Uniportal video-assisted thoracoscopic bronchoplastic and carinal sleeve procedures
The thoracoscopic approach for major pulmonary resection has numerous advantages compared to open techniques (1-4) without sacrificing the oncologic principles of thoracic surgery. In fact, there is evidence that video-assisted thoracoscopic surgery (VATS) lobectomy may even offer reduced rates of complications and even better survival rates for early stage tumors (5). Future studies will be needed as well to determine if there are advantages for thoracoscopic sleeve resections when comparing with open surgery.
The sleeve procedures offer benefits of parenchymal preservation and oncologic safety even for patients who can tolerate more extensive resections (6). However sleeve resections are technically more demanding than pneumonectomy and are more prone to particular complications (7).
Sleeve procedures are contraindicated when local extension of the tumor requires pneumonectomy as it occurs with involvement of interlobar fissure. The surgeon must identify and avoid reconstructive techniques with risk to develop a severe complication. If the bronchial reconstruction is likely to fail because of the excessive tension or poor anastomotic technique, the result should be carefully evaluated at the end of the procedure, leading to an extensive resection in case of doubt.
Thanks to the recent improvements in thoracoscopy, advanced cases and sleeve resections can be performed without performing thoracotomies (8). During the last years, experience gained through VATS techniques, design improvements of the surgical instruments and improvements of high definition cameras have greatly contributed to advances in VATS (9). Because its approach is less invasive, the uniportal approach for VATS has emerged as a novel technique, applicable to all large spectrum of pulmonary resections including sleeve reconstructions.
In this article we describe the technique of thoracoscopic sleeve procedures through a single incision approach for bronchial, bronchovascular and carinal resection.
Preoperative planning
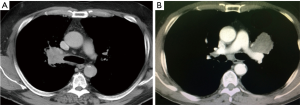
The indication for a sleeve resection is usually made preoperatively based on computed tomography scan (CT), Positron emission tomography—computed tomography scan (PET-CT) and bronchoscopy (Figure 1). Mediastinoscopy or endobronchial ultrasound biopsy (EBUS) should be performed prior to the operation in the case of uptake on PET-CT. The extension of the tumor should be carefully ascertained and histology should be confirmed with biopsy. Preoperative bronchoscopy can identify the need for a sleeve lobectomy when the tumor is at the entrance of a lobar bronchus, or when there are exophytic tumors in a main-stem bronchus or when submucosal signs indicate cancer extension. This diagnostic information is helpful at the time of the surgery when the bronchus is incised and divided. Suitability for surgery should also be assessed, and a pulmonary function test and a perfusion scan performed to predict postoperative lung function are relevant when planning a sleeve.
Typical carcinoid tumors are the ideal cases for sleeve resections. They frequently have a limited base of invasion of the bronchus and the margins do not need to be too large.
During the postoperative management, the patients are usually given antibiotics, humidification or mucolytic and physiotherapy. A bronchoscopy should be performed to check the integrity of the suture and to clear secretions before patient is discharged home.
Surgical thoracoscopic technique
Most of the authors use 3 incisions for the VATS sleeve procedures but the surgery can be performed by using only one (10,11). The patient is positioned in a lateral decubitus position. We consider very important the proper placement of the incision, especially when it is performed by uniportal VATS. Performing the incision at the fourth or fifth intercostal space, more anterior (anterior axillary line), helps to use the needle holder parallel to the hilum, making suturing similar to an open anterior thoracotomy. Using a wound protector is helpful because fatty tissue could interfere with the suture threads (Figure 2).

The operating table’s position makes the lung exposure easier to perform the anastomosis (the anterior rotation of the table 45º to the surgeon places the lung on an anterior position and makes easier the posterior bronchial suture, especially the membranous portion).
Our preferred method for suturing is to use a continuous absorbable suture (Polydioxanone, PDS 3/0) which makes the thread movement easier, as well as the tying or a novel absorbable barbed suture device, the V-Loc™ wound closure device (Covidien, USA), which avoids knot-tying and keeps strength and security (13). We always test the anastomosis under saline water and we only place one chest tube at the end of the operation.
When performing bronchial suturing using uniportal VATS, it’s very important to maintain the camera on the posterior part of the incision, operating with both hands below the camera. Here we apply the same principle as when performing an anterior thoracotomy in open surgery. That is to have a direct view with the surgeon’s eyes above his/her hands (Figure 3). The geometrical explanations of the approach (14) are important factors to facilitate the sleeve reconstructions through a single incision approach. As a result, the anastomosis can be accomplished from a straight perspective in our opinion (Figure 2).
