Giant saccular superior vena cava aneurysm—a rare and difficult clinical case
Introduction
A superior vena cava (SVC) aneurysm is an extremely rare case of vascular malformation in the chest cavity. Since 1949, when Abbot described a patient with a SVC aneurysm for the first time, there have only been a few more than 30 cases reported in medical literature (1). The majority of them are fusiform aneurysms circumstantially detected in chest X-rays. In our case we report a more unusual saccular aneurism of SVC. This pathology may cause severe hemorrhaging or pulmonary embolism and should be operated on.
Case presentation
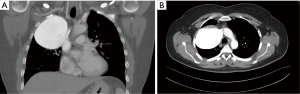
Our case is a 57-year-old woman with an 8 cm wide saccular aneurysm of SVC. Because of dyspnea and minor chest pain, a chest X-ray was performed which revealed an oval opacity in the right upper lobe. The patient’s medical history indicated nothing of relevance, but there was record of trauma. A chest computed tomography (CT) scan was done and this showed an extensive 75 mm × 79 mm × 81 mm mass filled with contrast from SVC. The mass was constricting the right lung parenchyma and partially narrowing the right innominate vein. The inferior circuit was adjoining the right pulmonary vein. The mass was in contact with the anterolateral chest cavity wall and was adjoining the superior mediastinum. Due to the connection with SVC we diagnosed a huge saccular aneurism (Figure 1). Resection surgery was planned. Under general anesthesia the chest cavity was opened using the median sternotomy approach. A cardiopulmonary bypass (CPB) was used, cannulating the ascending aorta and both the superior and inferior vena cava. After opening the pleural cavity, a giant vein aneurism of 8.5 cm × 8.7 cm in size was discovered. The aneurysm filled one third of the pleural cavity space and was entirely constricting the right upper lobe of the lung. After the mass was dissected from the right phrenic nerve and the surrounding tissue, we used a vascular clamp to exclude the neck of the aneurism. The mass was detached; the neck of the aneurysm was continuously sutured and strengthened with teflon felt patches (Figure 2). A histopathological examination was conducted and this confirmed that the mass which had been removed was a part of a venous blood vessel. A control CT scan and chest X-ray was done after surgery (Figure 3). Because of an uneventful postoperative period, the patient was discharged on the 5th day after the procedure.
Discussion
A vein aneurysm is an extremely rare phenomenon in medicine. In 1963, Abbot and Leight introduced a classification of aneurysms and divided them into four groups (congenital, acquired, pseudo-aneurysm, and arteriovenous aneurysm) (2). The fusiform aneurysm constitutes the vast majority. In our case we are presenting a saccular aneurysm, which has only been described in literature a few times. Such aneurysms are usually asymptomatic and are usually diagnosed accidentally in routine chest X-rays. Detailed diagnostics include a CT scan or magnetic resonance imaging (MRI). Aneurysms might be congenital, or caused by inflammation or by the degeneration of the vascular wall, but in most cases their cause is unknown (3). They might be solitary or they may coexist with cystic hygromas and angiomas. In asymptomatic patients where the diameter of the aneurysm is less than 40 mm, we might proceed conservatively, using anti-plaque therapy and periodic scans (4). Aneurysms which are larger, growing, symptomatic or containing thrombus require radical surgical treatment (3,5,6). Part of the thrombus forming the sack of the aneurysm can break away and cause pulmonary embolism or lung infarct which may lead to the patient’s death (7,8). Particular caution is required in this circumstances. Thanks to CPB, our patient was protected from pulmonary embolism and lung infarct. The use of CPB should be considered not only when the thrombus formation is detected, but also in the case of calcification in the wall of the aneurysm (5). In our opinion, the type of surgical approach presented here gives better insight into the operative field, especially in the neck area of the aneurysm. It also provides security for the patient and comfort for the surgeon. The procedure allows extravasated blood to be returned and prevents excessive blood loss. The alternative to open surgery is an endovascular approach. This involves a thrombin injection into the sack of the aneurysm. In our case this could not be done because the entrance of the aneurysm was 4 cm wide (9).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Abbott OA. Congenital aneurysm of superior vena cava; report of one case with operative correction. Ann Surg 1950;131:259-63, illust. [Crossref] [PubMed]
- Abbott OA, Leigh TF. Aneurysmal dilatations of the superior vena caval system. Ann Surg 1964;159:858-72. [Crossref] [PubMed]
- Pasic M, Schöpke W, Vogt P, et al. Aneurysm of the superior mediastinal veins. J Vasc Surg 1995;21:505-9. [Crossref] [PubMed]
- Koga S, Ikeda S, Sanuki Y, et al. A case of asymptomatic fusiform aneurysm of the superior vena cava detected by magnetic resonance imaging. Int J Cardiol 2006;113:e39-41. [Crossref] [PubMed]
- Varma PK, Dharan BS, Ramachandran P, et al. Superior vena caval aneurysm. Interact Cardiovasc Thorac Surg 2003;2:331-3. [Crossref] [PubMed]
- Gozdziuk K, Czekajska-Chehab E, Wrona A, et al. Saccular aneurysm of the superior vena cava detected by computed tomography and successfully treated with surgery. Ann Thorac Surg 2004;78:e94-5. [Crossref] [PubMed]
- Ream CR, Giardina A. Congenital superior vena cava aneurysm with complications caused by infectious mononucleosis. Chest 1972;62:755-7. [Crossref] [PubMed]
- Nakamura Y, Nakano K, Nakatani H, et al. Surgical exclusion of a thrombosed azygos vein aneurysm causing pulmonary embolism. J Thorac Cardiovasc Surg 2007;133:834-5. [Crossref] [PubMed]
- Jargiello T, Durakiewicz M, Sojka M, et al. Saccular aneurysm of superior vena cava treated with percutaneous, transcatheter thrombin injection. Cardiovasc Intervent Radiol 2014;37:529-32. [Crossref] [PubMed]