Left upper lobectomy and systematic lymph nodes dissection in enlarged pulmonary hilar lymph nodes in primary lung cancer patient by uniportal video-assisted thoracic surgery
Introduction
Video-assisted thoracic surgery (VATS) lobectomy has evolved rapidly in the last two decades and usually includes a 3 to 5 cm utility incision and 2 or 3 other ports. Compared with thoractomy, VATS has advantages, such as less postoperative pain, faster recovery, fewer complications and shorter hospital stays (1,2).
Improved technology and experience in VATS anatomical lung resection made fewer and smaller incisions feasible for major pulmonary resection. Some approaches reported the technique of 2 ports to perform lobectomy and segmentectomy comprehensively (3) and Gonzalez-Rivas’s group described their first experience of single-port thoracoscopic lobectomy in June 2010 (4). Recently, they published a series of 102 uniportal video-assisted thoracoscopic lobectomies with satisfied results (5). Since then uniportal VATS became an increasingly popular approach with reduced trauma, shorter recovery time and better cosmesis. Uniportal VATS anatomical pulmonary resection, with only one small incision for all surgery instruments and camera manuplation, requires higher operative skill, especially in the situation of enlarged hilar lymph nodes. Here we present a technical procedure for left upper lobectomy and systematic lymph node dissection with enlarged pulmonary hilar lymph nodes by uniportal VATS.
Case presentation
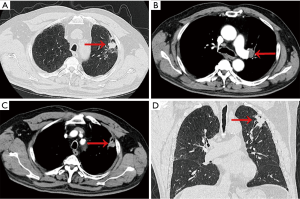
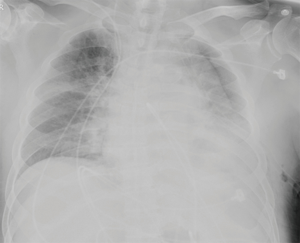
A 67-year-old male had found a nodule in the left upper lobe for 2 months, a history of coronary disease and hypertension was dictated. He had smoked about 40 cigarettes per day for 45 years. He had chronic obstructive pulmonary disease (COPD) with mild obstructive and restrictive ventilation pulmonary dysfunction and moderate diffusion pulmonary disfunction (FEV1 of 2.06 L, 68.7% of the predicted value, MVV of 71.62 L, 63.1% of predicted value, DLCO 4.87 mmoL/min/kPa, 55.7% of predicted value) on pre-operation evaluation. A preoperative chest computed tomography (CT) revealed a nodule in the left upper lobe, with enlarged hilar lymph nodes and emphysema. Fiberoptic bronchoscopy showed no abnormalities, the pathological results of the 4L & 4R station lymph nodes EBUS-TBNA were negative (Figure 1). Preoperative pathological examination of the lung lesion obtained by CT-guided percutaneous transthoracic needle biopsy indicated a poorly differentiated squamous cell carcinoma. The patient had coronary heart disease and the coronary artery DSA indicated 50% stenosis in left anterior descending (LAD). Left upper pulmonary lobectomy was performed. The operation took 171 minutes. During the operation, the estimated blood loss was 100 mL. On postoperative day (POD) 1, the amount of fluid drainage was 350 mL, and chest X-ray showed satisfied left lung inflation (Figure 2). The chest tube was removed on POD 4. The patient was discharged on POD 6 without complications. The tumor size was 4 cm in diameter, and the postoperative pathology confirmed lymph metastasis in station 5, 11 and 13. Four cycles of adjuvant chemotherapy and radiotherapy were followed.
Operative techniques
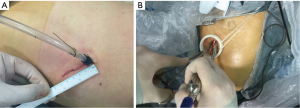
Operative position, insicion and instruments: the uniportal insicion were performed between the anterior axillary line and posterior axillary line over the fourth intercostal space about 4 cm in length (Figure 3A). No rib spreader was used. A disposable, plastic wound retractor was used to stretch and protect the incision (Figure 1B). A 30-degree, 10-mm high definition camera thoracoscope was placed at the posterior part of the incision during operation time for a panoramic view. To relieve the camera-man’s hand tiredness, the thoracoscope bounded by a tape was fixed to the surgical drape (Figure 3B). Both the surgeon and the camera-man stood in front of the patient and shared the same vision. For a better exposure, another assistant may be needed to retract the lung and he/she stood posteriorly. The unipotal VATS uses the same instruments as the conventional 3-port VATS dose (Figure 4). During dissection, we held a curving suction (Panther Healthcare, China) in left hand and an electrocautery hook or an ultra-sonic scalpel in the right hand.

