Reasons not to perform uniportal VATS lobectomy
Introduction
There is little doubt that uniportal video-assisted thoracic surgery (VATS) has become the most exciting technical development in thoracic surgery over the past 5 years (1-3). First introduced as a minimally invasive approach for minor thoracic procedures by pioneers such as Dr. Gaetano Rocco, it has since been developed to encompass major lung resections—most famously by Dr. Diego Gonzalez Rivas (1,4-9). Today, hardly a Thoracic Surgery conference goes by without uniportal VATS being a much-discussed topic. Workshops and symposia teaching this approach can be found frequently in virtually every corner of globe. The popularity surrounding this approach is becoming quite evident throughout the specialty.
However, as with any ‘new kid on the block’ generating mass excitement—whether it is Muhammad Ali, rock n roll music, or robotic surgery—there will inevitably be some backlash from the establishment (10,11). Feted by many, uniportal VATS has also received increasing criticism from some well-respected voices. This was quite evident, for example, at the European Conference on General Thoracic Surgery in Lisbon in 2015 (12,13). Whether it was in the form of heated debate at the Breakfast Session, or in the form of sarcastic humour at the Postgraduate Course, many were now beginning to voice concerns about Uniportal VATS. A schism appears to have appeared between proponents and opponents of the approach, and this debate could have far-reaching implications for the future direction of Minimally Invasive Thoracic Surgery.
It would be easy—and churlish—for proponents to dismiss criticism of uniportal VATS as ‘sour grapes’ from those who do not perform it. However, such an attitude would be counter-productive in terms of advancing medical science. Instead, it must be realized that opponents of uniportal VATS may actually have very valid reasons for opposing it. Understanding the bases of their arguments is crucial in order to develop, regulate and improve the surgical approach so that ultimately patients can benefit. This article seeks to summarise some of evidence (or lack thereof) for those arguments, with a view towards furthering such a fairer understanding.
The supposed pros and cons of uniportal VATS
Proponents of uniportal VATS lobectomy have been vociferous in suggesting the potential benefits of this approach. The logic is simple to understand: if conventional multiportal VATS is superior to open thoracotomy by virtue of minimizing surgical access trauma (14,15), then further reduction in such access trauma should yield even greater benefits. Therefore, reducing the number of wounds from three or four to just one, should, in theory, lead to:
Furthermore, it has been argued that the visualization geometrics afforded by uniportal VATS allow a more ergonomic and natural hand-eye approach for the surgeon to operate with (18).
However, opponents of the approach point to the technical challenge of having all instrumentation sharing the same access incision alongside the video-thoracoscope (13,19). The crowding of the scope and instruments, it is argued, leads inevitably to compromised dexterity. The analogy is to suggest the surgeon and the assistant are playing a game of ‘Twister’. With such compromised operating, the opponents suggest that:
- Patient safety is put at risk;
- Adequacy of oncologic clearance is not achieved.
If such basic tenets of good surgery are not rigorously upheld, then the approach should not be practised—regardless of any purported benefits. In any case, they also argue, these ‘benefits’ may not even exist outside the realm of the hypothetical (12,13).
The battle lines have been drawn. The question is which side will emerge the victor. To decide that, a battlefield must be defined.
Resolving the debate: lessons from the history of conventional VATS
It turns out that that the battleground is not hard to find. In fact, a very similar battle was fought here not so long ago.
When conventional multiportal VATS lobectomy was first developed in the 1990s, it represented as much of a technical revolution then as uniportal VATS does now—perhaps even more so. The change from open thoracotomy to ‘keyhole’ surgery represented a huge leap not only in terms of surgical technique, but in clinical philosophy and oncologic strategy (3,15). Not surprisingly, many renowned surgeons of the day voiced misgivings and deep concerns about the new upstart approach. Their arguments were that the use of the small surgical access incisions compromised the surgery in terms of operative safety and oncological efficacy (15,20). If these basic tenets of good surgery could not be upheld, then VATS should not be performed.
In other words, the exact same arguments used against uniportal VATS today were used against conventional multiportal VATS two decades ago!
Today, there is no question that conventional multiportal VATS lobectomy is a well-established, central element of lung cancer management. It is, in fact, regarded by authoritative international guidelines as being the preferred surgical approach for the management of lung cancer (21). How did multiportal VATS go from being a shunned ‘alternative’ to open thoracotomy to becoming enshrined as the favoured approach for treating lung cancer? The answer lies in winning the key battles on the most important battleground of all: clinical evidence.
