An uncommon presentation of Kikuchi-Fujimoto disease as mediastinal lymphadenopathy
Introduction
Histiocytic necrotizing lymphadenitis, so-called Kikuchi-Fujimoto disease (KFD), is a relatively rare self-limiting cervical lymphadenopathy primarily affecting young women (1,2). A number of possible etiologies have been proposed, including infection (Epstein-Barr virus, cytomegalovirus, influenza, adenovirus and toxoplasma), T cell-mediated immune response, and HLA class II gene involvement; however, the detailed pathogenesis of KFD has not been elucidated to date (3). Here we report a rare case of KFD with a unique presentation of isolated mediastinal lymphadenopathy without cervical lymph node swelling in senior age, mimicking a malignant disease or tuberculous lymphadenitis.
Case presentation
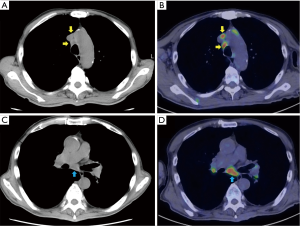
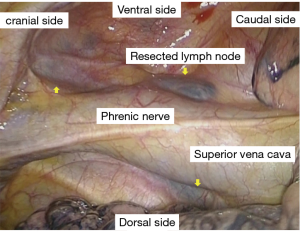
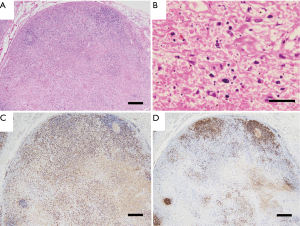
A 69-year-old male patient was admitted to our hospital with fever of unknown origin. His medical history included peripheral neuropathy probably due to alcoholism. He had no prior history of treatment for malignant or infectious disease. He was suffering from high fever, general malaise for approximately 6 months, and gradually worsening appetite loss complicated by severe body weight loss (10 kg in 6 months). Laboratory findings showed slight elevation of serum lactose dehydrogenase to 453 IU/L (normal range, 106–211 IU/L) and soluble interleukin 2 receptor to 1,595 U/mL (normal range, 122–496 U/mL). Computed tomography (CT) showed massive multiple mediastinal lymphadenopathy, and 18F-fluorodeoxyglucose-positron emission tomography (FDG-PET) also indicated high standardized uptake value (SUV) in the same lesion (Figure 1). Considering the patient’s age and poor general condition, malignant diseases including malignant lymphoma and metastatic carcinoma of unknown origin or tuberculous lymphadenitis were strongly suspected, and sarcoidosis and other atypical infections including cat scratch disease and hemophagocytic syndrome were considered as possible differential diagnoses. For a definitive diagnosis and determination of appropriate treatment, video-assisted thoracic surgery for mediastinal lymph node biopsy was performed. The lymph nodes were macroscopically black and stony hard, and two right anterior mediastinal lymph nodes were resected without trouble (Figure 2). Histological examination revealed massive necrosis and some lymphoid follicles, without giant and epithelioid cell invasion; however, no malignant cells of any type could be ascertained (Figure 3). Bacteriological examination also revealed no causative agents including tuberculosis. The definitive diagnosis proved to be histiocytic necrotizing lymphadenitis, or KFD. Due to the patient’s severely impaired general condition, intravenous steroid (methylprednisolone 0.5 mg/kg/day) was administered and getting better gradually. Changing it to oral medication, he was discharged at 3 weeks after the surgery.
Discussion
Histiocytic necrotizing lymphadenitis, or KFD, was first reported by two Japanese pathologists in 1972 and is generally characterized by uncommon self-limiting cervical lymphadenopathy with intermittent high fever, primarily in younger females (1,2). KFD is typically diagnosed based on cervical lymphadenopathy with or without histological examination in patients with a mean age of 30 (range, 11–75) years and self-limiting good clinical outcome; however, some long-lasting, severe cases (approximately 30% of total) are treated with steroid administration (4,5). Clinically, some cases may involve recurrence (3–4%) and subsequent complications of systemic lupus erythematosus, Sjögren’s syndrome, and adult Still’s disease (4). Isolated mediastinal lymphadenopathy without cervical lymph node swelling is very rare in KFD, with only two younger cases ever reported (6,7). Furthermore, this is the oldest case report which was firstly diagnosed as KFD. Although the patient had a rare presentation, the advanced age of the patient and the rare presentation as a mediastinal rather than cervical lymphadenopathy might be related.
