Corticosteroids in the adjunctive therapy of community-acquired pneumonia: an appraisal of recent meta-analyses of clinical trials
Introduction
Several studies have indicated that community-acquired pneumonia (CAP) is the cause of a high burden of disease in many regions of the world, including the United States of America (USA), Europe, Latin America and the Asia-Pacific region, being associated with a high rate of infection, emerging antibiotic resistance, ongoing mortality, both immediate and long-term, significant impact on health-related quality of life, as well as high medical healthcare costs (1). CAP is a leading cause of death, not only in the USA, but throughout the world (2). The recent Global Burden of Disease Study [2013] indicated that although there has been a reduction in the number of cases worldwide between 1990 and 2013, lower respiratory tract infections still remain a common cause of death and feature as the second most common cause of global years of life lost (3).
With respect to the in-hospital setting, persistently high mortality rates of CAP, which in developed countries have been reported to reach 17% and 27% at 4 weeks and 6 months post-intensive care unit (ICU) admission respectively, present an ongoing challenge (4). Acute respiratory failure, acute cardiovascular events and multiple organ dysfunctions resulting from CAP-associated hyperacute inflammation, represent the major threats (1). Preventing these complications, which are exacerbated, at least in part, by pre-existing, low-grade, chronic inflammatory co-morbidities, and possibly the pro-inflammatory activity of bactericidal antibiotics, is a field of considerable interest and activity. In the case of the former, risk factors include atherosclerosis, type II diabetes/obesity and chronic lung diseases (5). The pro-inflammatory activity of bactericidal antimicrobial agents such as beta-lactams and fluoroquinolones result from bacteriolysis, with accompanying release of cell-wall, cytoplasmic and nuclear components (6). These, in turn, interact with the various types of pathogen recognition receptors present on cells of the innate immune system and structural cells to activate the production of pro-inflammatory cytokines/chemokines, while others lead to activation of the complement cascades. The risk is highest in the setting of a high bacterial load, leading to development of a Jarisch-Herxheimer-like reaction.
Clearly the mainstay of therapy of CAP is the use of antibiotics, which, of necessity, is initially empiric, since the causative organism(s) are not known at the time of initiation of treatment. Much has been written regarding what constitutes appropriate and/or optimal antibiotic treatment, and this has been extensively reviewed elsewhere (1,7-9). However, while it is well recognised that inappropriate initial antibiotic therapy is associated with a worse outcome, it is also noted that even in the setting of appropriate initial antibiotic treatment, many patients still die (10). This has resulted in considerable interest in the potential role of adjunctive, anti-inflammatory therapies in the management of patients with CAP, particularly among the more seriously ill patients (1,7-9,11,12). Shindo and colleagues recently studied risk factors for 30-day mortality in patients with CAP who had received appropriate antibiotic therapy, with the aim of trying to identify patients who were most likely to benefit from adjunctive therapy (10).
Awareness of the threat posed by CAP-associated, inflammation-mediated tissue damage and organ dysfunction, seemingly exacerbated by co-existent co-morbidities, has motivated exploration of the therapeutic potential of adjunctive anti-inflammatory therapies (1,7,9,11,12). Foremost amongst these are corticosteroids (CS) and macrolides (1), with more recent interest in statins and platelet-targeted pharmacological agents (13). While the macrolide group of antibiotics is recommended primarily for their antimicrobial effects, being used in combination with beta-lactam agents in the more seriously ill patients with CAP, there is also considerable evidence that these agents possess beneficial, secondary anti-inflammatory effects directed at both the host and the pathogen (1). More recently, an appreciation of a potential role for statins as adjunctive therapy has also emerged; however, CS are currently amongst the most favoured adjunctive agents, with several clinical trials, as well as systematic reviews and meta-analyses, having been undertaken in the past 2 years. Of the systematic reviews and meta-analyses, one of the most comprehensive was that undertaken by Siemieniuk and colleagues, and is the focus of this current review (14). This is preceded by a brief consideration of the mechanisms of anti-inflammatory activity of CS, the interactions of these agents with macrolide antibiotics, and the potential benefits and risks of short-term administration of CS.
Corticosteroid (CS) mechanisms of anti-inflammatory activity, interactions, benefits and limitations
CS possess broad-spectrum anti-inflammatory activities which target a broad range of immune, inflammatory and structural cells (15,16). The mechanisms underpinning these activities of CS are well documented and are covered only briefly here. These result from the interactions of CS with the cytosolic glucocorticoid receptor-α (15,16). The resultant homodimeric glucocorticoid/glucocorticoid receptor-α complex (GC/GR) undergoes translocation to the cell nucleus where anti-inflammatory activity is achieved by two distinct mechanisms. The first of these, known as trans-repression, is non-genomic and involves recruitment of histone deacetylase-2 to the activated inflammatory gene complex by the GC/GR. This, in turn, results in termination of activation of genes encoding a range of pro-inflammatory proteins. These include cytokines/chemokines such as tumour necrosis factor-α and interleukin-8 (15,16). The second mechanism, known as trans-activation, is achieved via the binding of the GC/GR to GC response elements located in the promoter regions of target genes resulting in the transcription of genes encoding various anti-inflammatory proteins such as IL-10 and the IL-1 receptor antagonist (15,16).