Over the past 20-odd years, the pioneers of VATS have relentlessly conducted clinical research looking at the use of VATS for treating a range of disease, especially lung cancer. The research started from simple beginnings and gradually matured (3,15). The evidence generated became increasingly sophisticated and convincing. Eventually, the world of Thoracic Surgery was forced to accept the evidence and embrace VATS. This evolution of the research and evidence-gathering can be categorized into five distinct phases that neatly correspond to the development of a human:
Infancy—safety & feasibility
As a new surgical technique is introduced (such as VATS in the early 1990s), the first most important issue to prove is its safety. Following the Hippocratic dictum of primum non nocere, it is imperative to demonstrate that the procedure will not harm patients. This is actually not too difficult to do. Simple case reports, and then increasingly larger case series can adequately show that the approach can be performed with reasonable safety. And this was in fact what happened with VATS lobectomy in the early 1990s. Some of the initial papers showing that VATS lobectomy was feasible and could be performed with reasonable safety have now become legendary (22-25). Just as importantly, similar case series emerged from different centers around the world, making the important point that the technique itself was a sound, reproducible one (26-28).
Childhood—crude benefit
The next step in the development of VATS was to show that it could be better than open surgery. The most obvious outcome measures for an approach designed to minimize surgical trauma were: reduction of pain, reducing crude morbidity rates, and expediting recovery. As VATS moved into the mid-1990s, these were exactly the outcome measures used to compare VATS and open thoracotomy. The initial comparisons were between a series of VATS patients with historical cohorts of patients receiving thoracotomy (29). As the studies developed, the comparisons were made using case-matching of patients in the study arms to add to the scientific quality (30). These studies—to this day—have established VATS as offering patients less pain and shorter hospital stays. There have, of course, been attempts at randomized trials to compare open surgery and VATS (20). However, the cachet of a randomized trial methodology is not always matched by correspondingly stringent interpretation of results. In one of the few randomized trials ever conducted (20), it is peculiar that despite the finding that “significantly more postoperative complications occurred in the thoracotomy group” and no data showing worse outcomes for VATS in any parameter, the paper concluded that VATS “continues to expose the patient to the risk of major pulmonary resection being done in an essentially closed chest” and warned against accepting VATS! Thankfully, the avalanche of accumulated clinical data showing the benefits of VATS has since rendered this randomized trial obsolete (14,15). Today, it is accepted that thoracic surgeons and their patients are so convinced of the benefits of VATS that future randomized trials are unlikely to be feasible, or even ethical (31).
Adolescence—objective, quantifiable benefit
Through the 1990s, it gradually became evident that pain scores, chest drain durations and lengths of stay were inadequate as outcome measures to show the advantages of VATS over open surgery (15). These were subjective measurements that could be influenced by a disconcertingly large number of confounding variables. These included individual patient pain thresholds, postoperative analgesic protocols, variability of chest drain suction algorithms and removal criteria, socio-cultural acceptance of early discharge, and so on (32). The quest for more reliable outcome measurements led to ever more sophisticated study designs. Instead of subjective pain scores per se, meticulous quality-of-life assessments using authoritative and validated questionnaires, patient mobilization, and shoulder function were used as quantifiable surrogate measurements of pain (33-35). More intriguingly, inflammatory markers (including cytokines and indicators of humoral and cellular immune activation) were used to demonstrate that VATS caused less systemic and physiological disruption than open surgery (36-38). These lab-proven benefits—objective and free from observer bias—provided irrefutable and convincing evidence that VATS was indeed less ‘invasive’ than open surgery.
Adulthood—treatment efficacy
Even with benefits proven, the use of VATS cannot be justified unless it provided equivalent treatment outcomes as open surgery (then the gold standard). In terms of lung cancer surgery, this meant completeness of resection and survival. For completeness of resection, the most used surrogate measurement was lymph node dissection adequacy. That VATS could allow equivalent nodal dissection as open surgery was proven by a series of simple but effective comparative studies (39-41). More important was the demonstration of equivalent survival. Through the late 1990s and early 2000s, a reasonable volume of clinical data was accumulated comparing lung cancer survival after VATS and open surgery. These ultimately culminated in the last 10 years with a series of well-executed systematic reviews and meta-analyses comparing lung cancer survival between the VATS and open approaches (42-44). In summary, these have now demonstrated that VATS is not only equivalent to open thoracotomy in the treatment of lung cancer, but may even be marginally superior in terms of survival for early-stage disease. It should be remarked upon that this adulthood phase of the clinical evidence (showing survival) occurred after the childhood and adolescence phases (showing benefit)—because collecting data on immediate post-op benefit is relatively easier, whereas survival data requires many years of good follow-up. For patients operated on in the 1990s, long-term survival data would not be ready until the early 2000s, and subsequently the time needed for accumulation of case series data dictates that the meta-analyses would not be available until relatively recently. This long wait is necessary and well worth the while. The demonstration of treatment efficacy by VATS is what has directly led to VATS being declared not just an alternative to open thoracotomy, but actually “preferred over a thoracotomy for anatomic pulmonary resection” for stage I lung cancer in the international guidelines (21).
