Thoracoscopic surgery via a single-incision subxiphoid approach is associated with less postoperative pain than single-incision transthoracic or three-incision transthoracic approaches for spontaneous pneumothorax
Introduction
An increasing number of studies have demonstrated that thoracoscopic surgery is associated with decreased postoperative pain, reduced length of hospital stay, and fewer postoperative complications compared to open thoracotomy (1-5). Conventional thoracoscopic surgery is performed via three or four ports. In 2004, Rocco et al. reported on the use of single-incision thoracoscopic wedge resection for the treatment of diagnosis of interstitial lung diseases or treatment of primary spontaneous pneumothorax and found that uniportal thoracoscopic surgery for wege resection can be safe and effective (6). They also described 644 patients who underwent single-port thoracoscopic surgery for different indications (7) and the indications of single-incision thoracoscopic surgery were expanded. The potential advantage of reducing incisions is to decrease post-operative chest wall neuralgia and fasten recovery course.
Several studies have compared the intensity of self-reported postoperative pain and chest wall neuralgia between patients who received single-incision thoracoscopic surgery and those who underwent multiple-incision thoracoscopic surgery for pneumothorax (8-13). In some of those studies, acute postoperative pain was reported to be markedly lower in patients who received thoracoscopic surgery via a single incision than in patients who underwent surgery via three incisions. Nonetheless, even small chest wall incisions cause intercostal neuralgia and can result in chronic thoracotomy pain (6,14,15). A number of alternative methods have been developed to minimize trauma to the chest during surgery, including transvesical lung biopsy, transesophageal mediastinal lymph node dissection, transtracheal pericardial window creation, transoral dorsal sympathectomy, transumbilical lung resection and subxiphoid incision (16-23).
The subxiphoid approach to the thoracic cavity has been adopted in numerous procedures, such as subxiphoid pericardial window creation, coronary operations, thymectomy, ablative sympathectomy pulmonary wedge resection and lobectomy (16-25). Few studies have compared the perioperative and postoperative outcomes associated with single-incision subxiphoid transthoracic surgery, single-incision transthoracic surgery and three-incision thoracoscopic surgery. The aim of this study was to compare the intensity of acute chest pain associated with three thoracoscopic techniques, namely single-incision subxiphoid thoracoscopic surgery, single-incision transthoracic surgery and three-incision transthoracic thoracoscopic surgery for spontaneous pneumothorax.
Materials and methods
We retrospectively reviewed the surgical records of 57 consecutive patients who underwent thoracoscopic surgery for primary spontaneous pneumothorax at the Taipei Municipal Wanfang Hospital during the period August 2013 to September 2015. Data gathered from the records for analysis included demographic data, medical history, operative time, operative blood loss, length of hospital stay, duration of chest tube drainage, postoperative complications, and numeric pain rating scale scores. Surgical mortality was defined as death occurring during the same hospitalization or within 30 days after the operation. Indications for thoracoscopic surgery included recurrent pneumothorax or prolonged air leakage (>5 days). Thoracoscopic surgery was performed exclusively via the three-port approach in our hospital from 2009 to July 2013. Beginning in August 2013, we began to perform single-port incisions for patients with pneumothorax requiring thoracoscopic surgery and by the beginning of 2014 we began to perform thoracoscopic surgery via a single-incision subxyphoid approach. The indications for spontaneous pneumothorax were similar for all three approaches. Epidural analgesia is not used at our institution. The intensity of pain was estimated using an 11-point numeric rating scale. The numbers 0 to 10 are set out in a line at equal intervals, with the anchors ‘‘no pain [0]’’ and ‘‘pain as bad as you can imagine [10]’’ (26). The intensity of pain was evaluated immediately after surgery and then every 8 hours until discharge. The postoperative pain control protocol for all patients was as follows: diclofenac (25 mg) was administered every 6 hours during the postoperative course unless the numeric pain scale score was greater than 4, at which time intravenous injection of morphine (0.1 mg/kg) was administered. The pig tail was removed when postoperative chest plain films showed full expansion in both lungs without evidence of air leakage.
Surgical techniques
Patients were intubated with a double-lumen endotracheal tube under general anesthesia. The lateral decubitus positioning of the patients was based on the location of lesions. The blebs were identified using a thoracoscope. The pulmonary lesion was resected using a combination of endoscopic instruments (Scanlan International, Inc., USA) and an endo-stapler (Either Covidian or Ethicon End surgery, USA). Mechanical pleurodesis was also performed in the upper half of the pleural cavity by pleural abrasion with a cautery tip cleaner.