This dual mechanism of CS-mediated anti-inflammatory activity targeting many cell types, with the possible exception of neutrophils (17), clearly underscores the potential of these agents in the adjunctive therapy of CAP.
Corticosteroid (CS)/macrolide interactions
In many of the studies designed to assess the adjunctive utility of CS in patients with CAP, a seemingly under-appreciated aspect is the interactions of these agents with macrolide antibiotics. In this context, it is well established that several macrolides inhibit the activity of cytochrome P450 3A4 (CYP3A4), a xenobiotic-metabolising enzyme, which is induced by, and also eliminates various types of CS (18-20). The most commonly used macrolides in the treatment of severe CAP, clarithromycin, erythromycin and azithromycin do, however, vary with respect to their inhibitory effects on CYP3A4, and are classified as strong, moderate and weak inhibitors, respectively (19). Metabolism of methylprednisolone, used in many clinical trials of severe CAP, appears to be particularly responsive to the inhibitory effects of clarithromycin on CYP3A4, while metabolism of prednisone is apparently unaffected (21). Furthermore, another property of macrolides which needs to be considered in the setting of CS adjunctive therapy of CAP is the suppressive effects of these agents on neutrophils, cells which are apparently insensitive to the direct anti-inflammatory actions of CS (17,22,23). Therefore, although the current literature is limited, the influence of concomitant macrolide administration, whether beneficial, detrimental or negligible, on CS metabolism, may be an issue which requires serious consideration when evaluating the outcome of most clinical trials investigating the role of adjuvant CS in severe CAP.
Potential benefits and limitations of short-term administration of corticosteroids (CS) in CAP
The stringent systematic review and meta-analysis reported by Siemieniuk et al., complemented by very recent clinical trials and additional meta-analyses expanded on below, largely support the contention that short-term adjunctive CS therapy is associated with a shorter time to clinical stability and decreased duration of hospitalisation in CAP patients overall, with the potential for a decrease in mortality in those with severe infection (14). The difficulties in interpreting the data emanating from the various studies and systematic reviews originate from the inherent differences in the characteristics of the individual investigations. These include study type (e.g., retrospective versus prospective vs. observational), patient inclusion (e.g., all CAP vs. severe CAP) and exclusion (e.g., excluding immunocompromised patients and/or specific pathogens in some studies) criteria and differences in study end-points, as well as the specific CS agent, route, dose, and duration used. The strengths of the meta-analysis by Siemieniuk et al. include the rigorous search for the included studies, the inclusion of numerous end-points, and the authors’ stringent attention to heterogeneity and bias in the data, as well as their reporting of the quality/certainty of the evidence for CS benefits and risks (14).
Notwithstanding uncertainty in respect of optimum type, dosage, route and duration of administration, Prina et al. in their recent review mention that clinically insignificant hyperglycemia was the only evident side-effect noted in several randomised clinical trials of CS in CAP (9). The authors cautioned, however, the need for awareness of the potential threat of superinfection (9), while other risks, albeit very infrequent, include gastrointestinal (GIT) bleeding, osteonecrosis, severe mood changes and psychotic reactions, as well as fatal varicella-zoster in immunocompetent persons (24,25). In addition, CS use is contra-indicated in the setting of Influenza A H1N1 pneumonia and should be used with extreme caution, or not at all, in the presence of certain medical conditions, such as insulin-requiring diabetes mellitus (26).
Although of unproven significance in the setting of severe CAP, the apparent resistance of neutrophils to the anti-inflammatory actions of steroids also represents a potential limitation of these agents. These include prolongation of the lifespan of neutrophils via steroid-mediated inhibition of apoptosis (22), as well as progressive loss of GR function during sustained activation of these cells (23). Given the suppressive effects of macrolides on neutrophil reactivity, future studies of adjunctive CS therapy should consider adjusting for specific antibiotic therapy when assessing outcomes.