Maturity—sustainability
Even after all the important work on safety, benefits and efficacy have been done, there can still be some clinical research published on a mature surgical entity such as conventional multiportal VATS. Such research may lie in demonstrating that VATS is a sustainable approach: it is not a flash in the pan, but something that is here to stay. Studies in this regard have shown that VATS is cost-effective for any health system to adopt, and that VATS can be readily passed on from one generation of Thoracic Surgeons to the next (45,46).
The above brief history of clinical evidence for conventional multiportal VATS has taught us that establishing a revolutionary, new surgical approach is not an easy task. It requires perseverance, patience and plenty of time to achieve. However, that arduous undertaking is rewarded—provided the approach is a good one—by a glorious body of clinical evidence that will convince even the most stubborn critics.
What is the evidence for uniportal VATS?
It follows from the above that in order to win over critics today and establish uniportal VATS as a viable, mainstream surgical approach, clinical evidence must be generated. Moreover, that evidence can be generated in the same sequence of evolutionary phases, from infancy through to adulthood. In this context, how far have we come with evidence for uniportal VATS?
Case reports and case series
A casual Medline search was conducted using the Ovid search engine on 30 Nov 2015. The following search strategy was used: (“VATS” or “thoracoscopic” in Title) AND (“uniportal” or “single” in Title). This yielded 153 results—of which over 120 were ostensibly papers on uniportal VATS. The publication dates of the latter ranged from Feb 2004 to Oct 2015. Of these, over 90% were case reports and simple, non-comparative case series. Although this is admittedly an extremely crude, non-scientific literature search, it readily illustrates two very important ideas.
The first idea is that there is a very sizeable volume of case reports and case series on uniportal VATS. Almost unanimously, they claim that uniportal VATS is safe and feasible. Amongst these papers, some of those concerning uniportal VATS lobectomy have already become amongst the most cited papers in the recent thoracic surgery literature (2,3,8,9). Furthermore, these have demonstrated that the uniportal technique can be applied safely for an ever increasing range of lung resection procedures—ranging from segmentectomies to complex sleeve and double-sleeve resections (1,6,7,9). The fact that such a body of clinical documentation exists—together with no reports that the uniportal approach for lobectomy has been shown to be harmful in any way—attests to the safety of the approach. This is further corroborated by the increasing use of uniportal VATS as the standard approach for lobectomy in centers around the world (3,17,18,47,48). The volume of case reports and case series on uniportal VATS is currently approaching that on conventional multiportal VATS in the mid- to late-1990s when the latter was becoming gradually accepted as an ‘alternative’ to thoracotomy (14,15). It is perhaps now reasonable to conclude that the safety of using the uniportal VATS has been adequately demonstrated and that the ‘infancy’ phase of the clinical evidence accumulation has been passed.
The second idea brought out by the extremely high proportion of case reports and case series is that there is a relative paucity of ‘higher tier’ evidence on uniportal VATS Lobectomy. Although ‘infancy’ is passed, has the approach reached the ‘childhood’/‘adolescence’ phase yet in terms of evidence?
Comparative studies
Perusal of the medical literature (not a proper systematic review) reveals that 8 comparative studies have thus far been published by 7 groups comparing uniportal VATS with conventional multiportal VATS for anatomical resection of lung cancer (49-56). These are summarized in Table 1.
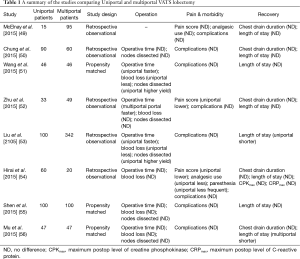
Full table
All 8 studies were retrospective, observational studies. All were published in 2015. Interestingly, 7 of these studies originated from Asia. Of the 8 studies, three were case-matched studies, and the rest were unmatched comparisons. All studies focused on post-operative clinical outcomes. None of these studies had medium- or long-term follow-up and none looked at post-operative survival—whether overall or cancer-related.
