Symptomatic pericardial schwannoma treated with video-assisted thoracic surgery: a case report
Introduction
Neurogenic tumors of the mediastinum consist of 19%–39% of all the mediastinal tumors, of which benign schwannoma is the most common. It is asymptomatic in the majority of cases (1); however, signs of nerve compression can occasionally occur, and, although rare, there have been cases of malignant transformation. The specific diagnosis of mediastinal tumors still relies on the final pathological result, although preoperative imaging such as computed tomography (CT) and magnetic resonance imaging (MRI) can provide some information. Currently, a complete surgical resection is the mainstay of the treatment, with excellent prognosis. The immunohistochemical examination shows that schwannoma is made up of fascicles of spindle cells different from neurofibroma. The tumor is positive for S-100 protein and calretinin (2). Based on its nature, schwannoma should have an anatomical relationship with nerve structures (3). In the present case, the tumor was resected using video-assisted thoracoscopic surgery (VATS), and there were no postoperative complications and recurrence.
Case presentation
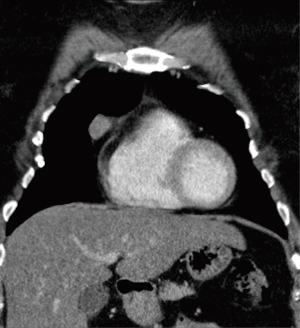
A 48-year-old Taiwanese female was hospitalized due to a deteriorating bronchial asthma, progressive chest tightness, and dyspnea on exertion. Posteroanterior chest radiography revealed a widened mediastinum and cardiomegaly. A contrast-enhanced CT of the chest revealed a well-defined, homogeneous soft-tissue nodule at the right heart border with mild intracardiac extension, measuring 2.5 cm (axial view) × 2.6 cm (coronal view) (Figure 1). The tumor was located just adjacent to the pericardium of the right atrium, and was distinct from the lung parenchyma. No significant enhancement and no calcification of tumor were noticed after contrast medium administration. Physical examination of the heart and chest was unremarkable, and no lymphadenopathy was found in the neck or axillary regions.
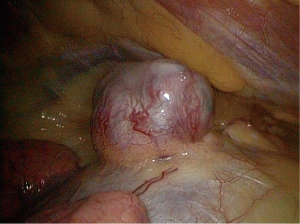
A complete surgical resection of the tumor was performed by VATS. Intraoperatively, the tumor was smooth, grey-pink in color, well encapsulated, and firm in consistency with abundant vascularity (Figure 2). The tumor had no identifiable stalk and protruded from the pericardium of the right atrium without any involvement or invasion of the surrounding tissue, such as the right phrenic nerve. The resected surface of the tumor showed a heterogeneous yellow and white appearance with focal hemorrhage.
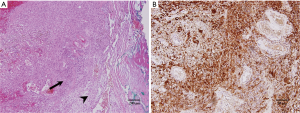
On histopathological examination, the tumor was characterized as a well-encapsulated mass composed of spindle cells, with alternative hyper- and hypo-cellularity of the mediastinal tissue regions (Figure 3A). In addition, numerous hyalinized vessels were also observed. Immunohistochemical staining showed that tumor cells were strongly positive for S-100 protein (Figure 3B). The diagnosis of a pericardial schwannoma was made according to the final pathological result. There was no recurrence over a one-year follow-up.
Discussion
Schwannomas are benign neoplasms arising from the Schwann cells and may develop in any part of the body. They are mostly found in the head, neck, and flexor aspects of the limbs, although they may also be present within the thorax, mostly in the posterior mediastinum, originating from the sympathetic chain, intercostal nerves, spinal nerve roots, or vagus nerve. It is very rare for schwannomas to be localized in the middle mediastinum; moreover, very few cases of schwannoma arising from the pericardium have been reported. Zhang et al. (4) reported the first case of a benign pericardial schwannoma, located in the pretracheal space and aortopulmonary window with compression effect. In this case, the tumor was resected subsequently via thoracotomy. The case also emphasized the importance of image differential diagnosis for pericardial tumors. Imaging of schwannoma usually reveals a characteristic smooth, well-defined margin, and an ovoid or spherical shape. Our case presented with a widening mediastinum on plain film radiography of the chest, and CT revealed a homogeneous solitary protruding mass without cystic changes or calcification. The approximate size, location, possible internal content, and relationship with the surrounding structures for a given tumor can be determined by a CT; however, it cannot be differentiated whether the tumor is benign or malignant, which can lead to life-threatening conditions, such as pericardial effusion and decompensated heart failure (5). Hence, further surgical intervention is required.