For three-port thoracoscopic surgery, a 30-degree 10-mm thoracoscope was placed through the 7th intercostal space in the mid-axillary line and a utility incision (2 cm) was made at the 5th intercostal space through which a wound protector (Alexis Wound Retractor, Applied Medical, USA) was introduced. Another 5-mm accessory port was placed at the 5th intercostal space in the posterior axillary line (Figure 1A). After the operation, a pig-tail drainage tube was inserted at the 7th intercostal space. For the single transthoracic approach, a 2-cm incision was created at the 5th intercostal space in the anterior axillary line through which a wound protector (Alexis Wound Retractor, Applied Medical, USA) was introduced (Figure 1B). After the operation, the 14-Fr pig-tail drainage tube was placed at the edge of incision wound. For the single subxiphoid incision, a 2-cm incision was made over the subxiphoid area (Figure 1C). A substernal tunnel extending from the wound to the pleural cavity was made by finger blunt dissection. The sternum was lifted with a retractor to provide an adequate working space. A 30-degree thoracoscope was introduced into the pleural cavity via the subxiphoid wound. A pig-tail drainage tube was placed in the pleural cavity and the subxiphoid wound was closed with 3-0 vicryl suture.

Statistical analysis
Continuous data are expressed as mean ± standard deviation (SD). Comparisons of continuous data between the three groups were made using the Krus-Wallis test. Categorical data were compared using the Chi-square or Fisher test. A P value <0.05 was considered to indicate statistical significance. All statistical analyses were performed using the statistical package SPSS for Windows (Version 12.0, SPSS, Chicago, IL, USA).
Results
During the period August 2013 to September 2015, fifty-seven patients with primary spontaneous pneumothorax underwent thoracoscopic pulmonary resection at the Wan Fang hospital. The 57 patients comprised 6 women and 51 men (Table 1). Of those patients, 14 received single-incision subxiphoid thoracoscopic surgery, 26 underwent single-incision transthoracic thoracoscopic surgery, and 17 received three-incision transthoracic thoracoscopic surgery. There were no significant differences in age, sex, side, surgical indication, operative blood loss, length of stay, duration of chest tube drainage or complications among the three groups. All surgeries were completed without the need for conversion to open surgery. There were no deaths in any of the groups and only one case of post-operative complication (prolonged air leakage) was observed in the single-incision thoracoscopic group. The patient was treated conservatively and was discharged on the 8th postoperative day. Operative time was significantly longer in the single-incision subxiphoid thoracoscopic surgery group than in the other two surgical groups (P=0.0064).
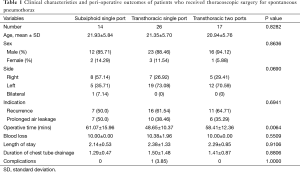
Full table
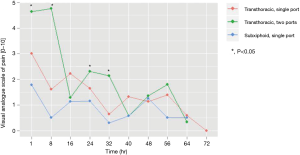
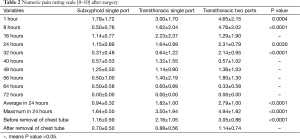
In all groups, pain intensity was highest during the first hour after surgery and then decreased with time (Figure 2). However, patients who underwent the single-incision subxiphoid procedure had significantly lower 1-, 8-, 24- and 32-hour postoperative pain scale scores than patients who underwent the other two procedures (Table 2). The average and maximum pain scale scores in the first 24 hours were lowest in the single-incision subxiphoid group (P<0.0001). However, there was no significant difference in pain scale scores among the groups after removal of the chest drainage tubes.
Full table
Discussion
In this study, we found that thoracoscopic surgery performed via a single subxiphoid port for spontaneous pneumothorax was associated with markedly less acute postoperative pain during the first 24 hours after surgery than single-incision thoracoscopic or three-incision thoracoscopic surgery.
Transthoracic thoracoscopic surgery is the most commonly employed approach to the thoracic cavity. Improvements in surgical instruments and surgical skill have resulted in a reduction in the number of incisions needed to perform thoracoscoic surgery. Single-incision thoracoscopic lobectomy and segmentectomy have been shown to result in perioperative outcomes similar to those of multiple-incision approaches (27). However, chest wall incisions are necessary even when performing thoracoscopic surgery via a single incision. The major shortcoming of the transthoracic thoracoscopic approach is chronic post-thoracotomy pain (6,14,15). Sihoe et al. (14) reported that more than half of their patients who received thoracoscopic surgery for spontaneous pneumothorax complained of chest wall paresthesia. Passlick et al. (28) found that 31.7% of patients who underwent three-port thoracoscopic surgery for spontaneous pneumothorax experienced chronic postoperative pain.