The Siemieniuk systematic review and meta-analysis
Siemieniuk and colleagues undertook a comprehensive systematic review and meta-analysis of all randomised controlled trials (RCTs) that had been undertaken evaluating the use of adjunctive systemic CS in adults hospitalised with CAP (14). At the time of their study, a Cochrane systematic review and meta-analysis, with similar inclusion criteria, had been published in 2011, which had included all CAP studies undertaken up to December 2010 (27). Siemieniuk and colleagues used the same search strategy of that review for the extraction of additional studies in MEDLINE, MBASE and the Cochrane register of controlled trials for the period 1 January 2010 to 24 May 2015 and also reviewed the reference lists of all the existing studies and reviews, together with all articles on Google Scholar that had cited the included studies (14). The authors extracted data of all potential benefits and also harms of adjunctive CS therapy, the latter including the occurrence of hyperglycemia requiring treatment, GIT haemorrhage, neuropsychiatric symptoms and need for rehospitalisation. The authors used a stringent definition of severe CAP, if possible, using the following scoring systems in preferential order: the Pneumonia Severity Index (PSI), the CURB—65 score, the American Thoracic Society criteria or the British Thoracic Society criteria. If objective scoring was not possible, the classification of severe CAP as described by the authors of the individual studies was used. Siemieniuk and colleagues were meticulous in their handling of the data, using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system to evaluate the quality/certainty of evidence. They also used a Cochrane instrument to assess the risk of bias in the individual studies, with publication bias assessed by inspection of funnel plots. Various tests for heterogeneity of the studies were also applied. In total, the authors evaluated 13 RCTs, encompassing 2,005 patients, including additional studies which followed the previous Cochrane review.
The main findings were as follows. In the studies that assessed mortality, there were 52/977 (5.3%) deaths in the CS group vs. 79/997 (7.9%) deaths in the control group (RR =0.67; 95% CI, 0.45–1.01). The effects on mortality varied according to CAP severity, being significant in the severe group (RR =0.39; 95% CI, 0.20–0.77), but not in the non-severe group (RR =1.0; 95% CI, 0.79–1.26). Other positive endpoints in the CS group were a reduction in need for mechanical ventilation (MV) (RR =0.45; 95% CI, 0.26–0.79), which was greater in studies enrolling less severely ill cases, a reduction in acute respiratory distress syndrome (ARDS) (RR =0.24; 95% CI, 0.10–0.56), a decrease in time to clinical stability [mean difference (MD), −1.22 days; 95% CI, −2.08 to −0.35 days] and a decrease in the duration of hospitalisation (MD, −1.00 days; 95% CI, −1.79 to −0.21 days). The only significant adverse event was the occurrence of hyperglycemia requiring treatment (RR =1.49; 95% CI, 1.01–2.19).
The final assessment was that CS use was associated with a lower mortality (moderate quality evidence), which was only significant in the group of patients with severe CAP; however, there was a significant reduction in the need for MV (moderate quality evidence), in the occurrence of ARDS (moderate quality evidence), in the time to clinical stability (high quality evidence) and in the duration of hospitalisation (high quality evidence). Hyperglycaemia requiring treatment occurred significantly more frequently in the CS group (high quality of evidence).
The major advantages of this analysis were the rigorous searches by the authors that elicited studies that had not been included previously, and their meticulous assessment of bias, heterogeneity and quality of data, providing estimates of uncertainty for each endpoint or conclusion.
One of the major issues highlighted by the authors that they have indicated as a limitation of their study is that the included investigations varied considerably with regard to the type of CS used, the dose and the route of administration (14). Thus even though the evidence for benefit of CS use in this systematic review and meta-analysis appeared with moderate-to-high certainly, the study is unable to recommend an optimal agent or dose for CS therapy.
A number of additional studies, as well as systematic reviews and meta-analyses were published before and after the Siemieniuk paper and to a large extent they came to similar conclusions and are reviewed in some detail below.
Review of other recent meta-analyses
After Siemieniuk
Marti and colleagues undertook a systematic review and meta-analysis of RCTs comparing adjunctive CS and antibiotic therapy with antibiotics alone in adult patients with CAP of any severity (28). British and American Thoracic Society criteria were used to define CAP. The primary outcome measure used was 30-day mortality. Secondary outcomes evaluated were length of hospital stay, time to clinical stability, need for vasopressors or MV and severe complications (need for MV or vasopressors). Adverse events evaluated were hyperglycemia and in-hospital GIT bleeding. A total of 14 trials were included which had enrolled 2,077 patients. There was no difference in mortality when comparing the cases that had received adjunctive CS vs. those that had not (RR =0.84; 95% CI, 0.55–1.29). However, adjunctive CS therapy was associated with a lower risk of severe complications (RR =0.36; 95% CI, 0.23–0.56), a shorter length of hospital stay [9 days (95% CI, 7.6–10.7) vs. 10.6 days (95% CI, 7.4–15.3)] and a shorter time to clinical stability [3.3 days (95% CI, 2.8–4.1) vs. 4.3 days (95% CI, 3.6–5.1)]. The risk of hyperglycemia was higher in the CS group (RR =1.59; 95% CI, 1.06–2.38), while there was no difference in occurrence of GIT bleeding between the two groups. Subgroup analysis documented a mortality benefit in patients with severe CAP (RR =0.47; 95% CI, 0.23–0.96).