We can classify 3 types of bronchoplastic procedures according to the resection type:
- Simple bronchoplasty. It is the easiest bronchoplastic procedure. When the tumor is located at the bronchial base, the bronchus is incised at its origin using a long scalpel. For the closure, we use a single PDS 3-0 suture (flushed shape) (Figure 4);
- Wedge bronchoplasty. In this case the bronchial incision is made deeper in a wedge shape to the main bronchus. This kind of incision may call for a transverse closure, but if the wedge is large and doesn’t allow approximation, it may be reconstructed using a lateral closure. The closure stitches are made without tension, and with approximation to the mucosa using a monofilament absorbable interrupted or continuous suture. Recent studies have shown that wedge bronchoplasties, when possible, are a good oncological equivalent to sleeve bronchoplasties, enabling better preservation of the bronchial vascular supply. This is suitable for small tumors with limited invasion of the bronchus, and it allows surgeons with limited experience performing VATS bronchial sleeves to accomplish an oncologic and safe resection (16);
- Sleeve bronchoplasty. The bronchial sleeve resections with an end to end anastomosis are the most complex bronchoplastic procedures. The right upper lobe (RUL) bronchoplasty is normally the most frequently performed and less difficult procedure, due to the alignment of the main and the intermediate bronchi. However, the right bronchus is located at the rear side of the pulmonary artery, and occasionally it is too hidden by the pulmonary artery or the azygos vein which increases the difficulty of the anastomosis (Figure 1). The liberation of the pulmonary ligament facilitates lung mobility and reduces tension during and after the anastomosis. For RUL sleeves, the subcarinal lymph node dissection should be performed at the beginning of the procedure. However, the paratracheal lymphadenectomy is preferably done last, after the anastomosis, to prevent the proximal bronchi from retracting under the azygos vein into the paratracheal space, which makes subsequent suturing difficult and requires division of the azygos vein.
The bronchus may be incised initially using a long scalpel, and then the bronchial circumference section may be completed using scissors. Our preferred method is to perform the entire anastomosis using a running suture in two steps. Usually, the first step is to suture the posterior bronchus wall and then the second step is to suture the anterior wall from behind (inside out) so that both edges are tied at the front level. Another option is a combined technique: interrupted stitches for the cartilage portion of the anastomosis and a continuous suture for the membranous portion. It is best to tie each interrupted stitch before placing the next interrupted stitch to avoid having the free ends of the suture touch each other and get tangled. It is also preferable to tie the knot outwards.
The most complex sleeve procedures are usually those of the left side, due to the presence of the aortic arch and the larger size of the PA. For left-sided bronchial resections, it’s best to use a right-sided double-lumen tube in order to make the suturing easier and reduce to the tension on the bronchus.
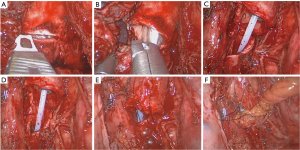
Right upper lobe (RUL) sleeve lobectomy (Figure 5)

Clinical case: 55-year-old male. Squamous cell carcinoma located on the main right bronchus. The patient received 3 cycles of chemotherapy with good response. The incision, 4–5 cm long, was performed on the 4th intercostal space (more convenient for anastomosis on the right side). After division of the vessels and opening the fissure, the right main bronchus, upper lobe bronchus and intermediate bronchus were dissected and sectioned using a long scalpel or scissors (18). The margins were inspected macroscopically and a frozen section was performed before starting the anastomosis. The azygos vein was transected with endostaplers. Sutures were placed on the edge of the main and intermedius bronchus and the bronchial anastomosis was initiated by using a continuous monofilament absorbable 3/0 suture (PDS or V-loc). To compensate the difference of caliber between both bronchi, the interval between the sutures of main bronchus was slightly larger than the intermedius and was adjusted during continuous suture (19).
Left upper lobe (LUL) sleeve resection (Figure 6)

The absence of intermediate bronchus, the interference with aortic arch and main PA and the short length of upper lobe bronchus, makes the anastomosis more difficult than on the right side. Care must be taken to avoid injury of the left laryngeal nerve when dissection and anastomosis involves the main bronchus or when complete lymph node dissection of station 5 is performed.
Division of the bronchus occurs just proximal and distal to the base of the LUL. Division of the distal end is potentially hazardous because the base of the superior segmental bronchus is next to the LUL’s base, and care must be taken not to injure this structure.