Operative key points and procedure (Figure 5)
- Mobilization of pulmonary vessels. The patient’s interlobar fissure was complete. First we dissected the pulmonary artery in the interlobar fissure with ultrasonic scalpel or electrocautery hook and stapled the lingular atrey with a vascular (white cartridge, 45-mm-long) endostapler (EndoGIA, Covidien, USA). Then we dissected the interlobar lymph nodes (station 11). After the dissection of inter lobar fissure, the mediastinal pleura of the upper and anterior hilum was separated to isolate the anterior and apical segmental pulmonary arteries. With enlarged hilar lymph nodes, the isolation of anterior and apical segmental arteries was difficult. So we isolated the posterior ascending atery and ligated it. The first branch of the superior vein was ligated and divided to dissect the enlarged lymph nodes. After dissecting the adhesion between the lymph nodes and superior vein, the superior vein was cut off. Then the adhesions among the lymph nodes and anterior and apical segmental pulmonary arteries were dissected carefully with electrocautery hook, the arteries were ligated and divided;
- Division of the bronchus. After dissection of the vessels and interlobar fissure, the left upper lobar bronchus could be isolated easily and divided by green cartridge (60-mm-long) endostapler. The upper lobe was placed in a specimen bag and removed. The frozen pathology comfired an negative bronchus margin;
- Dissection of mediastinal lymph nodes. Opened the superior mediastinal pleura, the stations 5 and 6 nodes were dissected with caution of the phrenic nerve and the left innominate vein injury. The station 4 lymph nodes were dissected using a combination of blunt and sharp dissection technique, with special care to exposure and preserve the left recurrent laryngeal nerve. Then we divided the inferior pulmonary ligament and dissected station 9 lymph nodes. The ring forceps was applied to pull the left lower lung forwards to exposure the posterior mediastinum. First we dissected along the posterior aspect of subcarinal lymph nodes, and the small vessels between esophagus and lymph nodes were cauterized with electrocautery hook. Then we completely dissected along the anterior of subcarinal nodes by electrocautery hook and ultrasonic scalpel, and the lymph node station 7 was completely removed. To facilitate the exposure during subcarnial lymph nodes dissection in the left side, a right-sided double-lumen intubation was used;
- Check the air leak. The thorax lavage was performed with distilled water, and the lung was inflated to rule out the air leak of the bronchial stump and the lung.
Comments
VATS lobectomy was first reported in 1992 (7,8). In 20 years, VATS lobectomy has become a popular approach for thoracic disease. Three to four incisions were usually performed.
Rocco and colleagues first described the uniportal VATS pulmonary resections in 2004 (9). Since then uniportal had been performed as a diagnostic and therapeutic procedure for lung lesions. In 2010, Gonzalez-Rivas’s group reported the world’s first uniportal VATS lobectomy, a milestone approach.
It is certain that operating through fewer and smaller surgical incisions will be popular if the procedure can be safely performed with satisfied outcomes. For major pulmonary resection, the uniportal VATS involved only one intercostal space, thus the trauma is less. Meanwhile, no trocar insertion could minimize the risk of intercostal nerve injury; while combined with the relevant nerve block the postoperative pain could be effectively reduced. Comparing with the 3-port VATS, uniportal VATS provides completely different geometric visions. In fact, the view of unipotal VATS is the same as that in open surgery. Three-port VATS requires the surgeons to adapt to an unnatural vision which is discordant with hand coordination. The uniportal VATS approach requires the translation of thoracoscope instruments 90° along a sagittal plane, which brings a vertical, caudo-cranial perspective for the operative instruments and the target lesion. The surgeon accustomed to open thoracic surgery could shorten the learning period of uniportal VATS (10).
In China, some lung cancer cases accompanied with enlarged hilar lymph nodes, would increase operation difficulties. In this patient, similar situation was encountered. Considering the thoractomy could induce severe postoperative complains and delay recover, we decided to apply uniportal VATS lobectomy. Because of enlarged lymph nodes, there was not enough space to insert the endostapler, especially in dissecting the apico-anterior pulmonary arteries. So we ligated the apico-anterior pulmonary arteries.
Uniportal VATS anatomical pulmonary resection, with only one small incision used for all instruments and camera, requires higher operative skill. According to our experience, 100 cases experience of conventional 3-port VATS lobectomy are needed before the usage of unipotal VATS. It is better if the surgeon has the training experience of double port VATS lobectomy. The surgeon could also directly adopt UVATS, as we did. An experienced cameraman is crucial for a successful uniportal VATS major pulmonary resection. To effectively relieve the arm fatigue of the cameraman, we bind a tape to the thoracoscope at the posterior part of the incision.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [Crossref] [PubMed]
- Salati M, Brunelli A, Xiumè F, et al. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg 2008;7:63-6. [Crossref] [PubMed]
- Onaitis MW, Petersen RP, Balderson SS, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg 2006;244:420-5. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fieira E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Fan JQ, Yao J, Chang ZB, et al. Left upper lobectomy and systematic lymph nodes dissection in enlarged pulmonary hilar lymph nodes in primary lung cancer patient by uniportal video-assisted thoracic surgery. Asvide 2016;3:338. Available online: http://www.asvide.com/articles/1107
- Landreneau RJ, Mack MJ, Hazelrigg SR, et al. Video-assisted thoracic surgery: basic technical concepts and intercostal approach strategies. Ann Thorac Surg 1992;54:800-7. [Crossref] [PubMed]
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Bertolaccini L, Rocco G, Viti A, et al. Geometrical characteristics of uniportal VATS. J Thorac Dis 2013;5 Suppl 3:S214-6. [PubMed]