The final assessment was that use of CS did not result in a lower mortality overall, but was associated with a lower mortality in the sub-group of severe CAP; CS use was, however, associated with a decrease in severe complications, in the length of hospital stay and time to clinical stability. There was an increased risk of hyperglycemia in the CS group.
Horita and colleagues undertook a systematic review and meta-analysis of original RCTs, written as full articles in English, which evaluated the use of adjunctive CS in addition to antibiotic therapy targeting both typical and atypical pathogens in hospitalised adults with CAP (29). Use of any type, dose, or duration of CS was considered acceptable. Articles focusing on immunocompromised patients or “specified pathogens” (not defined further) were excluded. All the articles analysed were required to include data on at least one of the following outcomes: mortality [expressed as an odds ratio (OR)], length of ICU stay, length of hospital stay, and time to clinical stability [in the form of a hazard ratio (HR) or as mean difference]. The study eventually evaluated 10 RCTs encompassing 1,780 patients. The main findings in the CS group were that the pooled OR for all-cause death was 0.80 (95% CI, 0.53–1.21), being 0.41 (95% CI, 0.19–0.90) in the subgroup of severe cases, and 0.21 (95% CI, 0.0–0.74) in the subgroup of ICU cases. Furthermore, the length of ICU stay was −1.30 days (95% CI, −3.04 to −0.44), length of hospital stay −0.98 days (95% CI, −1.26 to −0.71), and time to clinical stability −1.16 days (95% CI, −1.73 to −0.58). While some studies had reported on adverse events, the data were not considered suitable for meta-analysis due to differences in the described methodology. In general, the authors indicated that while there may have been an increased risk of CS-related adverse events and hyperglycaemia, there did not appear to be a risk of serious adverse events.
The final assessment was that the use of CS was associated with a significantly lower mortality only in patients with severe CAP, while in the CAP patients overall there was a shorter length of hospital stay and shorter time to clinical stability. There appeared to be no increased risk for severe adverse events in the CS group.
Chen and colleagues undertook a systematic review and meta-analysis of RCTs of adult patients (>18 years) with CAP, diagnosed according to the China and American Thoracic Society CAP guidelines who had been treated in the emergency room or in hospital (30). Studies which included HIV-infected patients with CAP were excluded, as were studies with incomplete or inaccurate information. The cases treated with CS and conventional antibiotics were compared to the group receiving antibiotics alone. The endpoints evaluated were mortality, length of hospital stay, length of ICU stay, as well as the occurrence of adverse events including superinfection, upper GIT bleeding and hyperglycaemia. Seven RCTs encompassing a total of 944 patients were evaluated further. No differences in mortality (RR =0.77; 95% CI, 0.46–1.27; Z=1.03; P=0.30), or length of ICU stay [weighted mean difference (WMD), 1.17; 95% CI, 1.68–4.02; Z=0.81; P=0.42) were evident. However, the mean length of hospital stay was shorter in the CS group (WMD, −1.70; 95% CI, −2.01 to −1.39; Z=10.81; P<0.00001). With regard to adverse events, there were no significant differences noted in the occurrence of superinfection, upper GIT bleed or hyperglycemia when comparing the CS vs. the standard treatment group.
The final assessment was that use of CS was associated with a shorter length of hospital stay, but had no impact on mortality. There were no differences in the adverse events when comparing the two groups of patients.
Wan and colleagues undertook a systematic review and meta-analysis of RCTs of adult patients with CAP (31). Studies comparing treatment vs. placebo or no agent which had the endpoints of mortality rate, either in-patient or 28-day mortality, were evaluated in the analysis. The secondary endpoints included adverse events including superinfection, hyperglycaemia, GIT bleeding and empyema. Observational cohort studies were included to confirm the results of the RCTs with studies published as abstracts included in the sensitivity analysis. Overall, there were nine eligible RCTs, as well as six cohort studies, encompassing 1,667 and 4,095 patients respectively. The main findings were that CS use in CAP patients overall (RR =0.72; 95% CI, 0.43–1.21) and in severely ill cases (RR =0.72; 95% CI, 0.43–1.21) was not associated with a significant reduction in mortality. Neither was there a reduction in mortality in severely ill cases in the cohort studies (RR =1.00; 95% CI, 0.86–1.17). There was, however, a significant decrease in the risk of ARDS (RR =0.21; 95% CI, 0.08–0.59). Because of the way the data were reported, a combined analysis of the other endpoints was not possible, but there was a tendency for CS use to be associated with a shorter time to clinical stability, and duration of intravenous (IV) antibiotic therapy, as well as a reduced length of hospital and ICU stay. The use of CS was not associated with any adverse events, such as superinfection, hyperglycaemia, GIT bleeding, or empyema.
