Single-port thoracoscopic surgery for pneumothorax under two-lung ventilation with carbon dioxide insufflation
Introduction
A pneumothorax is a collection of air in the pleural space between the lung and chest wall. Primary spontaneous pneumothorax is a common disease that usually occurs in tall, thin young men as a result of the rupture of emphysematous subpleural bullae or blebs in the apical lung (1,2). The goal of surgical therapy is to reduce the likelihood of a recurrence, which can exceed 50% if not managed appropriately (3). Video-assisted thoracoscopic surgery (VATS) is the preferred surgical method of resecting bullae or blebs and creating a pleurodesis (4,5).
Recently, the surgical technique for VATS has evolved into single incisional thoracoscopic surgery (SITS) performed through 2- to 3-cm incisions (6,7). In addition, some groups, including ours, reported on the feasibility and safety of SITS for minor to major lung resection in benign or malignant thoracic disease (8-11). The potential benefits of SITS in thoracic surgery reportedly include reduced intercostal pain (12,13), reduced surgical trauma (14), and surgeon hand-eye coordination similar to that of open thoracotomy (15). The single-port approach also promises improved ergonomics through the development of SITS endoscopic devices and their combination with robotics (16).
Despite recent improvements in surgical technique, one-lung ventilation anesthesia (OLVA) is still indicated in most thoracic surgeries and can be performed with double-lumen endotracheal intubation or with bronchial blockers through single lumen endotracheal intubation (17). During VATS for pneumothorax, OLVA is used for the identification and resection of bullous lesions in a non-ventilated state since bullae are most commonly treated with endoscopic stapling. Many physiological disadvantages of OLVA have been reported including overventilation of a non-collapsed lung resulting in a postoperative ventilation/perfusion mismatch, hypoxemia, sputum retention, consolidation, and edema in the operative lung (18,19). Moreover, fiberoptic bronchoscopy is essential for confirming the proper location of the endotracheal tube or blocker (20). These OLVA-related problems can be minimized with adequate intraoperative management and postoperative care. However, even minor adverse events after VATS for pneumothorax in patients with poor pulmonary function and lung manipulation during surgery can increase postoperative lung problems such as pulmonary edema or atelectasis, resulting in prolonged hospital stays (21).
Since 2007, we have been using a two-lung ventilation anesthesia (TLVA) strategy with low tidal volume during VATS for pneumothorax (22). We previously reported that TLVA was cost-effective and time-saving compared with OLVA (23). In 2009, we started performing SITS for pneumothorax under TLVA with carbon dioxide (CO2) gas insufflation using a special multiple-access single port (SILSTM port, Covidien, Mansfield, MA). The SILS port has multiple channels including a three-way stopcock for gas infusion, which enabled the performance of SITS under TLVA with gas infusion to achieve acceptable surgical views. To our knowledge, there are no reports on SITS under TLVA. This was the first study to evaluate the feasibility and safety of SITS performed using a SILS port under TLVA with CO2 gas insufflation for pneumothorax.
Methods
Patients
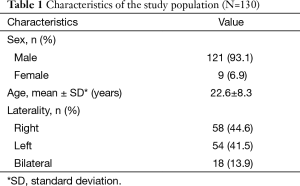
A consecutive series of 130 patients with primary spontaneous pneumothorax underwent single-port thoracoscopic bleb resection using a SILS port under TLVA with CO2 gas insufflation between February 2009 and May 2014 at our institution. The study was approved by our institution’s Ethics Committee, and written informed consent was obtained from all patients in accordance with the Declaration of Helsinki (institutional review board no. KUGH14263-001). Initially, all patients were managed with a tube thoracostomy. Chest computed tomography was performed to identify subpleural bullae or blebs. Our hospital’s surgical indications were reported previously (22). Patients with a first episode of bullae or blebs on chest computed tomography, combined hemothorax, an air leak lasting more than 5 days, an unexpanded lung, bilateral pneumothorax, tension pneumothorax, or recurrent attack were included in our study. Patients with secondary pneumothorax with severely emphysematous lungs or pneumothorax caused by traumatic injury and moderate-to-severe adhesions on computed tomography scans were excluded (Table 1).
Full table
Anesthesia
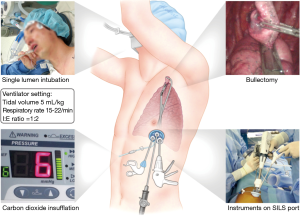
The TLVA protocol used during single-port surgery was the same as that described in our previous report (24). After general anesthesia induction, patients were intubated with a single-lumen endotracheal tube (Sheridan/CF Tracheal Tubes, ID 7.0 for women and ID 8.0 for men; Hudson RCI, Durham, NC) and ventilated with a volume of 10 mL/kg, a respiratory rate of 12 breaths/min at a 0.5 fraction of inspired oxygen, a 1:2 inspiratory-to-expiratory ratio, and a 1.5 L/min flow rate for oxygen and nitrous oxide without positive end-expiratory pressure. Immediately before surgical incision, the tidal volume was reduced to 5 mL/kg and the respiratory rate was increased to 15 breaths/min (Figure 1). CO2 retention and intrinsic positive end-expiratory pressure were monitored using end-tidal CO2 and a manometer with a ventilator (S/5 Avance with monitor; Datex-Ohmeda, Madison, WI). To minimize the potential for hypoxia and a barotrauma event, the anesthesiologist adjusted the ventilator setting when pulse oximetry was lower than 90% or the peak inspiratory pressure was higher than 25 mmHg. We recorded the time from intubation to surgical incision, operation time, and total anesthesia time.
