. Less than 5% of the patient’s complaint of port site pain. If the pain is still persistent at 6 weeks follow-up, they were referred to integrative medicine department for ayurvedic management.
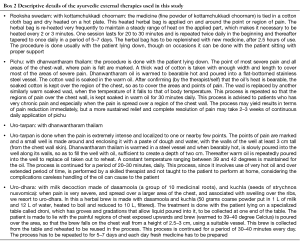
Patients approaching the Integrative Medicine Department for the post-thoracotomy pain were administered ayurvedic therapies called “Uro-tarpan” (retaining warm medicated oil on specific area of chest for a specified period of time) (Figures 6,7) and “Patra potali” (patra means medicated leaves and potali refers to a cloth bag where these special leaves are processed and bound-in. These potalis were warmed by immersing them in hot medicated oil, and thereafter used to give hot-fomentation over the affected body part) (Figures 8,9) (10).


The criteria for deciding the ayurvedic treatments were dependent on the clinical symptoms of pain, oedema and healing status of the surgical wound. Patients were classified as (I) those with pain and non-healed surgical wound, with or without oedema; and (II) those with pain of long standing nature (often radiating and spread over the chest wall) with fully healed surgical wounds. The ayurvedic therapies such as rookshaswedam, pichu, uro-tarpan and uro-dhara were administered over the areas of pain especially covering the chest-wall, abdomen and upper limbs (Table 2) (Box 2).

Full table
Full table
The external therapies, especially oil based/or herbal brew based therapies were performed only after the surgical wounds were completely healed. In case of patients who were referred with post thoracotomy pain but with an open wound, we use the rookshaswedam, taking great precautions as not to have any contact with the wound or contaminate it in any manner.
The temperature of the herbal bags and oil is one thing to be extremely cautious about. During our training of the patient/patient relative, we instruct the person performing the treatment to check the warmth of the herbal bag and oil on the dorsum of his/her hand before applying it on the chest or around the loci of pain. Even in self-administration, this is essential and point of caution, as the patient might have altered sensation to heat/pain/touch in the affected region of the chest.
Internal medicines of ayurvedic origin were used very rarely, and when used they were assured to be of 100% herbal origin, with good safety record, and manufactured by reputed and licensed pharmaceutical companies. Most commonly used internal medicines were shaddharanam gulika (a tablet) for improving metabolism, in patients with oedema and triphala choornam (a powder) for management of constipation.
We looked at a variety of outcomes to assess patient compliance and benefits. In case of compliance to Yoga therapy, we looked for complaints about pain, tiredness, inability to perform, lethargy and breathlessness while or immediately after Yoga therapy, or mental unacceptability to the procedure of Yoga. Benefits of Yoga were also assessed by noting several parameters such as the number of hours the patients spend in the post-surgical recovery ward, the quantum of fluid drained from the thoracic drain at defined time intervals, number of days within which patients were mobilized or were bed-ridden, number of days it takes for the patient to generate enough air-pressure to raise all the three balls in the spirometer during inhalation and exhalation and the number of days the patient is discharged from the hospital. The post-surgical events and complications if any are also noted, to assess the long term benefits to the patients.
In case of external therapies for post-thoracotomy pain, compliance was assessed from costing, ease of acceptance and regularity of performing the procedure. The benefit in terms of pain (localized/radiating), localized edema, general and upper limb mobility and upper trunk flexibility were also noted to assess long-term outcome benefits.
Results
We compared results with patients who underwent minimally invasive thoracic surgery before our integrative medicine program started.
We have documented that our pain scores have improved. Patients are using less pain medications at lower doses.
The Yoga group has less drainage (185±35 mL) as compared to previous group (230±35 mL) (P= ns).
Chest X-ray review suggested less atelectasis in the Yoga group as compared to previous group. There were three episodes of chest infection in the Yoga group requiring antibiotics for 5 days. No readmission in this group. Previously we had 15 episodes of chest infection requiring antibiotics. Of these three patients needed readmission.
The ability to move shoulder and arms was good in these patients. No shoulder stiffness or frozen shoulder was reported. Three patients in the control group complained of shoulder and chest wall stiffness and required physiotherapy.
All patients were discharged early (mean hospital stay 2.1±1.2 days) as compared to 2.8±1.6 days previously (P= ns).
Patient satisfaction scores were very high (8–9/10, mean 9.1). Unfortunately we do not have satisfaction data from previous group. The patients and their family reported a high level of comfort with the Yoga therapist and integrative physician.
Early intervention of port site pain led to a break in the cycle of chronic pain. The soothing effect of the hot fomentation and massage therapy seems to have helped patients overcome the pain (19/20 patients). One patient did not benefit from the uro-tarpan was subsequently referred to the chronic pain clinic for local ablation therapy.