The final assessment was that CS use had no impact on mortality, either overall, or in the severely ill cases, but there was a decrease in the risk of ARDS. Although analysis was not possible, there was a suggestion that CS use may reduce length of hospital and ICU stay, time to clinical stability, and duration of IV antibiotic therapy. CS use was not associated with an increase in adverse events (The key findings of these meta-analyses are summarised in Table 1).
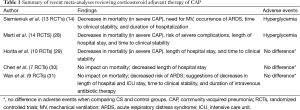
Full table
Before Siemieniuk
Cheng and colleagues undertook a systematic review of RCTs in adult patients with severe CAP (32). Studies were included if CS were used as adjunctive therapy and compared with placebo, defined as normal saline solution or a drug with similar appearance to that of the CS. Studies in abstract form or lacking original data were excluded. The primary endpoint was in-hospital mortality, or, if that was unavailable, mortality at the longest follow-up time. Secondary outcomes were length of hospital and ICU stay, duration of MV, days off MV and adverse events. Four RCTs enrolling patients with severe CAP were included. Use of CS was found to be associated with a significant reduction in hospital mortality vs. the control group (Peto OR =0.39; 95% CI, 0.17–0.90). There was a trend from the RCTs towards reduction in the secondary endpoints and no significant difference in adverse events.
The final assessment was that CS use was associated with a reduced mortality in adults with severe CAP, with an indication of a possible reduction in ICU and hospital length of stay, and duration of MV, and increased days off MV, with no difference in adverse events when compared with the control group.
Review of recent clinical studies
Before Siemieniuk
Blum and colleagues conducted a multicentre, randomised, double-blind, placebo-controlled trial in hospitalised adult patients (>18 years) with CAP (defined as previously described), who were randomly assigned to receive prednisone 50 mg daily for 7 days, or placebo (33). The primary study endpoint was time to clinical stability which was defined as the time taken to achieve stable vital signs for at least 25 h. There were multiple secondary endpoints, including all-cause mortality. Ultimately, 785 patients were assigned, 392 to the CS group and 393 to the placebo limb. The median time to clinical stability was significantly shorter in the CS compared with the placebo group [3.0 days (IQR, 2.5–3.4) vs. 4.4 days (IQR, 4.0–5.0); HR =1.33; 95% CI, 1.15–1.50; P<0.0001]. There was no difference in pneumonia-related complications when comparing the two groups, but the CS group had more in-hospital hyperglycemia requiring insulin therapy [76 (19%) vs. 43 (11%); OR =1.96; 95% CI, 1.31–2.93; P=0.0010]. All-cause 30-day mortality was not different between the two treatment groups.
Torres and colleagues conducted a multicentre, randomised, double-blind, placebo-controlled trial in adult patients (>18 years) with severe CAP and, what they described as a high inflammatory response [defined as a C-reactive protein (CRP) level >150 mg/L] (34). The primary outcome was treatment failure, a composite outcome of early treatment failure based on clinical deterioration, need for subsequent MV, death within 72 h of treatment, or a composite outcome of late treatment failure based on radiographic progression, persistent respiratory failure, development of shock, subsequent need for MV, death 72 h after treatment initiation or a composite of both early and late treatment failure. In-hospital mortality was a secondary outcome. Adverse events were also evaluated. Treatment failure was significantly less common in the CS versus the placebo group [8 patients (13%) vs. 18 patients (31%); P=0.02]. The risk of treatment failure was lower in the CS group (OR =0.34; 95% CI, 0.14–0.87; P=0.02). There was no difference in the in-hospital mortality when comparing the CS and placebo groups [6 patients (10%) vs. 9 patients (15%); P=0.37], and no significant difference in the occurrence of hyperglycemia [11 patients (18%) vs. 7 patients (12%); P=0.34].
After Siemieniuk
Tagami and colleagues undertook a retrospective record review of adult patients (≥18 years) with severe CAP, requiring MV, who had received catecholamines (for septic shock) (35). Patients were divided into two groups based on whether they had received CS (n=631) or not (n=1,893). Of interest in the CS group was the inclusion of cases that received “low-dose” CS defined as IV infusion of methylprednisolone 0.5–2.5 mg/kg per day (or equivalent doses for other CS), while those who had received high-dose CS were excluded. The primary outcome measure was 28-day mortality. In the 2,524 cases that had received catecholamines [2,524] the 28-day mortality was significantly lower in the CS vs. the placebo group (unmatched; 24.6% vs. 36.3%; P<0.001; propensity matched: 25.3% vs. 32.6%, P=0.01; inverse-probability weighted: 27.5% vs. 34.2%; P<0.001). There was no difference in 28-day mortality when comparing the CS and placebo groups in cases who had not received catecholamines (n=4,410).
Major ongoing studies
A number of clinical trials which may address some of the questions that have arisen from previous investigations are currently recruiting cases.