A subxiphoid incision is a simple and feasible route through which to enter the thoracic cavity (16-25). Liberman et al. reported on subxyphoid approaches for drainage of pericardial effusions (17). Yilmaz et al. reported on the removal of lung specimens via a subxiphoidal port after transthoracic thoracoscopic lobectomy in order to avoid mini-thoracotomy and found that subxiphoid route was an alternative method (29). Suda et al. (21) reported on the use of a single subxiphoid incision for bilateral thoracoscopic wedge resection and found that this technique enables exposure to both lungs through a single incision. Liu et al. (24) described the use of a subxiphoid single-incision thoracoscopic procedure for left upper lobectomy. The subxiphoid approach does not cause intercostal nerve injury and theoretically may result in reduced chest pain intensity. When we compared the perioperative and postoperative outcomes of the three procedures, we found that single-incision subxiphoid thoracoscopic surgery was associated with a longer operative duration than the other two techniques; however, duration of chest tube drainage, length of hospital stay, and rate of postoperative complications were similar among the three groups, indicating that the single subxiphoid approach is a safe and feasible surgical method for pneumothorax.
Surgical techniques that require fewer chest wall incisions reduce the chances of chest wall damage and intercostal nerve compression. In a review article that compared postoperative pain between patients who underwent single-port thoracoscopic surgery and those who received multiport thoracoscopic surgery, Young et al. found inconsistent results on pain intensity after single-port thoracoscopic surgery. The authors concluded that uniport thoracosccopic surgery may have a small clinical effect on reducing postoperative pain during the first 72 h following surgery (30). Jutley et al. compared pain outcomes associated with three-incision and single-incision thoracoscopic surgery for spontaneous pneumothorax and found that the intensity of acute postoperative pain was lower in patients who received the single-incision technique (8). Others studies have provided similar results (9-11). In contrast, Yang et al. found no significant differences in acute operative pain scale scores between patients who underwent a uniport technique and those who received thoracoscopic surgery via a three-port technique for primary spontaneous pneumothorax (13). In the present study, we compared the intensity of acute postoperative pain in patients who received thoracoscopic surgery via a single subxiphoid incision with the intensity of pain in those who underwent thoracoscopic surgery via a single transthoracic incision or three transthoracic incisions and found that patients who received surgery via a single subxiphoid incision had markedly lower pain scale scores during the first 24 hours after surgery than patients who received either of the other two techniques. The reason for the marked difference in postoperative pain intensity can be explained, at least in part, by the fact that the subxiphoid approach avoids injury to the intercostal nerve.
During the subxiphoid approach, we used a sternal retractor to increase the working space, thereby reducing interference caused by the heartbeat. No arrhythmic events occurred in any of the patients during or after surgery. Theoretically, it is possible that lifting of the sternum will induce sternal pain. However, pain was limited to the wound area in all 14 of the patients who received surgery via the single-incision subxiphoid approach. None of the patients reported significant sternal pain. The average and maximum VAS scores in first 24 hours were 0.94±0.32 and 1.64±0.50, respectively. Pain scale scores were significantly lower in patients who received surgery via the subxiphoid approach than in those who received surgery via either of the other two approaches in the first 24 hours after surgery (P<0.0001).
The main limitations of this study are the limited number of patients and its retrospective nature. In addition, exact doses of analgesic agents given to patients were not available for analysis. Furthermore, the intensity of pain was difficult to quantify and could have been influenced by emotion as well as by educational and socioeconomic backgrounds. These confounding factors were not investigated.