Discussion
A Yoga session costs 10 USD and a pain management session costs 20 USD. Each patient attended an average of six sitting of Yoga and three sittings of pain management therapy. By Indian economic standards these amounts are not exorbitant. The benefit of an integrated practice is not dependent on the immediate cost alone, but on the cost-benefit analysis. Considering the benefit for the patient in terms of early recovery, reduced complications and overcoming of thoracotomy pain, we feel that the integrative practice is cost effective. In addition, we taught the patient and a relative, tailor-made treatment procedure in one or two sittings and encouraged them to video graph the whole procedure administered by an expert to keep as a reference point. They were also given the names of the medicines in a printed prescription, and whenever plausible, address of medical shops which might stock the medicines near their locality of residence. Patients are very happy with the Yoga interventions and the compliance is more than 95%. In case of the pain management intervention there is more than 75% compliance, 2/20 patients remarked that the procedure was cumbersome and time consuming, as it required repeated hospital visit for therapy sessions. These were patients with low intensity pain.
“Holistic” rather than disease specific therapy maybe the way forward. Multitude of therapeutic options is available to the modern physician. It is important that we do not scorn the past and reject it.
Yoga, Meditations and Ayurveda have been around for centuries and have found their way into day-to-day life. Increasing number of people around the world are accepting these techniques for better living and wellness. If these techniques can help wellness then there is nothing to suggest that they will not help the patient who is undergoing a major life changing surgery.
At our centre, an open and honest communication between the various specialities helped us to set up the integrative medicine program. Our Integrative Medicine Department holds equivalent status as other clinical specialities like cardiothoracic and neurosurgery. We are presenting papers at each other’s conferences. The Yoga therapist and integrative medicine physician have recently presented papers at the Indian Association of Cardiothoracic Surgeons Annual Meeting. By the same token, our robotic surgeons have given talks and presentations at World Ayurveda Conference and World Yoga Day. We have been well received at both these platforms.
The Indian Ministry of AYUSH is in consultation with us to implement similar programs at other hospitals.
At our institute, integrative medicine is now in collaboration with other specialities including oncology, radiotherapy, urology, neurology, endocrinology, and cardiology.
Psychologically the Indian patients are very comfortable with Yoga, Meditation and Ayurveda as this is in line with their innate religious beliefs.
Our protocols are designed such that these exercises can be done at home. They do not mandate a return to hospital. The program has led to a change in lifestyle for these patients who are making “wellness” a part of their daily routine.
In Charaka Samhita, the sage physician of Ayurveda, Charaka illuminates “The Science of Life shall never attain finality. Therefore, humility and relentless industry should characterize your endeavour and approach to knowledge. The entire world consists of teachers for the wise. Therefore, knowledge, conducive to health, longevity, fame and excellence, coming even from an unfamiliar source, should be received, assimilated and utilized with earnestness” (11).
We do believe that it would be a folly to ignore our heritage and ancient sciences. In order to fully live in the present, it is important to learn from the past to plan a better future.
Acknowledgements
The authors would like to thank Vijaypal Sharma (Diploma Panchakarma), and Dinesh Yadav [B.Sc (Yoga), Department of Integrative Medicine, Medanta The Medicity, Gurgaon, India].
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Consents: I write to confirm that we have communicated with the people in the pictures and they have given written permission to use their pictures for publication.
References
- Dwarakanath C. The Fundamental Principles of Ayurveda. Varanasi: Krishnadas Academy, 1952.
- Snyderman R, Weil AT. Integrative medicine: bringing medicine back to its roots. Arch Intern Med 2002;162:395-7. [PubMed]
- Govindaraj P, Nizamuddin S, Sharath A, et al. Genome-wide analysis correlates Ayurveda Prakriti. Sci Rep 2015;5:15786. [PubMed]
- Champaneria MC, Workman AD, Gupta SC. Sushruta: father of plastic surgery. Ann Plast Surg 2014;73:2-7. [PubMed]
- Valiathan MS. The Legacy of Susruta. Chennai: Orient Longman, 2007.
- Pillai GK, Sharma P. Finding a sustainable prototype for integrative medicine. J Ayurveda Integr Med 2014;5:134-8. [PubMed]
- Horrigan B, Lewis S, Abrams D, et al. Integrative Medicine in America: How Integrative Medicine Is Being Practiced in Clinical Centers Across the United States. Minneapolis: The Bravewell Collaborative, 2012.
- Brunelli A, Charloux A, Bolliger CT, et al. ERS/ESTS clinical guidelines on fitness for radical therapy in lung cancer patients (surgery and chemo-radiotherapy). Eur Respir J 2009;34:17-41. [PubMed]
- Singh V, Wisniewski A, Britton J, et al. Effect of yoga breathing exercises (pranayama) on airway reactivity in subjects with asthma. Lancet 1990;335:1381-3. [PubMed]
- Lavekar GS, Menon TV, Bharti. A Practical Handbook of Panchakarma Procedures. New Delhi: Central Council for Research in Ayurveda and Siddha, Department of AYUSH, Ministry of Health and Family Welfare, Government of India, 2009.
- Shankar D. Conceptual framework for new models of integrative medicine. J Ayurveda Integr Med 2010;1:3-5. [PubMed]