The Extended Steroids in CAPe (ESCAPEe) study aims to document whether early treatment with methylprednisolone compared to placebo improves survival in critically ill adult patients (≥18 years) with CAP (36). There are a number of patient exclusion criteria. The treatment duration chosen is 20 days, including 7 days of full dose CS, followed by a slow reduction in dose over 13 days. The CS dose chosen is an initial bolus dose on randomisation, followed by 40 mg/day for the first 7 days, 20 mg/day for the next 7 days and 6 days of tapering doses (12 mg/day and then 4 mg/day). It will be noted whether patients required MV at the time of treatment assignment. Patients will otherwise receive standard of care according to guidelines. Patients will be followed for 180 days, with the primary outcome measure being 60-day all-cause mortality. A number of secondary endpoints have been chosen which, among others, includes in-hospital morbidity-mortality, ventilator-free days, multiple organ dysfunction syndrome-free days, length of ICU and hospital stay, and post-hospital morbidity-mortality. Mortality will be followed up to 1 year.
The second study, the Santeon-CAP study (37), is a multicentre study planning to recruit 600 hospitalised patients with CAP. There are certain predefined sub-group analyses planned. The study will compare the use of dexamethasone administered at a dose of 6 mg by mouth daily for 4 days, compared to placebo. The primary outcome measures are length of hospital stay. Secondary endpoints include, among others, mortality, disease severity and inflammatory indices.
A related study, albeit not focused specifically on CAP, is the ADRENAL study (38), which aims to document whether patients admitted to the ICU with septic shock have a better outcome when given hydrocortisone compared to placebo. The study aims to recruit 3,800 participants with septic shock who will receive a continuous IV infusion of hydrocortisone at a dose of 200 mg daily for 7 days versus placebo while in ICU. The primary outcome measure is mortality at 90 days after randomisation and there are a number of secondary outcomes.
Commentaries/editorial comments on the various studies
Several commentaries, focused on the meta-analysis by Siemieniuk et al. (14), as well as the trials reported by Torres et al. (34), Tagami et al. (35) and Blum et al. (33) have accompanied or followed publication. These commentaries, although generally positive, do not, however, reflect concordance with respect to the role of CS in the adjuvant therapy of CAP.
Restrepo et al., commenting on the report by Siemieniuk et al. (14), expressed the opinion that “this meta-analysis supports the use of systemic CS therapy” in patients with severe CAP (39); however, they also highlighted the difficulty in defining what constitutes “severe CAP”. While patients requiring MV and/or vasopressor support are an obvious target group, the authors proposed that the use of biomarkers such as CRP may help in identifying those patients who do not have these clinical characteristics, but who nevertheless may also benefit from CS therapy.
While commending Torres et al. (34) on their attempts to identify a category of patients likely to benefit most from CS (those with the highest systemic inflammatory indices), Wunderink expressed some reservations about the study, including the relatively low percentages of patients in both the CS and control group who had received concomitant macrolide therapy, the 8-year period required for recruitment, and the relatively short time of CS administration (only 5 days) (40). Wunderink noted that the major difference between the two groups with regard to “treatment failure” was less radiographic progression in the CS treatment group, possibly due to attenuation of a Jarisch-Herxheimer-like reaction, necessitating confirmation in larger studies (40). While conceding the limitations identified by Wunderink (40), Torres and Ferrer in their commentary conclude that in the presence of a high systemic inflammatory response and the absence of influenza pneumonia or significant medical contra-indications for CS “that CS are useful in severe CAP and can help decrease treatment failure and probably mortality” (26). The authors indicated that although CS were used in their study patients for only 5 days, with abrupt cessation, there was no rebound of the inflammatory markers at day 7.
Ricard and Messika in their commentary on the study reported by Tagami et al. (35), while noting some limitations of this study, indicated that the study clearly indicated that patients with severe CAP and associated shock are most likely to benefit from adjunctive CS therapy as opposed to those without shock (41). As proposed by Torres et al., this is likely to be the sub-group of patients with the highest inflammatory indices (34).
Commenting on the clinical trial reported by Blum et al. (33), Annane in his largely complimentary review, in which he noted the favourable benefit-risk ratio associated with CS therapy, also raised several issues for future investigation, including likely CS therapy benefit in outpatients and ICU cases with CAP, as well as the potential for long-term benefits of CS (42). Baskar et al., commenting on the same trial, raised several interpretational issues, stating that “additional high quality studies with a clinical event as the primary end-point are needed before rallying for any change in clinical practice” (43).
In terms of future research, several strategies which may clarify the adjunctive therapeutic potential of CS in CAP are shown in Table 2.