The subcarinal lymph node dissection should be performed before the bronchial division. The main bronchus and lower lobe bronchus are initially incised with a long scalpel and then with scissors. The anastomosis is performed as previously described. The running suture technique is performed in two steps: every 180 degree of the 360 degree of the bronchus circumference.
Left lower sleeve anastomosis
The left lower sleeve lobectomy is technically more complex because of the presence of the pulmonary artery (which should be retracted), the atrium and upper lobe vein. The orientation to perform the anastomosis is also more difficult because the upper lobe bronchus needs to be re-implanted on the main bronchus from an anterior view position, and once we incise the main bronchus is deeply located (10).
The left upper lobe (LUL) bronchus is dissected and exposed. The mainstem and the upper lobe bronchi are cut circumferentially with a knife on a long handle and scissors (Figure 7). We commence an end-to-end anastomosis with the first suture in the cartilaginous-membranous junction to help appose the upper lobe bronchi and mainstem bronchi, and then proceeded with a running suture in the posterior wall of airway (the most difficult part of anastomosis). Once the posterior wall of the anastomosis is completed, a running anterior suture is then performed and both sutures are tied with the help of a thoracoscopic knot-pusher.
Bronchial sleeve resection (sparing lung) (Figure 8)
Bronchoplastic resections with preservation of parenchyma should be attempted whenever possible when treating distal tracheal or centrally located endobronchial tumors rather than performing a lobectomy, especially for young patients or with poor pulmonary function (22). Generally, the main indications for this surgical technique without lung resection include bronchial low malignant tumors and some benign diseases (23).
VATS lung sparing bronchial sleeve resection is a technically more complex procedure than a standard VATS sleeve lobectomy.
The bronchial anastomosis after a VATS sleeve lobectomy is less difficult to perform as exposure for suturing of the two bronchial ends is easier after removal the lobe (24). The overlying undivided lobar structures limit the exposure for mobilization and sewing during sparing lung sleeve procedures. Compared to the right bronchial sleeve resection, the thoracoscopic reconstruction of the second carina on the left side is usually more complex because the anastomosis of upper and lower lobe bronchus and the left main bronchus is often hidden in the rear of the left pulmonary artery (24).
Clinical case: a 34-year-old young women with an endobronchial carcinoid located on the intermedius bronchus. The main and the RUL bronchus were dissected and exposed. The subcarinal and peribronchial lymph nodes were removed to better expose the anatomy. Once the fissure was divided, the basal artery for lower lobe was taped and retracted. The bronchus intermedius was incised distally above the origin of the right middle bronchus and proximally just below the origin of the RUL bronchus (Figure 9). The anastomosis was commenced by suturing the posterior wall of the bronchus from anterior to posterior direction by using a 3/0 PDS suture. Another continuous suture was done to complete the anterior wall of the anastomosis and both sutures were tied together. The integrity of the anastomosis was tested under saline water. The postoperative recovery of the patient was uneventful and the patient was discharged home on the third postoperative day.
Bronchial sleeve and vascular reconstruction (Figure 10)

When the tumor invades the pulmonary artery sometimes it’s necessary to resect part of the artery (26,27) or, occasionally a total sleeve (28). The dissection and control of the PA is recommended from the beginning (sometimes intrapericardial control is needed). Before the PA clamping, 5,000 UI intravenous heparin must be administered to prevent thrombosis. We can perform the proximal pulmonary artery clamping with a thoracoscopic clamp. For distal clamping it’s better to use bulldog clamps on the artery or clamping the inferior pulmonary vein to interfere as less as possible with the instruments (28). Occasionally, a double vessel loop is enough to clamp the distal artery for partial resections.
When vascular reconstruction is necessary it is advisable that it is done during the last step of the lobectomy (first divide the veins, bronchus and fissure) in order to have a larger surgical field and more control of the section of the pulmonary artery.
The indications for sleeve resection of the pulmonary artery are mostly upper lobe tumors where the tumor or malignant lymph nodes affect the main PA or the upper lobe branches (Figure 1B).
A partial resection of the pulmonary artery can be performed especially when the tumor invades the base of one of the lobar branches but without a large involvement (less than 1/3 circumference) into the main PA. After heparinization and clamping of the main artery and distal trunk a tangential incision on the pulmonary artery is performed and a direct closure by means of a running suture with prolene 5/0 or with several interrupted sutures.
