Glasses-free three-dimensional endoscopic bronchoplasty, arterioplasty, and angioplasty of the superior vena cava for the radical treatment of right middle upper lung cancer
Case presentation
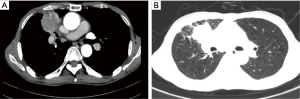
A 63-year-old male patient was admitted due to the confirmed squamous cell carcinoma of right upper lung for over 3 months. The patient was admitted to our hospital three months ago, during which percutaneous lung puncture biopsy indicated the presence of moderately-differentiated squamous cell carcinoma in the right upper lung. The patient was then received two cycles of chemotherapy including albumin-bound paclitaxel (355 mg) + carboplatin (400 mg). A second chest CT showed a soft-tissue mass sized 4.0 cm × 4.3 cm in the anterior segment of right upper lung and right middle lung (Figure 1). Most of the lesion was located in the right middle lung, with visible spiculation in its edge and pleural retraction. Contrast-enhanced scan shoed that lesion was not heterogeneously enhanced, along with the stenosis and occlusion of right middle lobe bronchus and the decrease of volume of the right middle lobe; in addition, the anterior segmental bronchus of right upper lobe also showed stenosis and partial occlusion.
Routine blood test and liver/kidney function tests, heart and lung function tests, and whole-body PET-CT showed no evidence of functional abnormality of each organ or cancer metastasis. Lung function test showed that FVC was 75% and FEV1 was 75%. The patient was explained about the disease condition and the need for surgery, and he agreed to receive a surgery. Therefore, we performed endoscopic bronchoplasty, arterioplasty, and angioplasty of the superior vena cava under general anesthesia with double lumen tube.
Surgical maneuvers
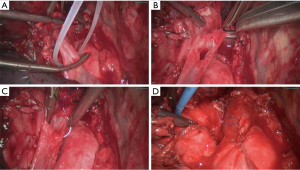
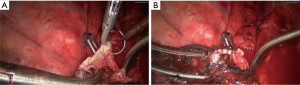
Intraoperative exploration showed that the mass was located at the center of right upper lobe and had protruded into the right main bronchus; it surrounded the interlobar portion of right lung artery and invaded part of the lateral wall of superior vena cava. Also, it had invaded the phrenic nerve. Pleural indentation was also observed. The mass was hard and sized about 7 cm × 6.5 cm. A number of swollen lymph nodes sized 1 cm × 1 cm or 1.3 cm × 1.5 cm were detected in pulmonary hilum and mediastinum. Extensive pleural adhesions were seen, while no pleural effusion was detected. After consulting with Dr. Jianxing He and his team, we decided to perform right middle upper lobectomy in combination with bronchoplasty, arterioplasty, and angioplasty of the superior vena cava.
This surgery is featured by the reconstruction of three major vessels/bronchus—superior vena cava, right pulmonary artery, and right bronchus.
- Open the pericardium to dissociate the superior vena cava. After blocking with non-invasive vascular forceps, we resected part of the superior vena cava, followed by the continuous anastomosis using Prolene sutures (Figure 2);
- Cut open the right oblique fissure to separate the intermediate trunk of right lung artery; after it was blocked using non-invasive vascular forceps, we resected the right middle upper lung. The right lung artery was continuously sutured, and then the forceps were released and the exhaust pipe was tied (Figure 3);
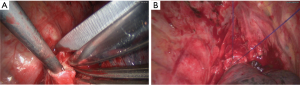
- Continuous suture of right main bronchus and right middle bronchus (Figure 4);
- Surgical incisions (Figure 5).
Results
The surgery lasted 175 min, among which the time consumed for angioplasty of the superior vena cava, arterioplasty, and bronchoplasty were 30 min, 22 min, and 30 min. The intraoperative blood loss was about 120 mL. Totally 5 lymph node stations (23 lymph nodes) were intraoperatively dissected, and metastasis to one lymph node was seen in station 4. Intraoperatvie frozen-section analysis showed that the upper and lower margins of the bronchus were negative. The postoperative recovery was good, and the patient was discharged on day 8. The detail of the operation was demonstrated in the video (Figure 6).
Discussion
The past two decades have witnessed the rapid developed of video-assisted thoracoscopic surgery (VATS) techniques, and VATS has been widely applied in the treatment of thoracic diseases such as lung cancer (2). VATS has been recongized by the US National Comprehensive Cancer Network (NCCN). During the lung cancer surgeries, bronchial sleeve pneumonectomy can avoid total pneumonectomy when removing tumors, and therefore it can lower the surgery-associated mortality and improve the long-term survival by maximizing the preservation of lung function. Thus, it has become a standard procedure for central-type lung cancer. Many studies have confirmed the safety and feasibility of VATS bronchial sleeve resection in the treatment of central-type lung cancer. Compared with conventional open chest surgery, VATS has comparable safety and postoperative survival rate, along with smaller trauma, shorter hospital stay, and faster recovery (3-7).We initially had carried out Hybrid VATS sleeve pneumonectomy (3,4); in recent years, we further performed complete VATS sleeve pneumonectomy (5), carinal resection and reconstruction (5), and resection and reconstruction of superior vena cava (8). In our current case, the tumor had invaded the right pulmonary trunk, superior vena cava, and right upper bronchus; during the surgery, we completely resected the tumor and achieved reconstruction. The triple reconstruction procedures were performed by the continuous suture technique using Prolene sutures.In our surgery, glasses-free three-dimensional (3D) endoscopic system was applied, which effectively reduced the operator’s sense of discomfort and poor lighting; meanwhile, it effectively improved the operator’s sense of space and reduced the time required for space conversions. Thus, the operation goes in a more natural and smooths way and thus effectively reduces the surgical risks.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Shao W, Yin W, He J, et al. Endoscopic bronchoplasty, arterioplasty, and angioplasty of the superior vena cava. Asvide 2016;3:158. Available online: http://www.asvide.com/articles/913
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [Crossref] [PubMed]
- Shao WL, Liu LX, He JX, et al. Bronchial sleeve resection and reconstruction of pulmonary artery by video-assisted thoracic small incision surgery for central lung cancer: a report of 139 cases. Zhonghua Wai Ke Za Zhi 2007;45:1530-2. [PubMed]
- He J, Shao W, Cao C, et al. Long-term outcome of hybrid surgical approach of video-assisted minithoracotomy sleeve lobectomy for non-small-cell lung cancer. Surg Endosc 2011;25:2509-15. [Crossref] [PubMed]
- Xu X, Chen H, Yin W, et al. Thoracoscopic half carina resection and bronchial sleeve resection for central lung cancer. Surg Innov 2014;21:481-6. [Crossref] [PubMed]
- Rendina EA, De Giacomo T, Venuta F, et al. Lung conservation techniques: bronchial sleeve resection and reconstruction of the pulmonary artery. Semin Surg Oncol 2000;18:165-72. [Crossref] [PubMed]
- Ettinger DS, Bepler G, Bueno R, et al. Non-small cell lung cancer clinical practice guidelines in oncology. J Natl Compr Canc Netw 2006;4:548-82. [PubMed]
- Xu X, Chen H, Yin W, et al. Initial experience of thoracoscopic lobectomy with partial removal of the superior vena cava for lung cancers. Eur J Cardiothorac Surg 2015;47:e8-12. [Crossref] [PubMed]