Full table
Conclusions
The meta-analysis by Siemieniuk and colleagues documented that adjunctive CS use in patients with CAP is associated with a shorter time to clinical stability and a shorter length of hospital stay, as well as a possible mortality benefit in those with severe CAP, a contention which is largely supported by additional recent studies and meta-analyses (14). Although clarity is still required as to which specific subgroups of CAP would benefit most from adjunctive CS, those with severe CAP, those with the highest inflammatory biomarker indices, such as CRP levels greater than 150 mg/L, and those with shock requiring vasopressor support, appear to experience greatest benefit, as suggested by the meta-analyses and by several of the investigators (14,35,44).
Acknowledgements
C Feldman is supported by the National Research Foundation of South Africa.
Footnote
Provenance: This is an invited article commissioned by the Section Editor Wan-Jie Gu (Department of Anesthesiology, Affiliated Drum Tower Hospital, Medical College of Nanjing University, Nanjing, China).
Conflicts of Interest: C Feldman has acted on the advisory board and/or received honoraria for lectures from pharmaceutical companies manufacturing and/or marketing macrolide antibiotics. R Anderson has no conflicts of interest to declare.
References
- Steel HC, Cockeran R, Anderson R, et al. Overview of community-acquired pneumonia and the role of inflammatory mechanisms in the immunopathogenesis of severe pneumococcal disease. Mediators Inflamm 2013;2013:490346.
- Wunderink RG. CAP death: what goes wrong when everything is right? Lancet Infect Dis 2015;15:995-6. [Crossref] [PubMed]
- GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117-71. [Crossref] [PubMed]
- Walden AP, Clarke GM, McKechnie S, et al. Patients with community acquired pneumonia admitted to European intensive care units: an epidemiological survey of the GenOSept cohort. Crit Care 2014;18:R58. [Crossref] [PubMed]
- Millett ER, De Stavola BL, Quint JK, et al. Risk factors for hospital admission in the 28 days following a community-acquired pneumonia diagnosis in older adults, and their contribution to increasing hospitalisation rates over time: a cohort study. BMJ Open 2015;5:e008737. [Crossref] [PubMed]
- Karlström A, Boyd KL, English BK, et al. Treatment with protein synthesis inhibitors improves outcomes of secondary bacterial pneumonia after influenza. J Infect Dis 2009;199:311-9. [Crossref] [PubMed]
- Liapikou A, Torres A. Current treatment of community-acquired pneumonia. Expert Opin Pharmacother 2013;14:1319-32. [Crossref] [PubMed]
- Musher DM, Thorner AR. Community-acquired pneumonia. N Engl J Med 2014;371:1619-28. [Crossref] [PubMed]
- Prina E, Ranzani OT, Torres A. Community-acquired pneumonia. Lancet 2015;386:1097-108. [Crossref] [PubMed]
- Shindo Y, Ito R, Kobayashi D, et al. Risk factors for 30-day mortality in patients with pneumonia who receive appropriate initial antibiotics: an observational cohort study. Lancet Infect Dis 2015;15:1055-65. [Crossref] [PubMed]
- Meijvis SC, van de Garde EM, Rijkers GT, et al. Treatment with anti-inflammatory drugs in community-acquired pneumonia. J Intern Med 2012;272:25-35. [Crossref] [PubMed]
- Sibila O, Ferrer M, Agustí C, et al. Corticosteroids as adjunctive treatment in community-acquired pneumonia. Minerva Anestesiol 2014;80:1336-44. [PubMed]
- Feldman C, Anderson R. Community-acquired pneumonia: pathogenesis of acute cardiac events and potential adjunctive therapies. Chest 2015;148:523-32. [Crossref] [PubMed]
- Siemieniuk RA, Meade MO, Alonso-Coello P, et al. Corticosteroid therapy for patients hospitalized with community-acquired pneumonia: a systematic review and meta-analysis. Ann Intern Med 2015;163:519-28. [Crossref] [PubMed]
- Barnes PJ. Glucocorticosteroids: current and future directions. Br J Pharmacol 2011;163:29-43. [Crossref] [PubMed]
- Cruz-Topete D, Cidlowski JA. One hormone, two actions: anti- and pro-inflammatory effects of glucocorticoids. Neuroimmunomodulation 2015;22:20-32. [Crossref] [PubMed]
- Tintinger GR, Anderson R, Feldman C. Pharmacological approaches to regulate neutrophil activity. Semin Immunopathol 2013;35:395-409. [Crossref] [PubMed]
- Westphal JF. Macrolide - induced clinically relevant drug interactions with cytochrome P-450A (CYP) 3A4: an update focused on clarithromycin, azithromycin and dirithromycin. Br J Clin Pharmacol 2000;50:285-95. [Crossref] [PubMed]
- Common medications classified as weak, moderate and strong inhibitors of CYP3A4. Available online: http://www.ebmconsult.com/articles/medications-inhibitors-cyp3a4-enzyme
- Matoulková P, Pávek P, Malý J, et al. Cytochrome P450 enzyme regulation by glucocorticoids and consequences in terms of drug interaction. Expert Opin Drug Metab Toxicol 2014;10:425-35. [Crossref] [PubMed]
- Fost DA, Leung DY, Martin RJ, et al. Inhibition of methylprednisolone elimination in the presence of clarithromycin therapy. J Allergy Clin Immunol 1999;103:1031-5. [Crossref] [PubMed]
- Saffar AS, Dragon S, Ezzati P, et al. Phosphatidylinositol 3-kinase and p38 mitogen-activated protein kinase regulate induction of Mcl-1 and survival in glucocorticoid-treated human neutrophils. J Allergy Clin Immunol 2008;121:492-498.e10.