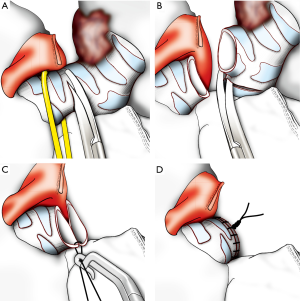
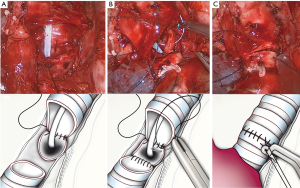
In case of vascular sleeve, the bronchial anastomosis should be performed first in order to avoid traction to the vascular suture (Figure 11A). The end-to-end vascular anastomosis can be performed with a running monofilament suture (prolene 5/0) in two steps: the first suture line must be the posterior wall of the anastomosis from a back to front direction (Figure 11B). Another running suture is used to complete the anastomosis of the anterior wall and it is then tied to the first suture.

Once the vascular suture is completed the distal clamp is removed to release any air thanks to the return flow and tied once the artery is filled. Then a progressive release of the proximal clamp is done.
Carinal resection
Tumors invading the distal trachea or carina represent a challenge due to the complexity of airway reconstruction and management through a thoracoscopic approach (29). The surgical approach for distal trachea or carinal resections should by the right side (30). A total coordination with the anesthesiologist is paramount during airway resection and a plan in case of emergency should be carefully stablished preoperatively.
To perform this procedure through uniportal VATS, there are two options in order to maintain lung ventilation: the use of an intra-surgical field tracheal tube (31) or through high frequency jet ventilation (32). In the first option a sterile circuit is passed onto the field and prepared to directly ventilate a single lung. For high frequency ventilation jet, the catheter can be introduced through the endotracheal tube and thanks to the small diameter of the catheter for ventilation; it doesn’t interfere with the anastomosis of the membranous portion (Figure 12). This way we do not need intra-field intubation. Both strategies require a perfect communication with the anesthetics team.
The mode of airway reconstruction depends greatly on the extent of resection. For limited resections of the carina, the right and left mainstem bronchi can be reapproximated to form a ‘‘neocarina,’’ which is then attached to the distal trachea. When a right upper lobectomy is necessary with carinal resection, a careful reimplantation of the bronchus intermedius or right lower lobe bronchus to the trachea or left mainstem should be performed to avoid airway necrosis and narrowing. To avoid anastomotic angulation, devascularization, or excesive tension, it is recommended to perform maneuvers for hilar release before the anastomosis. The azygos vein can be transected by using vascular clips (click aV, GrenaR, UK) or endostaplers.
To avoid the aspiration of blood into the left main bronchus, carinal resection should be performed without removing the double-lumen tube. This maneuver allows a safe incision and resection of the distal trachea, right main and left main bronchus. The use of high-frequency jet ventilation of the left lung is useful to maintain oxygenation and facilitates the anastomosis of the left side wall of the main stem bronchus and distal trachea, avoiding the insertion of a tracheal tube through the incision (33).
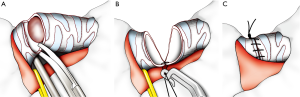
The suture should be commenced first suturing the left side wall of the trachea and left main bronchus (Figure 12A). Then sutured membranous trachea and left main bronchus. Then neo-carina of left main bronchus and right main (in case of pure carinal resection) or intermediate bronchus (in case or RUL and carinal) (Figure 12B). Finally the right side wall of the trachea, left main bronchus and right bronchus should be anastomosed (33) (Figure 12C). It is recommended to cover the suture with a pericardial flap.
Another option is the resection of the carina, followed by a total end-to-end anastomosis between the left main bronchus and the trachea with an anastomosis of the right main bronchus to the lateral, cartilaginous wall of the trachea (at least 2 cm above the first anastomosis).
When carinal reconstruction can not ensure a tension-free anastomosis, the safest option is to perform a carinal pneumonectomy (if patient tolerate the procedure) by doing an end-to-end anastomosis of the trachea to the remaining mainstem bronchus (Figure 13). The suture should be commenced first suturing the left side wall of the trachea to the left side wall of the left main bronchus, then membranous portion and finally right side of trachea and left main bronchus.