The findings from the eight studies can be broadly categorized into 3 main areas:
- Operation. Of the 7 studies providing data in this area, 2 found that uniportal VATS gave shorter operation times (170 vs. 191 min and 3.0 vs. 3.5 h respectively), less blood loss 53 vs. 95 mL and 56 vs. 78 mL respectively), and higher yields from lymph node dissection (27 vs. 22 nodes and 28 vs. 25 nodes respectively) (51,53). However, both of these studies came from the same center. Another study actually showed that operation times were longer with uniportal VATS (180 vs. 151 min) (52). The remaining 4 studies found no difference between the approaches in terms of intraoperative parameters;
- Pain & morbidity. uniportal VATS was found to give lower postoperative pain scores in 2 studies (3.6 vs. 5.5 and 2.4 vs. 4.2 respectively), and one of these further noted quicker cessation of analgesic use and lower frequency of paresthesia following uniportal VATS (52,54). However, in all of the remaining 6 studies, uniportal VATS was not associated with any advantage in terms of postoperative morbidity. None of the studies found that overall complication rates were lower amongst uniportal patients;
- Recovery. Shorter postoperative length of stay was associated with uniportal VATS in one study (6.0 vs. 6.8 days), but with conventional multiportal VATS in another (6.8 vs. 5.4 days) (53,56). In all of the remaining 6 studies, uniportal VATS was not associated with any advantage in terms of chest drain durations or lengths of stay.
Only one of the above studies looked at inflammatory markers (54). Maximum postoperative levels of creatine phosphokinase and of C-reactive protein were measured, but no difference was noted between patients receiving uniportal and multiportal VATS.
And the winner is…
Based on the above evidence, one can now look back at the arguments put forth by the proponents and opponents of uniportal VATS. Which side is the ‘winner’ of this debate?
Proponents of uniportal VATS
The argument of the proponents is that uniportal VATS can reduce pain and morbidity, and it can expedite postoperative recovery.
In terms of the first claim about pain, the evidence that uniportal VATS is superior to conventional multiportal VATS is decidedly weak. Only 2 out of 6 studies supported this notion (52,54), with the remainder showing no difference. In both studies, the main assessment tool for pain was the simple numeric scale, asking patients to subjective grade the pain with a score of 0–10. Although widely used, this scale is inherently subjective and confounding variables—such as individual patient pain thresholds, circumstances under which pain is scored (at rest, moving, etc.), and so on. This problem is even greater amongst studies with small cohorts such as these. Moreover, in both the studies suggesting an ‘advantage’ for the uniportal approach, there is no evidence that intra-operative analgesia (e.g., regional blockade) or post-operative analgesia had been standardized amongst all patients (52,54). The reliability of the conclusions is therefore still subject to some doubt.
With regards the second claim regarding faster recovery, the evidence is even less favourable for uniportal VATS. Only one study showed shorter lengths of stay after uniportal VATS lobectomy, but this is countered by another study showing longer lengths of stay after the same approach (53,56). All of the other studies showed no difference. The authors of the study showing longer stays after uniportal lobectomy still argued in favour of this approach, and attempted to explain away the unfavourable finding by suggesting that lengths of stay were prolonged in the uniportal group because of poorer wound healing at the chest drain site (56). Nonetheless, they have not provided actual data to illustrate this point—and in any case, this would merely point to another potential weakness of the uniportal approach that may nullify any supposed benefits in terms of faster recovery. Ultimately, however, the issue of lengths of stay is a complex one that also involves many confounding variables—including patient confidence, socio-cultural influences on readiness for early discharge, financial considerations against prolonged stay (or lack thereof), and so on (32). The failure of the comparative studies to find any benefit for a supposedly less invasive approach may suggest that these variables may be even more important than surgical technique in determining length of stay—and call into question whether this ‘advantage’ of uniportal VATS is really that great (12,13).
At this juncture, it seems that both of the key claims of the proponents of uniportal VATS have not been well supported by the (limited) available evidence in comparative studies. To be fair, on balance these studies also show non-inferiority of the uniportal approach—but is that is certainly not what proponents are hoping for. So have the opponents ‘won’ this debate?
Opponents of uniportal VATS
The opponents of uniportal VATS also have two main lines of argument: that this upstart approach compromises operative safety, and that it does not achieve equivalent treatment efficacy.
The first claim regarding safety is easily refuted by the volume of case reports and case series showing uniportal VATS being performed safely in many centers around the world and over several years of experience (1-9,47-56). The published literature is very one-sided in this regard: virtually all the papers have thus far demonstrated reasonable rates of mortality, morbidity and conversion to open surgery when uniportal VATS lobectomy is performed worldwide. There has not been any published evidence to suggest that it has led to increased harm for any patient. In the comparative studies above, 2 studies from one group of authors showed shorter operating times and less blood loss when using uniportal VATS, and 1 study showed longer operating times but no difference in blood loss when using uniportal VATS (51-53). All other studies showed no difference. In contrast to the claims about pain and faster recovery, it is not necessary to demonstrate superiority of uniportal VATS. Instead, what these comparative studies have together adequately demonstrated is that uniportal VATS is evidently not inferior in terms of operative parameters and hence there is no compromise to safety.
