A multi-center evaluation of a powered surgical stapler in video-assisted thoracoscopic lung resection procedures in China
Introduction
Lung cancer is the leading cause of cancer death in China and worldwide, with non-small cell lung cancer (NSCLC) being the most prevalent subtype (1). Currently, surgery is still the mainstay of treatment for NSCLC, particularly for early-stage NSCLC. Surgical treatment of lung cancer can be performed by thoracotomy, video-assisted thoracoscopic surgery (VATS), or robotic approaches. Adoption of VATS has significantly increased since the first procedure performed more than 20 years ago (2). Advantages of the VATS include: decreased chest tube duration, fewer complications, shorter hospital stay, and improved patient reported outcomes, including earlier return to full preoperative activities and less post-operative pain (3-7).
Stapling devices are important tools widely used in VATS surgeries with a low incidence of staple associated complications (5,8). Prolonged air leak (PAL) is a common complication after pulmonary resection and is associated with increased hospital length of stay (LOS) after lung resection surgery (9). Estimates for PAL in VATS procedures generally range from 10–15% (9-11).
This clinical trial assessed the use of a powered stapler in VATS lung resection. The primary study endpoint was occurrence and duration of air leak and PAL. Procedure details and perioperative outcomes associated with VATS lung resections were also evaluated, including degree of articulation, cartridge selection, and how differences in these aspects might affect intra-operative performance and post-operative outcomes.
Methods
Data reported is from a single arm, multi-center, prospective study in Chinese patients scheduled for wedge resection or lobectomy (www.clinicaltrials.gov identifier NCT02338583). The study was sized with the intent of controlling the margin of error for the 95% confidence interval of PAL air leak to less than or equal to 5%.
Following institutional review board approval at each participating site, patients ≥18 years who met study entry criteria, scheduled for VATS wedge resection or lobectomy, and provided informed consent were enrolled in this study. VATS technique was defined as the use of a video thoracoscope without rib spreading and monitor-based dissection. Indications for surgery included any diagnostic VATS wedge resection or lobectomy for suspected NSCLC (up to and including stage II using AJCC 7th Edition Lung Cancer Staging criteria). Procedures were limited to a single lobe; diagnostic VATS wedge resections that immediately preceded VATS lobectomy were also included. The use of robotic assistance or staple line buttress was excluded. Patients providing informed consent were required to meet the following inclusion criteria for participation: ECOG status 0–1; American Society of Anesthesiologists (ASA) physical status classification ≤3; and no prior history of lung surgery. Individuals were excluded for active bacterial or fungal infections; systemic administration of steroids within 30 days prior to study procedure; or chemotherapy/radiation therapy for cancer within 30 days prior to the procedure. The study utilized the Echelon FlexTM Powered ENDOPATH® Stapler (Ethicon, Cincinnati, USA) along with compatible cartridges: gray (closed staple height, 0.75 mm), white (1.0 mm), blue (1.5 mm), gold (1.8 mm), green (2.0 mm), and black (2.3 mm). Procedures were performed according to institution standard of care between 26 November 2014 and 01 April 2015.
Intra-operative data collected included procedure duration; method of ligation/transection for bronchus, major vessels, and lung parenchyma; staple line interventions; blood loss; and device usage (articulation, cartridge use, and study device usability).
At the end of each surgery, a chest tube was placed to evacuate fluid and/or air from the pleural cavity and help re-establish normal intrathoracic physiology. All sites observed and treated air leak via a water seal chest drainage device per standard of care. Air leaks were qualitatively evaluated and described twice daily by a single surgeon. The observer would first observe the water seal during the patient’s spontaneous respirations. The patient was then asked to cough forcefully 3 to 5 times. If an air leak occurred, bubbling in the water seal chamber would be present and described as expiratory, inspiratory, continuous (both expiratory and inspiratory) or forced expiratory (cough). PALs were defined as those lasting longer than 5 days. Patients were followed post-operatively for approximately 4 weeks.
Post-operative data collected included air leak assessments, chest tube duration, hospital course, and adverse events (AEs). Data were collected using a centralized electronic data capture system and routinely monitored throughout the study.
Categorical variables were reported as counts and percentages; continuous variables were reported as mean, standard deviation, median, minimum, and maximum. The incidence rate of postoperative air leaks was estimated with 95% confidence intervals using the exact binomial method of Clopper and Pearson.
Results
A total of 100 consecutive patients were enrolled (procedure initiated) across four centers in China. Three patients were excluded from the final analysis due to conversion to open surgery. Three additional patients were excluded for protocol exclusions [segmentectomy (2) and mediastinal tumor resection]. There were 94 procedures included in the final analysis: 15 wedge resections, 74 lobectomies, and five wedge resections followed by lobectomy.