We have analyzed our experience with double sleeve and carinal resections in conjunction with the Tyumen Regional Oncological Center (Russian Federation). To date we have performed 10 cases (8 male, 2 female) with a mean age of 61±4.6 years (range, 48–68 years): 7 uniportal VATS double-sleeve resections (6 left upper lobectomy, 1 RUL) and 3 uniportal carinal resections (2 RUL and 1 sleeve pneumonectomy). Three cases of uniportal double-sleeve lobectomy and one case of uniportal carinal resection received neoadjuvant chemotherapy (gemcitabine + cisplatinum). The mean operative time was 260±20 min (range, 240–330 min) and the mean intraoperative blood loss of 235.5±55.6 mL (range, 50–460 mL). The mean number of lymph nodes resected was 13.12±5.13 (range, 12–20). The mean postoperative hospital stay was 10±1 days (range, 7–20 days). Two cases of double-sleeve lobectomy developed postoperative pneumonia but were succesfully treated with intravenous antibiotics. There was no postoperative 60-day mortality in this serie of patients.
Discussion and literature review
Minimally invasive surgery for cancer has proven to offer many benefits over traditional open surgery, including less pain and faster recovery without compromising oncologic results (1-5). VATS has evolved from the conventional three-port technique to the uniportal approach during the last decade (34).
Thanks to the increasing experience with thoracoscopic suturing, tying techniques and development of new instruments, the bronchoplastic procedures can be performed thoracoscopically by expert surgeons (33,35,36). There are many publications showing that an open sleeve lobectomy results in a better survival rate than pneumonectomy, a reduced loss in lung function, and an improved operative mortality (37,38). The first description of a VATS sleeve procedure was published 15 years ago by conventional VATS (39). The concerns about performing an oncologic resection and a safe anastomosis when bronchoplasty is needed are the main reasons for the slow adoption of the technique. This limits the number of surgeons that are able to master the sleeve technique by VATS. Some authors consider a minimum number of 25 cases for overcoming the learning curve and safely perform locally advanced cases by VATS (40).
Like all other procedures, VATS sleeve lobectomy has its natural learning curve. According to our own experience, at least more than 200 VATS lobectomies and at least 20 cases of open sleeve procedures should be done in order to lay the anatomical and operative technique foundation, before you can perform a thoracoscopic sleeve resection (41).
The principles of the VATS bronchoplasty are the same as for open surgery (37). The anastomosis must be performed free of tension for mucosa to mucosa approximation. We recommend using monofilament absorbable sutures for smooth placement and sliding of knots (non-absorbable sutures can irritate the airway and cause significant postoperative cough). A critical technical issue is the management of the sutures to avoid the tangling of the untied ends. The management of the instruments and sutures is more crucial in VATS than in an open thoracotomy. The tension of the suture can be carefully adjusted with a sliding knot-pushing instrument.
Some authors recommend interrupted sutures to allow better size matching, less anastomotic site ischemia and prevent the loosening and entanglement of the sutures (42).
Other authors improved the suturing technique by using both continuous and interrupted suturing, for the membranous and cartilaginous portions of the bronchus respectively (43). In our particular experience a continuous suture performed in two steps for the posterior and the anterior bronchial wall results in less suture tangling and is quicker (33,35). A novel absorbable barbed suture device, the V-Loc™ wound closure device can be used to avoid knot-tying (13).
We routinely do not buttress the suture unless the case was after radiation or presented with signs of infection (44). In these cases we can use an intercostal muscle flap, pedicle pericardial or mediastinal fat pad.
There are few articles published in the literature describing bronchial, vascular or combined bronchovascular sleeve by VATS, and most of these resections are reported by using conventional thoracoscopic techniques (45,46). As our experience has grown with the uniportal VATS approach we have increased the rate of these reconstruction techniques and decreased the incidence of pneumonectomy (27-29,33,34). In a recent publication, we assessed the feasibility of uniportal VATS approach in the treatment of advanced NSCLC and compared the perioperative outcomes with early-stage tumors with good postoperative results (47).
There are several case reports of NSCLC sleeve procedures of the RUL by using 4 ports (48), 3 ports (49,50) or 2 ports (51). Mahtabifard et al. reported a series of 13 sleeve resections. Median operative time was 167 min (range, 90–300 min) and chest tube duration was 3 days (range, 2–6 days). Morbidity was 31% (42).
Yu et al., reported case series of 9 bronchial thoracoscopic sleeve lobectomies performed through four ports. The authors modified the technique from interrupted sutures in the first cases to a continuous suture combined with discontinuous anastomosis in the late surgeries. The mean surgical time was 203±20 min. Two 28F chest tubes were placed at the end of the operation. The total duration of hospitalization lasted, on average, 20.8 ± 2 days. No recurrences or severe complications were reported (52).