In developing countries, prolonged fever and cervical lymphadenopathy are characteristic of tuberculosis infection, which is a major differential diagnosis of KFD, and empirical therapy for tuberculosis is often performed in clinical practice (6). By contrast, in developed countries, KFD is often misdiagnosed as lymphoma, sarcoidosis, infectious mononucleosis, cat scratch disease, some collagen diseases, drug eruption, and other disorders. With the growing prevalence of CT in developed countries including Japan, not only cervical lymphadenopathy but also mediastinal and abdominal lymphadenopathies could be detected through investigation for fever of undetermined origin. More latent KFD patients even of senior age might be overlooked and enter spontaneous remission without a detailed examination. In the present case, since the origin of fever was thought to be mediastinal lymphadenopathy and the patient’s condition was very poor, a definitive histological diagnosis could be obtained to determine treatment. We should consider KFD as a differential diagnosis for even senior patients with high fever and cervical and/or mediastinal lymphadenopathy.
As a state-of-the-art diagnostic tool, endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is often applied for the minimally invasive biopsy of mediastinal lymphadenopathy complicated by primary lung cancer. However, although EBUS-TBNA has become a useful diagnostic procedure for mediastinal lymphadenopathy, it is insufficient for the diagnosis of lymphoma (8) since the small sample volume is inadequate for histological examination including immunohistochemical staining and genetic examination. Since malignant lymphoma or sarcoidosis was considered the main differential diagnoses for the present case, we performed thoracoscopic biopsy to obtain a sample of sufficient size for immunohistochemical staining. Surgical biopsy as well as EBUS should be considered when histological diagnosis for mediastinal lymphadenopathy is demanded for definite diagnosis and appropriate therapy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Kikuchi M. Lymphadenitis showing focal reticulum cell hyperplasia with nuclear debris and phagocytosis. Nippon Ketsueki Gakkai Zasshi 1972;35:378-380.
- Fujimoto Y, Koizumi Y, Yamaguchi K. Cervical subacute necrotizing lymphadenitis: a new clinicopathologic entity. Naika 1972;30:920-7.
- Bosch X, Guilabert A, Miquel R, et al. Enigmatic Kikuchi-Fujimoto disease: a comprehensive review. Am J Clin Pathol 2004;122:141-52. [Crossref] [PubMed]
- Kucukardali Y, Solmazgul E, Kunter E, et al. Kikuchi-Fujimoto Disease: analysis of 244 cases. Clin Rheumatol 2007;26:50-4. [Crossref] [PubMed]
- Dorfman RF, Berry GJ. Kikuchi's histiocytic necrotizing lymphadenitis: an analysis of 108 cases with emphasis on differential diagnosis. Semin Diagn Pathol 1988;5:329-45. [PubMed]
- Gupta P, Lau K, West K, et al. Kikuchi-Fujimoto disease masquerading as tuberculosis. Gen Thorac Cardiovasc Surg 2014;62:125-7. [Crossref] [PubMed]
- Yoshida Y, Matsuzawa Y, Rikitake H, et al. Mediastinal lymphadenopathy without cervical lymphadenopathy in a case of Kikuchi-Fujimoto disease. Intern Med 2011;50:649-52. [Crossref] [PubMed]
- Varela-Lema L, Fernández-Villar A, Ruano-Ravina A. Effectiveness and safety of endobronchial ultrasound-transbronchial needle aspiration: a systematic review. Eur Respir J 2009;33:1156-64. [Crossref] [PubMed]