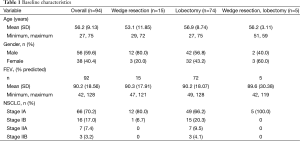
The study cohort included 56 (59.6%) men and 38 (40.4%) women with a mean (SD) age of 56.2 (9.13) years. All patients were Asian; baseline characteristics of the patients are summarized in Table 1. Of the 92 patients diagnosed with NSCLC, 89.1% had TNM stage I disease. Percent-predicted FEV1 scores averaged 90.2% (18.6%). Less than half (39.4%) of the patients (5.3% women, 62.5% men) were smokers; none had a medical history of emphysema or chronic obstructive pulmonary disease (COPD).
Full table
Operative details are shown in Table 2. Mean ± SD time for wedge resections (1.1±0.5 h), was less than half of the time for lobectomies (2.4±1.0 h). Mean blood loss was 53.9 mL (range, 0–400 mL). An intra-operative air leak test was performed in 89 procedures and no intra-operative leakage was reported.
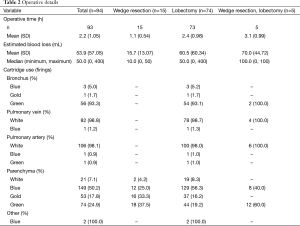
Full table
Sites were generally consistent relative to cartridge use. The white cartridge was used for all but two pulmonary artery transections (98.1%), and all but one pulmonary vein transections (98.8%). Cartridge selection was variable for parenchyma transection, with the green cartridge used most frequently for wedge resections (37.5%) and the blue cartridge most frequently in lobectomies (56.3%). Gold and white cartridges were also utilized for parenchymal transections. The green cartridge was used most often for bronchus transections (93.3%).
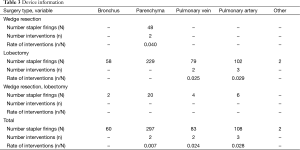
Surgical interventions required after stapler firings were recorded for all tissue types transected. In summary, there were no interventions required for bronchus transection out of 60 firings recorded. Six patients required cautery for seven occurrences of bleeding out of 550 total stapler firings (1.3%) on parenchyma and vasculature. Among them, two (0.7%) were reported on parenchyma (297 firings). Both parenchymal interventions occurred during wedge resection procedures when the green cartridges were used. Cautery for bleeding was applied during two occurrences of pulmonary vein transection (2.4%) and three occurrences of pulmonary artery transection (2.4%). All vessel interventions occurred when the white cartridges were used.
Device-specific data presented in Table 3 includes articulation and surgeon satisfaction with the usability of the device. There were 66 procedures in which articulation of staplers were applied. Articulation was described by the surgeons as “making the procedure easier” in 98.5% and “essential” in 83.3% of the firings. This increased to 100% for wedge resection procedures or wedge resection followed by lobectomy. Angle range of the device was reported as sufficient in 86.8% of the firings. Surgeons were also asked to complete a satisfaction questionnaire to rate usability of the study device on a scale of 1.0 (very unsatisfied) to 10.0 (very satisfied). The average (SD) usability satisfaction score was 9.0 (1.2).
Full table
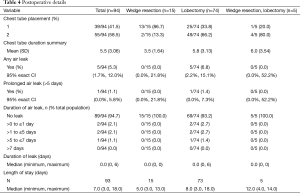
Post-operative information, provided in Table 4, includes chest tube placement and occurrences of air leak. A single chest tube was placed for most wedge resection procedures (86.7%) while two chest tubes were more frequently placed during lobectomies (67.1%). As the study investigators did not have access to a chest drainage system with an air leak monitor, air leak assessments were performed qualitatively. Post-operative air leak occurred in five (5.3%) patients (lobectomies). PAL occurred in one (1.1%) patient who had a lobectomy and single chest tube. The duration was reported as 6 days. For this study, LOS was defined as the duration of postoperative hospitalization. Median LOS was 7.0 days (range, 3–18 days).
Full table
All patients enrolled who had a study procedure (n=100) were followed for safety. AEs after surgery, summarized in Table 5 as subject count per event, were reported regardless of the relationship to the study device or procedure. Apart from air leaks, which are reported separately, a total of 31 AEs were reported in 25 (25.0%) patients. Most events were respiratory in nature, with cough reported most frequently (nine patients).