For the second claim about treatment efficacy (with regards to lung cancer particularly), the only ‘evidence’ provided is in terms of number of lymph nodes dissected. This is a well-accepted surrogate for respective efficacy, because it is impossible to gauge the ‘radicality’ of a lobectomy—a lobe is a lobe. This parameter was studied in 6 of the comparative studies, and 2 of these (albeit both by the same group of authors) found that nodal yields were actually higher in the uniportal group (51,53). However, once again, it is important to note that there is no need to demonstrate superiority of uniportal VATS here. The fact that none of the 6 studies showed that nodal yields were less in the uniportal group is sufficient to prove non-inferiority—and hence adequately refute the claim of the opponents.
Nevertheless, the most important measure of treatment efficacy when it comes to lung cancer must be survival. None of the studies thus far has focused on this outcome measure. This is not too surprising, given that uniportal VATS lobectomy for lung cancer was only first reported 5 years ago, and so long-term follow-up is still lacking. The experience with conventional multiportal VATS as discussed above has shown that good case series with sizeable patient cohorts only emerge 5–10 years after the technique is introduced (15). Following this crude logic, one can expect that clinical data regarding lung cancer survival after uniportal VATS lobectomy will start to appear in the next few years. These are eagerly awaited.
For the time being, the available evidence already gives a clear picture regarding the argument of the opponents of uniportal VATS. The evidence emphatically demonstrates the non-inferiority of uniportal VATS lobectomy compared to conventional multiportal VATS lobectomy.
The verdict (for now)
To use a boxing analogy, neither side has landed a knockout blow. The young challenger (uniportal) has weathered the onslaught of criticisms from the reigning champion (multiportal VATS) and has gone the distance without falling. The attacks about safety and nodal dissection adequacy have been well defended against by the available evidence. However, the challenger has not done enough to wrest the title from the champion: on the judges’ scorecards, the challenger has not been proven to be superior. The evidence for any advantage in terms of reducing morbidity and hastening recovery are very weak, if at all existing.
At the time of this writing, it is safe to declare this contest a draw.
What needs to be done now
Now is a good time to reflect on the contest though. A critique of the above comparative studies will show that the quality of evidence is not entirely impeccable (49-56). Five of the 8 studies are crude comparisons with no methodology to match the study arms. All are retrospective, and hence potentially subject to bias (including in outcome assessments). No sample size estimation was conducted. Ultimately, even where differences between the study arms were found, the absolute numerical difference was often not very great. There is therefore a pressing need to generate more and better quality clinical data to better define the role of uniportal VATS lobectomy in Thoracic Surgery.
At stake is more than just a clinico-academic debate amongst surgeons over which approach is better. Instead, investigating if uniportal VATS is any ‘better’ may lead to even more important questions about why it might be better (3,15). During the evolution of multiportal VATS, the progressive improvement in the research done (as explained above) revealed many important insights to Thoracic Surgeons. For example, it was realized that rib-spreading (more than incision length per se) was the key culprit in post-thoracotomy pain (15,35,57,58). It was learned that ‘pain’ after a thoracic operation was multi-factorial and hence individual components (such as neuropathy) may need to be treated separately (57,59,60). It became understood that surgical trauma is not just local but systemic, and that this may have implications on patient outcomes and survival (36-38,42-44). In the same way, it is the genuine hope of this author that the search to see whether uniportal VATS is any better in some patients will lead to newer revelations about how thoracic surgery can be made better for all patients.
To develop the next stage of clinical research in uniportal VATS, lessons can be drawn again from the history of multiportal VATS research (3,15). The following are four points for the reader to consider:
- With uniportal VATS, clinical research has now advanced well beyond the ‘infancy’ phase. Too many case reports and simple case series have been published over the last few years on this approach. It is becoming boring and even tedious to see yet another set of authors boasting of their own single institute’s experience in performing uniportal VATS for one condition or another. The point about proving safety and feasibility of the approach has already been well made. It is time to move on. If proponents of uniportal VATS continue to submit case reports and case series, this not only fails to advance the specialty, but it also provides more fodder for the opponents—who will point to continued lack of evidence and progress with this technique;
- Uniportal VATS clinical research has now clearly moved into the ‘childhood’ phase of simple comparative studies. This much is clear by noting that all of the above mentioned comparative studies were published in 2015. It is also apparent that the standard of comparison is still relatively rudimentary—as it was in the early ‘childhood’ phase of multiportal VATS. As mentioned above, crude outcome measures highly vulnerable to confounding variables are still the bases for the comparisons (e.g., pain scores, lengths of stay, etc.). Most of the comparative studies are still using crude comparisons of a uniportal group with an unmatched or historical ‘control’ group of conventional multiportal VATS patients. Future studies will need to make greater use of study design techniques to minimize bias. If randomization if not feasible, then greater use of propensity score matching may be a viable alternative. As comparative studies move into the ‘adolescence’ phase, more sophisticated outcome measures will need to be employed. Again referring to the multiportal VATS experience, options include: validated quality of life assessment techniques, functional and/or physiological measurements, study of inflammatory and immune parameters perioperatively, and so on;