Agastian et al. reported 21 VATS bronchoplastic procedures (9.1% of all VATS in his serie) including wedge (9), sleeve bronchoplasty (8) and other extended bronchoplasties (4). The authors used an interrupted suture technique for anastomosis. Mean surgical time was 287 min (range, 135–540 min), mean hospital stay was 5.2 days. Most of the cases were NSCLC (24). All brochial margins were negative for malignancy. Only one patient developed broncho pleural fistula and in a follow up of 26 months there was no tumor recurrence (36).
Xu et al. reported 20 sleeve lobectomies (including a RUL sleeve resection combined with half-carinal reconstruction and right medial lung sleeve resection combined with lower right dorsal segment). The average time of surgery was 239±51 min (range, 142–330 min), and the average time of airway reconstruction was 44±17 min (range, 22–75 min). The median postoperative hospital stay was 10 days (range, 8–12 days). None of the patients developed anastomotic leak and perioperative mortality was not observed. The bronchial suture was initially performed with a modified interrupted suture and subsequently with a continuous suture during which the membranous posterior and the cartilage wall were anastomosed with single 3/0 polypropylene suture (53).
The serie of Li et al. included 15 VATS sleeve lobectomies with bronchoplasty for NSCLC (RUL 10, right middle and lower lobes 1, left lower lobe 2 and LUL 2) by using 3 ports. The authors describe the technique for anastomosis by using a simple continuous and simple interrupted suturing of the membranous and cartilaginous portions of the bronchus. All procedures were uneventful, (only 1 minor complication) with a median operative time of 165 min (median bronchial anastomosis time of 44 min). The median duration of chest tube drainage was 5.4 days, and the median length of hospital stay was 7 days. All patients were followed postoperatively for a range of 1–16 months without tumor recurrence (43).
When experience is acquired with VATS, more advanced procedures such as double sleeve, tracheal or carinal resection can be performed by using even only a single incision (33). A perfect planning of the operation and coordination with the anesthesiologist are mandatory when dealing with these cases. The use of uniportal VATS for reconstructive surgery represents a challenge for the thoracic surgeon because of the technical difficulties for anatomic reconstruction, vascular and airway management.
There are few publications of VATS double sleeve procedures reported in the literature (54,55). Our group published several case reports of bronchoplastic procedures including vascular reconstruction (27) and double bronchial and vascular sleeve procedures (28,33). Huang et al. showed a retrospective multi-center study with thirteen thoracoscopic double sleeve resections for NSCLC patients. There were no conversions to thoracotomy. The median operative time was 263 min and the median postoperative hospital stay was 10 days (55).
The thoracoscopic technique for other complex procedures such as tracheal or carinal sleeve resections has recently been described (33). The classic approach for carinal reconstruction is the right thoracotomy or median sternotomy (29) but these complex procedures can be also performed by uniportal VATS through the right side. After carinal or tracheal resection, ventilation can be maintained by using a high ventilation jet (32) or by using an intraoperative single lumen tube (through the uniportal incision or adding an additional 1 cm skin incision). For resection of the distal trachea or carina, the left and the right main bronchus can be re-approached to create a new carina and then re-anastomosed to the trachea (33).
Conclusions
Thanks to the acquired experience with minimimally invasive techniques such the uniportal VATS, the broncoplastic procedures and even the most complex reconstructions including VATS broncho-vacular sleeve and carinal resections can be performed safely. These procedures must be performed as an alternative to pneumonectomy ensuring a safe anastomosis and complete tumor resection. Further studies will be necessary to evaluate the long term results of a large serie of these complex resections operated by uniportal VATS.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Villamizar NR, Darrabie MD, Burfeind WR, et al. Thoracoscopic lobectomy is associated with lower morbidity compared with thoracotomy. J Thorac Cardiovasc Surg 2009;138:419-25. [PubMed]