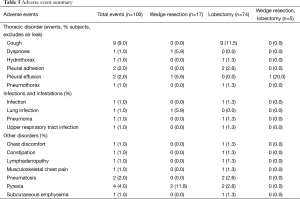
Full table
Discussion
In this study of VATS wedge resection or lobectomy performed with powered staplers, we analyzed the intra-operative performance and post-operative complications related to the device. Using powered staplers, VATS wedge resections and lobectomies were completed in 1.1±0.5 and 2.4±1.0 h (mean ± SD), respectively, with an average blood loss of 53.9 mL. No intra-operative air leakage was found. The incidence of surgical interventions (cautery) needed after stapler firing was 1.3%. There was a 5.3% incidence of post-operative air leak, and one (1.1%) case of PAL among the 94 patients enrolled, all following lobectomies, which is comparable with the studies of Chinese patients receiving lung resections (12-15).
Surgeon choice of cartridge for tissue transection with the study endocutter was generally consistent across sites. Based on the study results, it appears that most surgeons were matching cartridge to tissue type for vasculature, parenchyma, and bronchus. Surgeons participating in the study were generally satisfied with the articulation and overall usability of the stapler, reporting that it made the VATS surgery easier and sometimes essential. The study endocutter and reloads were consistently reliable across transections.
Limitations of this study include the lack of a comparison control stapler. Also, while this study is of moderate size (94 VATS procedures), it is not sufficient to perform predictive modeling for relevant factors of PAL.
Conclusions
The use of powered staplers in this study achieved intra- and post-operative patient outcomes comparable to those previously reported. VATS technique, including cartridge selection to tissue type, was also consistent. In addition, the articulation of the powered stapler makes the procedure easier for the surgeons.
Acknowledgements
This work was supported by Ethicon, a Johnson & Johnson company.
Footnote
Conflicts of Interest: Dr. Edmund Kassis, Susan Knippenberg and Michael Schwiers are employed by Ethicon. Tengfei Yang is employed by Johnson & Johnson Medical (Shanghai) Ltd. The other authors have no conflicts of interest to declare.
References
- He J, Gu D, Wu X, et al. Major causes of death among men and women in China. N Engl J Med 2005;353:1124-34. [Crossref] [PubMed]
- Levi JF, Kleinmann P, Riquet M, et al. Percutaneous parietal pleurectomy for recurrent spontaneous pneumothorax. Lancet 1990;336:1577-8. [Crossref] [PubMed]
- Yang X, Wang S, Qu J. Video-assisted thoracic surgery (VATS) compares favorably with thoracotomy for the treatment of lung cancer: a five-year outcome comparison. World J Surg 2009;33:1857-61. [Crossref] [PubMed]
- Swanson SJ, Herndon JE 2nd, D'Amico TA, et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802--a prospective, multi-institution feasibility study. J Clin Oncol 2007;25:4993-7. [Crossref] [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Whitson BA, Groth SS, Duval SJ, et al. Surgery for early-stage non-small cell lung cancer: a systematic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg 2008;86:2008-16; discussion 2016-8.
- Cao C, Manganas C, Ang SC, et al. A meta-analysis of unmatched and matched patients comparing video-assisted thoracoscopic lobectomy and conventional open lobectomy. Ann Cardiothorac Surg 2012;1:16-23. [PubMed]
- Gossot D, Merlusca G, Tudor A, et al. Pitfalls related to the use of endostaplers during video-assisted thoracic surgery. Surg Endosc 2009;23:189-92. [Crossref] [PubMed]
- Liang S, Ivanovic J, Gilbert S, et al. Quantifying the incidence and impact of postoperative prolonged alveolar air leak after pulmonary resection. J Thorac Cardiovasc Surg 2013;145:948-54. [Crossref] [PubMed]
- Cerfolio RJ, Bass CS, Pask AH, et al. Predictors and treatment of persistent air leaks. Ann Thorac Surg 2002;73:1727-30; discussion 1730-1.
- Brunelli A, Monteverde M, Borri A, et al. Predictors of prolonged air leak after pulmonary lobectomy. Ann Thorac Surg 2004;77:1205-10; discussion 1210. [Crossref] [PubMed]
- Dong Q, Cui J, Zhang K, et al. Video assisted Thoracoscopic Small incision Surgery for Lung Metastasis of Breast Cancer. Chin J Min Inv Surg 2012;12:47-9.
- Tan QY, Deng B, Kang PM, et al. Perioperative outcomes of complete video-assisted thoracoscopic lobectomy for early stage non-small cell lung cancer via single utility port. J Third Mil Med Univ 2012;34:2181-3.
- Huang J, Zhao X, Lin H, et al. Treatment of Non-small Cell Lung Cancer by Single-direction Four-hole Complete Video-assisted Thoracoscopic Lobectomy. Chin J Clin Thorac Cardiovasc 2012;19:125-9.
- Xie H, Ni B, Ma HT, et al. Uniportal video-assisted thoracoscopic surgery for radical resection of lung cancer: a report of 93 cases. Chin J Minim Invasive Surg 2014;14:529-30.