- The ‘adult’ phase may seem several years away, but it is essentially to start preparing now. This phase calls for assessment of survival after surgery, and will require years of follow-up of many patients before clinically useful data emerge. To produce a good paper on long-term cancer survival 5 years later, the data collection needs to start now. Proponents of uniportal VATS must therefore immediately start establishing clinical databases of all their patients (if they have not already started doing so). Furthermore, it is a good idea to consider collaborative efforts. The success of survival analysis depends to a large degree on sheer patient volumes. Not every institute has access to huge patient numbers by itself, and collaborations will help generate more convincing survival data more rapidly and effectively. However, to ensure compatibility of data, those collaborations should begin now—with partner institutes coming together to use mutually compatible databases with mutually agreed definitions of all clinical parameters;
- Following from the above point, the need to attain consensus amongst all advocates of uniportal VATS is a critical step. The history of multiportal VATS showed that poorly defined principles of what is or is not ‘VATS’ led to some disappointing and even damaging research which set back the progress of the approach for years (15,35,58,61,62). As uniportal VATS matures, it is therefore important for practitioners to unite and agree upon clinical standards. Future clinical research is only meaningful and representative if everyone is following the same principles of practice (although details in individual technique can vary widely). In the coming years, uniportal practitioners may need to come together to achieve this, either through existing professional associations in Thoracic Surgery, or by establishing special interest groups in uniportal VATS. Furthermore, structured and standardized training should be implemented to ensure that surgeons embarking on this technique meet a profession-wide accepted level of competence and safety. Such training could be provided under the auspices of these associations and interest groups, and/or could be run by special high volume centers with abundant experience in the uniportal technique.
Conclusions
The current debate about the role of Uniportal VATS lobectomy appears to have ended in a draw. There is not enough evidence to say it is ‘better’ and that it should become a ‘preferred’ approach for major lung surgery. On the other hand, there is sufficient evidence to say that it is safe and feasible—and that there is no reason why it should not be performed by those who have mastered the necessary skills.
The future, though, appears to be headed in a direction that may be favourable to uniportal VATS. If the trajectory of multiportal VATS is followed, clinical research in uniportal VATS will similarly go through the phases of comparative studies of increasing sophistication and of accumulation of vital survival data. The coming years ahead will provide ample time for uniportal VATS to prove its worth through generation of clinical evidence of increasingly better quality. A review article similar to this one, but written a few years from now, may probably conclude that the debate is no longer a draw, but a decisive victory for uniportal VATS.
The important message at this time is that the debate is a very important one to have. Despite the attractiveness of the uniportal approach, proponents must understand that the arguments of the opponents are very relevant. The reasons not to perform uniportal VATS are very much as important for patients as the reasons in favour of performing it. These reasons must never be dismissed or ignored. Properly facing up to this debate and seeking to resolve it through the generation of sound clinical evidence is the only way to ensure that patients emerge the ultimate victors.
Acknowledgements
The author wishes to thank Prof. Gening Jiang and Dr. Timothy Yang of the Shanghai Pulmonary Hospital for providing the platform for sharing of clinical ideas on which this article was based. The author further thanks Dr. Diego Gonzalez Rivas for his open-minded acknowledgment and feedback on the challenges facing uniportal VATS today.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [PubMed]
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17. [PubMed]
- Rocco G, Khalil M, Jutley R. Uniportal video-assisted thoracoscopic surgery wedge lung biopsy in the diagnosis of interstitial lung diseases. J Thorac Cardiovasc Surg 2005;129:947-8. [PubMed]
- Rocco G, Romano V, Accardo R, et al. Awake single-access (uniportal) video-assisted thoracoscopic surgery for peripheral pulmonary nodules in a complete ambulatory setting. Ann Thorac Surg 2010;89:1625-7. [PubMed]
- Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Single-port thoracoscopic lobectomy in a nonintubated patient: the least invasive procedure for major lung resection? Interact Cardiovasc Thorac Surg 2014;19:552-5. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [PubMed]
- D'Amico TA. Robotics in thoracic surgery: applications and outcomes. J Thorac Cardiovasc Surg 2006;131:19-20. [PubMed]
- Swanson SJ. Robotic pulmonary lobectomy--the future and probably should remain so. J Thorac Cardiovasc Surg 2010;140:954. [PubMed]
- Van Raemdonck D, Sihoe AD. Postgraduate symposium on general thoracic surgery. Lisbon, Portugal: the European Society of Thoracic Surgeons at the 23rd European Conference on General Thoracic Surgery; May 31, 2105.