- Swanson SJ, Herndon JE 2nd, D'Amico TA, et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802da prospective, multi-institution feasibility study. J Clin Oncol 2007;25:4993-7. [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [PubMed]
- Kaseda S, Aoki T, Hangai N, et al. Better pulmonary function and prognosis with video-assisted thoracic surgery than with thoracotomy. Ann Thorac Surg 2000;70:1644-6. [PubMed]
- Yang X, Wang S, Qu J. Video-assisted thoracic surgery (VATS) compares favorably with thoracotomy for the treatment of lung cancer: a five-year outcome comparison. World J Surg 2009;33:1857-61. [PubMed]
- Maurizi G, D'Andrilli A, Anile M, et al. Sleeve lobectomy compared with pneumonectomy after induction therapy for non-small-cell lung cancer. J Thorac Oncol 2013;8:637-43. [PubMed]
- Krüger M, Uschinsky K, Hässler K, et al. Postoperative complications after bronchoplastic procedures in the treatment of bronchial malignancies. Eur J Cardiothorac Surg 1998;14:46-52; discussion 52-3. [PubMed]
- Bertolaccini L, Viti A, Terzi A. Moving beyond the boundary: the emerging role of video-assisted thoracic surgery for bronchoplastic resections. J Thorac Dis 2014;6:1170-2. [PubMed]
- Ng CS. Thoracoscopic sleeve resection-the better approach? J Thorac Dis 2014;6:1164-6. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Left lower sleeve lobectomy by uniportal video-assisted thoracoscopic approach. Interact Cardiovasc Thorac Surg 2014;18:237-9. [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [PubMed]
- Gonzalez-Rivas D, Yang Y, Sekhniaidze D, et al. Surgical technique for thoracoscopic suturing by uniportal VATS (tying the knots). Asvide 2016;3:062. Available online: http://www.asvide.com/articles/814
- Nakagawa T, Chiba N, Ueda Y, et al. Clinical experience of sleeve lobectomy with bronchoplasty using a continuous absorbable barbed suture. Gen Thorac Cardiovasc Surg 2015;63:640-3. [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [PubMed]
- Gonzalez-Rivas D, Yang Y, Sekhniaidze D, et al. Simple bronchoplasty for a right upper lobe endobronchial tumor. Asvide 2016;3:063. Available online: http://www.asvide.com/articles/815
- Kotoulas C, Lazopoulos G, Foroulis C, et al. Wedge resection of the bronchus: an alternative bronchoplastic technique for preservation of lung tissue. Eur J Cardiothorac Surg 2001;20:679-83. [PubMed]
- Gonzalez-Rivas D, Yang Y, Sekhniaidze D, et al. Right upper sleeve resection. Asvide 2016;3:064. Available online: http://www.asvide.com/articles/816
- Guido W, Gonzalez-Rivas D, Duang L, et al. Uniportal video-assisted thoracoscopic right upper sleeve lobectomy. J Vis Surg 2015;1:10.
- Yang R, Shao F, Cao H, et al. Bronchial anastomosis using complete continuous suture in video-assisted thoracic surgery sleeve lobectomy. J Thorac Dis 2013;5 Suppl 3:S321-2. [PubMed]
- Gonzalez-Rivas D, Yang Y, Sekhniaidze D, et al. Left upper lobe sleeve resection. Asvide 2016;3:065. Available online: http://www.asvide.com/articles/817
- Gonzalez-Rivas D, Yang Y, Sekhniaidze D, et al. Bronchus intermedius resection (sparing lung). Asvide 2016;3:066. Available online: http://www.asvide.com/articles/818
- Bagan P, Le Pimpec-Barthes F, Badia A, et al. Bronchial sleeve resections: lung function resurrecting procedure. Eur J Cardiothorac Surg 2008;34:484-7. [PubMed]
- Bölükbas S, Schirren J. Parenchyma-sparing bronchial sleeve resections in trauma, benign and malign diseases. Thorac Cardiovasc Surg 2010;58:32-7. [PubMed]
- Tang J, Cao M, Qian L, et al. The pure distal left main bronchial sleeve resection with total lung parenchymal preservation: report of two cases and literature review. J Thorac Dis 2014;6:E294-8. [PubMed]
- Gonzalez-Rivas D, Yang Y, Sekhniaidze D, et al. Left upper sleeve resection and vascular reconstruction. Asvide 2016;3:067. Available online: http://www.asvide.com/articles/819
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Single-port video-assisted thoracoscopic lobectomy with pulmonary artery reconstruction. Interact Cardiovasc Thorac Surg 2013;17:889-91. [PubMed]