- Bergquist M, Jirholt P, Nurkkala M, et al. Glucocorticoid receptor function is decreased in neutrophils during endotoxic shock. J Infect 2014;69:113-22. [Crossref] [PubMed]
- Dilisio MF. Osteonecrosis following short-term, low-dose oral corticosteroids: a population-based study of 24 million patients. Orthopedics 2014;37:e631-6. [Crossref] [PubMed]
- Richards RN. Side effects of short-term oral corticosteroids. J Cutan Med Surg 2008;12:77-81. [Crossref] [PubMed]
- Torres A, Ferrer M. What's new in severe community-acquired pneumonia? Corticosteroids as adjunctive treatment to antibiotics. Intensive Care Med 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Chen Y, Li K, Pu H, et al. Corticosteroids for pneumonia. Cochrane Database Syst Rev 2011.CD007720. [PubMed]
- Marti C, Grosgurin O, Harbarth S, et al. Adjunctive corticotherapy for community acquired pneumonia: a systematic review and meta-analysis. PLoS One 2015;10:e0144032. [Crossref] [PubMed]
- Horita N, Otsuka T, Haranaga S, et al. Adjunctive Systemic Corticosteroids for Hospitalized Community-Acquired Pneumonia: Systematic Review and Meta-Analysis 2015 Update. Sci Rep 2015;5:14061. [Crossref] [PubMed]
- Chen LP, Chen JH, Chen Y, et al. Efficacy and safety of glucocorticoids in the treatment of community-acquired pneumonia: A meta-analysis of randomized controlled trials. World J Emerg Med 2015;6:172-8. [Crossref] [PubMed]
- Wan YD, Sun TW, Liu ZQ, et al. Efficacy and safety of corticosteroids for community-acquired pneumonia: a systematic review and meta-analysis. Chest 2016;149:209-19. [Crossref] [PubMed]
- Cheng M, Pan ZY, Yang J, et al. Corticosteroid therapy for severe community-acquired pneumonia: a meta-analysis. Respir Care 2014;59:557-63. [Crossref] [PubMed]
- Blum CA, Nigro N, Briel M, et al. Adjunct prednisone therapy for patients with community-acquired pneumonia: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet 2015;385:1511-8. [Crossref] [PubMed]
- Torres A, Sibila O, Ferrer M, et al. Effect of corticosteroids on treatment failure among hospitalized patients with severe community-acquired pneumonia and high inflammatory response: a randomized clinical trial. JAMA 2015;313:677-86. [Crossref] [PubMed]
- Tagami T, Matsui H, Horiguchi H, et al. Low-dose corticosteroid use and mortality in severe community-acquired pneumonia patients. Eur Respir J 2015;45:463-72. [Crossref] [PubMed]
- Extended Steroid in CAP(e) (ESCAPe). Available online: https://clinicaltrials.gov/ct2/show/NCT01283009
- Santeon-CAP; Dexamethasone in Community-acquired Pneumonia. Available online: https://clinicaltrials.gov/ct2/show/NCT01743755
- ADjunctive coRticosteroid trEatment iN criticAlly ilL Patients With Septic Shock (ADRENAL). Available online: https://clinicaltrials.gov/ct2/show/NCT01448109
- Restrepo MI, Anzueto A, Torres A. Corticosteroids for Severe Community-Acquired Pneumonia: Time to Change Clinical Practice. Ann Intern Med 2015;163:560-1. [Crossref] [PubMed]
- Wunderink RG. Corticosteroids for severe community-acquired pneumonia: not for everyone. JAMA 2015;313:673-4. [Crossref] [PubMed]
- Ricard JD, Messika J. Low-dose corticosteroids during severe community-acquired pneumonia: end of the story. Eur Respir J 2015;45:305-7. [Crossref] [PubMed]
- Annane D. Corticosteroids and pneumonia: time to change practice. Lancet 2015;385:1484-5. [Crossref] [PubMed]
- Baskar V, Sum CF, Lim SC. Prednisone for community-acquired pneumonia: not yet time. Lancet 2015;386:431. [Crossref] [PubMed]
- Siemieniuk RA, Guyatt GH. Corticosteroids in the treatment of community-acquired pneumonia: an evidence summary. Pol Arch Med Wewn 2015;125:570-5. [PubMed]