- Hansen HJ. VATS lobectomy: multiportal access is the optimal access. Lisbon, Portugal: Breakfast Session conducted by the European Society of Thoracic Surgeons at the 23rd European Conference on General Thoracic Surgery; June 2, 2015.
- Sihoe AD, Yim AP. Video-assisted pulmonary resections. In: Patterson GA, Cooper JD, Deslauriers J, et al. editors. Thoracic surgery (3rd edition). Philadelphia, USA: Elsevier, 2008:970-88.
- Sihoe AD. The evolution of VATS lobectomy. In: Cardoso P. editor. Topics in thoracic surgery. Rijeka, Croatia: Intech, 2011:181-210.
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [PubMed]
- Tam JK, Lim KS. Total muscle-sparing uniportal video-assisted thoracoscopic surgery lobectomy. Ann Thorac Surg 2013;96:1982-6. [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [PubMed]
- Bertolaccini L, Viti A, Terzi A. Ergon-trial: ergonomic evaluation of single-port access versus three-port access video-assisted thoracic surgery. Surg Endosc 2015;29:2934-40. [PubMed]
- Kirby TJ, Mack MJ, Landreneau RJ, et al. Lobectomy--video-assisted thoracic surgery versus muscle-sparing thoracotomy. A randomized trial. J Thorac Cardiovasc Surg 1995;109:997-1001; discussion 1001-2. [PubMed]
- Howington JA, Blum MG, Chang AC, et al. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e278S-313S.
- Lewis RJ, Caccavale RJ, Sisler GE, et al. One hundred consecutive patients undergoing video-assisted thoracic operations. Ann Thorac Surg 1992;54:421-6. [PubMed]
- Roviaro G, Varoli F, Rebuffat C, et al. Major pulmonary resections: pneumonectomies and lobectomies. Ann Thorac Surg 1993;56:779-83. [PubMed]
- Kirby TJ, Mack MJ, Landreneau RJ, et al. Initial experience with video-assisted thoracoscopic lobectomy. Ann Thorac Surg 1993;56:1248-52; discussion 1252-3. [PubMed]
- McKenna RJ Jr. Lobectomy by video-assisted thoracic surgery with mediastinal node sampling for lung cancer. J Thorac Cardiovasc Surg 1994;107:879-81; discussion 881-2. [PubMed]
- Yim AP, Ko KM, Chau WS, et al. Video-assisted thoracoscopic anatomic lung resections. The initial Hong Kong experience. Chest 1996;109:13-7. [PubMed]
- Yim AP, Liu HP. Complications and failures of video-assisted thoracic surgery: experience from two centers in Asia. Ann Thorac Surg 1996;61:538-41. [PubMed]
- Walker WS, Pugh GC, Craig SR, et al. Continued experience with thoracoscopic major pulmonary resection. Int Surg 1996;81:255-8. [PubMed]
- Giudicelli R, Thomas P, Lonjon T, et al. Video-assisted minithoracotomy versus muscle-sparing thoracotomy for performing lobectomy. Ann Thorac Surg 1994;58:712-7; discussion 717-8. [PubMed]
- Demmy TL, Curtis JJ. Minimally invasive lobectomy directed toward frail and high-risk patients: a case-control study. Ann Thorac Surg 1999;68:194-200. [PubMed]
- D'Amico TA. Thoracoscopic lobectomy: evolving and improving. J Thorac Cardiovasc Surg 2006;132:464-5. [PubMed]
- Bachiocco V, Morselli-Labate AM, Rusticali AG, et al. Intensity, latency and duration of post-thoracotomy pain: relationship to personality traits. Funct Neurol 1990;5:321-32. [PubMed]
- Li WW, Lee TW, Lam SS, et al. Quality of life following lung cancer resection: video-assisted thoracic surgery vs thoracotomy. Chest 2002;122:584-9. [PubMed]
- Li WW, Lee RL, Lee TW, et al. The impact of thoracic surgical access on early shoulder function: video-assisted thoracic surgery versus posterolateral thoracotomy. Eur J Cardiothorac Surg 2003;23:390-6. [PubMed]
- Shigemura N, Akashi A, Nakagiri T, et al. Complete versus assisted thoracoscopic approach: a prospective randomized trial comparing a variety of video-assisted thoracoscopic lobectomy techniques. Surg Endosc 2004;18:1492-1497. [PubMed]
- Yim AP, Wan S, Lee TW, et al. VATS lobectomy reduces cytokine responses compared with conventional surgery. Ann Thorac Surg 2000;70:243-7. [PubMed]
- Craig SR, Leaver HA, Yap PL, et al. Acute phase responses following minimal access and conventional thoracic surgery. Eur J Cardiothorac Surg 2001;20:455-63. [PubMed]
- Ng CS, Lee TW, Wan S, et al. Thoracotomy is associated with significantly more profound suppression in lymphocytes and natural killer cells than video-assisted thoracic surgery following major lung resections for cancer. J Invest Surg 2005;18:81-8. [PubMed]
- Sagawa M, Sato M, Sakurada A, et al. A prospective trial of systematic nodal dissection for lung cancer by video-assisted thoracic surgery: can it be perfect? Ann Thorac Surg 2002;73:900-4. [PubMed]
- Watanabe A, Koyanagi T, Ohsawa H, et al. Systematic node dissection by VATS is not inferior to that through an open thoracotomy: a comparative clinicopathologic retrospective study. Surgery 2005;138:510-7. [PubMed]
- Denlinger CE, Fernandez F, Meyers BF, et al. Lymph node evaluation in video-assisted thoracoscopic lobectomy versus lobectomy by thoracotomy. Ann Thorac Surg 2010;89:1730-5; discussion 1736.