Complete resection of the tumor remains the standard procedure for benign mediastinal schwannoma, and has an excellent prognosis without the need for an adjuvant therapy. We used VATS in this case, since the tumor had no complicated association with the neighboring structures, and showed no signs of an advanced invasion of the adjacent cardiac walls. However, had the tumor been malignant, an advanced thoracotomy may have been more appropriate to ensure a wider safety margin.
Because schwannomas arise within the nerve sheath, there should be an association between the tumor and its nerve of origin. Regarding cardiac and intrapericardial schwannoma, we believe that such tumors arise from the cardiac branches of the vagus nerve or the cardiac plexus. Gleason et al. (6) reported the first identified case of a primary cardiac schwannoma in 1972. This particular tumor was a 1.5-cm encapsulated nodule within the wall of the right atrium, with typical histologic features of neural origin. Since then, limited cases of intrapericardial schwannoma (with or without symptoms) have been reported (7-11), all of them being benign. Two of these were located in the left atrium, one in the right ventricle, and another two in the right atrium of the heart, near the cardiac plexus. In our patient, the tumor protruded from the lateral aspect of the right atrium without gross involvement of the nerve; however, based on its anatomical location, we postulate that this tumor might have originated from the cardiac branch of the vagus nerve.
In conclusion, pericardial schwannoma is benign but sometime complicated with life-threatening condition. We believe that VATS is an effective therapeutic choice for such pericardial tumors, as it achieves complete removal and pathological diagnosis simultaneously.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Marchevsky AM. Mediastinal tumors of peripheral nervous system origin. Semin Diagn Pathol 1999;16:65-78. [PubMed]
- Fine SW, McClain SA, Li M. Immunohistochemical staining for calretinin is useful for differentiating schwannomas from neurofibromas. Am J Clin Pathol 2004;122:552-9. [Crossref] [PubMed]
- Pilavaki M, Chourmouzi D, Kiziridou A, et al. Imaging of peripheral nerve sheath tumors with pathologic correlation: pictorial review. Eur J Radiol 2004;52:229-39. [Crossref] [PubMed]
- Zhang XH, Wang Y, Quan XY, et al. Benign pericardial schwannoma in a Chinese woman: a case report. BMC Cardiovasc Disord 2013;13:45. [Crossref] [PubMed]
- D'Amato N, Correale M, Ireva R, et al. A rare cause of acute heart failure: malignant schwannoma of the pericardium. Congest Heart Fail 2010;16:82-4. [Crossref] [PubMed]
- Gleason TH, Dillard DH, Gould VE. Cardiac neurilemoma. N Y State J Med 1972;72:2435-6. [PubMed]
- Hashimoto T, Eguchi S, Nakayama T, et al. Successful removal of massive cardiac neurilemoma with cardiopulmonary bypass. Ann Thorac Surg 1998;66:553-5. [Crossref] [PubMed]
- Rausche T, El-Mokthari NE, Krüger D, et al. Benign mediastinal schwannoma: cardiac considerations - case report and a short review of the literature. Clin Res Cardiol 2006;95:422-4. [Crossref] [PubMed]
- Early SA, McGuinness J, Galvin J, et al. Asymptomatic schwannoma of the heart. J Cardiothorac Surg 2007;2:1. [Crossref] [PubMed]
- Chung JH, Jung JS, Lee SH, et al. Resection of Intrapericardial Schwannoma Co-Existing with Thymic Follicular Hyperplasia through Sternotomy without Cardiopulmonary Bypass. Korean J Thorac Cardiovasc Surg 2014;47:298-301. [Crossref] [PubMed]
- Hwang SK, Jung SH. Schwannoma of the heart. Korean J Thorac Cardiovasc Surg 2014;47:141-4. [Crossref] [PubMed]