- Gonzalez-Rivas D, Fieira E, de la Torre M, et al. Bronchovascular right upper lobe reconstruction by uniportal video-assisted thoracoscopic surgery. J Thorac Dis 2014;6:861-3. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [PubMed]
- Porhanov VA, Poliakov IS, Selvaschuk AP, et al. Indications and results of sleeve carinal resection. Eur J Cardiothorac Surg 2002;22:685-94. [PubMed]
- Shao F, Yang R, Xu D, et al. Bronchial sleeve lobectomy and carinal resection in the treatment of central lung cancer: a report of 92 cases. Zhongguo Fei Ai Za Zhi 2010;13:1056-8. [PubMed]
- Weder W, Inci I. Carinal resection and sleeve pneumonectomy. Thorac Surg Clin 2014;24:77-83. [PubMed]
- Watanabe Y, Murakami S, Iwa T, et al. The clinical value of high-frequency jet ventilation in major airway reconstructive surgery. Scand J Thorac Cardiovasc Surg 1988;22:227-33. [PubMed]
- Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i6-16. [PubMed]
- Ng CS, Lau KK, Gonzalez-Rivas D, et al. Evolution in surgical approach and techniques for lung cancer. Thorax 2013;68:681. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Agasthian T. Initial experience with video-assisted thoracoscopic bronchoplasty. Eur J Cardiothorac Surg 2013;44:616-23. [PubMed]
- Rendina EA, De Giacomo T, Venuta F, et al. Lung conservation techniques: bronchial sleeve resection and reconstruction of the pulmonary artery. Semin Surg Oncol 2000;18:165-72. [PubMed]
- Burfeind WR Jr, D'Amico TA, Toloza EM, et al. Low morbidity and mortality for bronchoplastic procedures with and without induction therapy. Ann Thorac Surg 2005;80:418-21; discussion 422. [PubMed]
- Santambrogio L, Cioffi U, De Simone M, et al. Video-assisted sleeve lobectomy for mucoepidermoid carcinoma of the left lower lobar bronchus: a case report. Chest 2002;121:635-6. [PubMed]
- Nakanishi R, Fujino Y, Yamashita T, et al. Thoracoscopic anatomic pulmonary resection for locally advanced non-small cell lung cancer. Ann Thorac Surg 2014;97:980-5. [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [PubMed]
- Mahtabifard A, Fuller CB, McKenna RJ Jr. Video-assisted thoracic surgery sleeve lobectomy: a case series. Ann Thorac Surg 2008;85:S729-32. [PubMed]
- Li Y, Wang J. Video-assisted thoracoscopic surgery sleeve lobectomy with bronchoplasty: an improved operative technique. Eur J Cardiothorac Surg 2013;44:1108-12. [PubMed]
- Tsuchiya R. Bronchoplastic techniques. In: Pearson FG, Cooper JD, Deslauriers J, et al, eds. Thoracic Surgery. New York: Churchill Livingstone; 2002:1005-13.
- Yu DP, Han Y, Zhao QY, et al. Pulmonary lobectomy combined with pulmonary arterioplasty by complete video-assisted thoracic surgery in patients with lung cancer. Asian Pac J Cancer Prev 2013;14:6061-4. [PubMed]
- Nakanishi R, Yamashita T, Oka S. Initial experience of video-assisted thoracic surgery lobectomy with partial removal of the pulmonary artery. Interact Cardiovasc Thorac Surg 2008;7:996-1000. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [PubMed]
- Li X, Pan X, Zhang C, et al. Video-assisted thoracoscopic sleeve lobectomy. J Thorac Dis 2014;6:1351-3. [PubMed]
- Liu K, Jin C, Tian H, et al. Total video-assisted thoracic surgery sleeve lobectomy: suture by both hands. Thorac Cardiovasc Surg Rep 2013;2:43-5. [PubMed]
- Lu H, Zhang Z, Li W, et al. Video-assisted thoracic surgery right sleeve lobectomy. J Thorac Dis 2013;5 Suppl 3:S323-4. [PubMed]
- Jiao W, Zhao Y, Huang T, et al. Two-port approach for fully thoracoscopic right upper lobe sleeve lobectomy. J Cardiothorac Surg 2013;8:99. [PubMed]
- Yu D, Han Y, Zhou S, et al. Video-assisted thoracic bronchial sleeve lobectomy with bronchoplasty for treatment of lung cancer confined to a single lung lobe: a case series of Chinese patients. J Cardiothorac Surg 2014;9:67. [PubMed]
- Xu X, Chen H, Yin W, et al. Thoracoscopic half carina resection and bronchial sleeve resection for central lung cancer. Surg Innov 2014;21:481-6. [PubMed]
- Liu L, Mei J, Pu Q, et al. Thoracoscopic bronchovascular double sleeve lobectomy for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;46:493-5. [PubMed]
- Huang J, Li J, Qiu Y, et al. Thoracoscopic double sleeve lobectomy in 13 patients: a series report from multi-centers. J Thorac Dis 2015;7:834-42. [PubMed]