- Whitson BA, Groth SS, Duval SJ, et al. Surgery for early-stage non-small cell lung cancer: a systematic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg 2008;86:2008-16; discussion 2016-8.
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [PubMed]
- Rueth NM, Andrade RS. Is VATS lobectomy better: perioperatively, biologically and oncologically? Ann Thorac Surg 2010;89:S2107-11. [PubMed]
- Nakajima J, Takamoto S, Kohno T, et al. Costs of videothoracoscopic surgery versus open resection for patients with of lung carcinoma. Cancer 2000;89:2497-501. [PubMed]
- Ferguson J, Walker W. Developing a VATS lobectomy programme--can VATS lobectomy be taught? Eur J Cardiothorac Surg 2006;29:806-9. [PubMed]
- Shen Y, Liu Y, Feng M, et al. Uniportal video-assisted thoracoscopic lobectomy: Zhongshan experience. J Vis Surg 2015;1:5.
- Guido Guerrero W, Gonzalez-Rivas D, Hernandez Arenas LA, et al. Techniques and difficulties dealing with hilar and interlobar benign lymphadenopathy in uniportal VATS. J Vis Surg 2016;2:23.
- McElnay PJ, Molyneux M, Krishnadas R, et al. Pain and recovery are comparable after either uniportal or multiport video-assisted thoracoscopic lobectomy: an observation study. Eur J Cardiothorac Surg 2015;47:912-5. [PubMed]
- Chung JH, Choi YS, Cho JH, et al. Uniportal video-assisted thoracoscopic lobectomy: an alternative to conventional thoracoscopic lobectomy in lung cancer surgery? Interact Cardiovasc Thorac Surg 2015;20:813-9. [PubMed]
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [PubMed]
- Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [PubMed]
- Liu CC, Shih CS, Pennarun N, et al. Transition from a multiport technique to a single-port technique for lung cancer surgery: is lymph node dissection inferior using the single-port technique?†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i64-i72. [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i37-i41. [PubMed]
- Shen Y, Wang H, Feng M, et al. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i48-i53. [PubMed]
- Mu JW, Gao SG, Xue Q, et al. A Matched Comparison Study of Uniportal Versus Triportal Thoracoscopic Lobectomy and Sublobectomy for Early-stage Nonsmall Cell Lung Cancer. Chin Med J (Engl) 2015;128:2731-5. [PubMed]
- Sihoe AD, Au SS, Cheung ML, et al. Incidence of chest wall paresthesia after video-assisted thoracic surgery for primary spontaneous pneumothorax. Eur J Cardiothorac Surg 2004;25:1054-8. [PubMed]
- Shigemura N, Akashi A, Funaki S, et al. Long-term outcomes after a variety of video-assisted thoracoscopic lobectomy approaches for clinical stage IA lung cancer: a multi-institutional study. J Thorac Cardiovasc Surg 2006;132:507-12. [PubMed]
- Sihoe AD, Lee TW, Wan IY, et al. The use of gabapentin for post-operative and post-traumatic pain in thoracic surgery patients. Eur J Cardiothorac Surg 2006;29:795-9. [PubMed]
- Sihoe AD, Manlulu AV, Lee TW, et al. Pre-emptive local anesthesia for needlescopic video-assisted thoracic surgery: a randomized controlled trial. Eur J Cardiothorac Surg 2007;31:103-8. [PubMed]
- Yim AP, Landreneau RJ, Izzat MB, et al. Is video-assisted thoracoscopic lobectomy a unified approach? Ann Thorac Surg 1998;66:1155-8. [PubMed]
- Swanson SJ, Herndon JE 2nd, D'Amico TA, et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802--a prospective, multi-institution feasibility study. J Clin Oncol 2007;25:4993-7. [PubMed]