In conclusion, single-incision subxiphoid thoracoscopic surgery is associated with significantly lower postoperative pain than transthoracic thoracoscopic approaches and therefore may provide an alternative surgical technique for patients with spontaneous pneumothorax.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Scott WJ, Allen MS, Darling G, et al. Video-assisted thoracic surgery versus open lobectomy for lung cancer: a secondary analysis of data from the American College of Surgeons Oncology Group Z0030 randomized clinical trial. J Thorac Cardiovasc Surg 2010;139:976-81; discussion 981-3. [PubMed]
- Stephens N, Rice D, Correa A, et al. Thoracoscopic lobectomy is associated with improved short-term and equivalent oncological outcomes compared with open lobectomy for clinical Stage I non-small-cell lung cancer: a propensity-matched analysis of 963 cases. Eur J Cardiothorac Surg 2014;46:607-13. [PubMed]
- Paul S, Altorki NK, Sheng S, et al. Thoracoscopic lobectomy is associated with lower morbidity than open lobectomy: a propensity-matched analysis from the STS database. J Thorac Cardiovasc Surg 2010;139:366-78. [PubMed]
- Ceppa DP, Kosinski AS, Berry MF, et al. Thoracoscopic lobectomy has increasing benefit in patients with poor pulmonary function: a Society of Thoracic Surgeons Database analysis. Ann Surg 2012;256:487-93. [PubMed]
- Guden M, Korkmaz AA, Onan B, et al. Subxiphoid versus intercostal chest tubes: comparison of postoperative pain and pulmonary morbidities after coronary artery bypass grafting. Tex Heart Inst J 2012;39:507-12. [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [PubMed]
- Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg 2005;28:43-6. [PubMed]
- Chen PR, Chen CK, Lin YS, et al. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax. J Cardiothorac Surg 2011;6:58. [PubMed]
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [PubMed]
- Chen CH, Lee SY, Chang H, et al. The adequacy of single-incisional thoracoscopic surgery as a first-line endoscopic approach for the management of recurrent primary spontaneous pneumothorax: a retrospective study. J Cardiothorac Surg 2012;7:99. [PubMed]
- Salati M, Brunelli A, Xiumè F, et al. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg 2008;7:63-6. [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [PubMed]
- Sihoe AD, Cheung CS, Lai HK, et al. Incidence of chest wall paresthesia after needlescopic video-assisted thoracic surgery for palmar hyperhidrosis. Eur J Cardiothorac Surg 2005;27:313-9. [PubMed]
- Rogers ML, Duffy JP. Surgical aspects of chronic post-thoracotomy pain. Eur J Cardiothorac Surg 2000;18:711-6. [PubMed]
- Liu YH. Natural orifice transluminal endoscopic surgery: a transtracheal approach for the thoracic cavity in a live canine model. J Thorac Cardiovasc Surg 2011;141:1223-30. [PubMed]
- Liberman M, Labos C, Sampalis JS, et al. Ten-year surgical experience with nontraumatic pericardial effusions: a comparison between the subxyphoid and transthoracic approaches to pericardial window. Arch Surg 2005;140:191-5. [PubMed]
- McGinn JT Jr, Usman S, Lapierre H, et al. Minimally invasive coronary artery bypass grafting: dual-center experience in 450 consecutive patients. Circulation 2009;120:S78-84. [PubMed]
- Watanabe G, Yamaguchi S, Tomiya S, et al. Awake subxyphoid minimally invasive direct coronary artery bypass grafting yielded minimum invasive cardiac surgery for high risk patients. Interact Cardiovasc Thorac Surg 2008;7:910-2. [PubMed]
- Hsu CP, Chuang CY, Hsu NY, et al. Subxiphoid approach for video-assisted thoracoscopic extended thymectomy in treating myasthenia gravis. Interact Cardiovasc Thorac Surg 2002;1:4-8. [PubMed]
- Suda T, Ashikari S, Tochii S, et al. Single-incision subxiphoid approach for bilateral metastasectomy. Ann Thorac Surg 2014;97:718-9. [PubMed]
- Liu YH, Chu Y, Wu YC, et al. Natural orifice surgery in thoracic surgery. J Thorac Dis 2014;6:61-3. [PubMed]
- Chen JT, Liao CP, Chiang HC, et al. Subxiphoid single-incision thoracoscopic bilateral ablative sympathectomy for hyperhidrosis. Interact Cardiovasc Thorac Surg 2015;21:119-20. [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. [PubMed]
- Liu CY, Lin CS, Liu CC. Subxiphoid single-incision thoracoscopic surgery for bilateral primary spontaneous pneumothorax. Wideochir Inne Tech Maloinwazyjne 2015;10:125-8. [PubMed]
- De Conno F, Caraceni A, Gamba A, et al. Pain measurement in cancer patients: a comparison of six methods. Pain 1994;57:161-6. [PubMed]
- Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. [PubMed]
- Passlick B, Born C, Sienel W, et al. Incidence of chronic pain after minimal-invasive surgery for spontaneous pneumothorax. Eur J Cardiothorac Surg 2001;19:355-8; discussion 358-9. [PubMed]
- Yilmaz A, Van Putte BP, Van Boven WJ. Closed chest lobectomy with subxyphoid retraction. Interact Cardiovasc Thorac Surg 2011;13:549-51. [PubMed]
- Young R, McElnay P, Leslie R, et al. Is uniport thoracoscopic surgery less painful than multiple port approaches? Interact Cardiovasc Thorac Surg 2015;20:409-14. [PubMed]