Operation
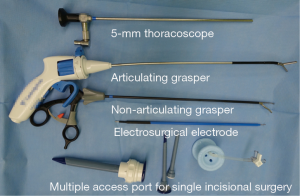
Patients were placed in the lateral decubitus position. A 2.5-cm surgical incision was made at the 6th or 7th intercostal space using the hole through which the chest tube was inserted. We installed the SILS port at this incision, and 6 mmHg of CO2 gas was continuously insufflated into the thoracic cavity via the SILS port channel to achieve a better operative field under TLVA (Figure 2). Initially, a 5-mm thoracoscope connected to a light cable at right angles to prevent instrumental conflicts was introduced to identify pleural adhesions and bullae or blebs. After inspecting the location and extent of bullae or blebs, we used one or two flexible endoscopic staplers to resect the apical lung lesion along with an articulating Endo Grasper. Finally, the CO2 gas insufflation was stopped and the SILS port was removed; a resected lung specimen was retrieved through the incision. The stapler line was reinforced with surgical mesh and fibrin glue. To facilitate pleural symphysis, we performed mechanical pleurodesis using medical sandpaper and chemical pleurodesis using powdered minocycline (Figure 3). In all patients, a 24-french chest drain was inserted into the lung apex.
Postoperative course
We routinely applied 15 to 20 cmH2O of thoracic suction and checked the daily chest PA or AP images. In case of a positive air leak with an unexpanded lung, we performed additional bedside chemical pleurodesis with powdered minocycline. The chest drain was removed if the drain amount was reduced to less than twice the weight (kg*mL) after a daily 5 cm step-by-step pullback of the chest drain. The day following chest drain removal, patients were discharged if their chest PA image showed no pneumothorax. All patients were followed up at 1 week, 1 month, and 3 months postoperatively.
Results
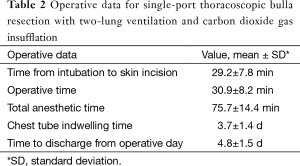
The study included 121 men and nine women aged 22.6±8.3 years (range, 13–56 years). The indication for surgery was a recurrent pneumothorax in 130 patients who showed bullae or blebs on chest computed tomography. There were 18 bilateral surgeries. All patients successfully underwent SITS under TLVA with CO2 gas insufflation through a SILS port. No conversions to a conventional three-port VATS or CO2-related intraoperative adverse events occurred. The time from endotracheal intubation to incision was 29.2±7.8 minutes (range, 15–55 minutes) and the operation time was 30.9±8.2 minutes (range, 11–57 minutes). The total time under anesthesia was 75.7±14.4 minutes (range, 30–126 minutes). Chest drains were removed 3.7±1.4 days (range, 2–11 days) from the day of operation. Fifteen patients showed prolonged air leaks (longer than 5 days) postoperatively and were treated with additional bedside pleurodesis with minocycline. Eventually, chest drains were removed successfully in these patients without complications. Patients were discharged after a mean of 4.8±1.5 days (range, 3–15 days) (Table 2). During 7.5±10.1 months (range, 4.3–43.9 months) of follow-up, no wound or TLVA-related problems occurred. There were five ipsilateral (3.8%) and nine contralateral (6.9%) recurrences. Ipsilateral recurrences were treated conservatively by reinserting a chest drain in three patients and with oxygen inhalation in two patients.
Full table
Comments
In this study, we infused CO2 gas into the thoracic cavity to collapse the lung during TLVA based on a similar method used in needlescopic sympathetic surgery for hyperhidrosis (26). To our knowledge, there have been no reports of SITS under TLVA with CO2 gas insufflation for pneumothorax.
The standard VATS procedure utilizes three or four ports that are 1 or 2 cm in size (utility incision, thoracoscope, one or two ports per instrument). However, the feasibility of performing VATS using two ports or a single port has been described in many thoracic diseases along with the benefits of better cosmetic results and tolerable postoperative pain. A 2- to 5-mm thoracoscope is preferred over the 10-mm thoracoscope as it reduces the torque on the intercostal nerves even through a small incision. There have been many modifications of the SITS technique, including SITS performed using a 2-mm needlescope (23) or a 5- to 10-mm thoracoscope with or without any trocar or scope guide to maximize instrumental maneuverability (27). Various incisional lengths measuring between 2 and 4 cm can be created during the procedure. In addition, a subxiphoid incision was introduced for bilateral lesions (28). Recently, the most minimally invasive VATS, non-intubated surgery using a single port, has been reported in limited numbers (29,30). Avoiding airway trauma and general anesthesia can be more advantageous than our strategy, although uncontrollable lung movement and spontaneous breathing can lead to a difficult surgical procedure and fatal events.
Some clinicians have reported the feasibility and safety of SITS performed using a SILS port (13,31). The SILS port was originally designed for single-port laparoscopic surgery; its application to VATS has enabled a more accurate lining up of instruments and improved reticulating endoscopic device ergonomics and performance through port channels. Moreover, the three-way stopcock in the SILS port was originally designed for pneumoperitoneum induction during laparoscopic surgery. Carbon dioxide gas insufflation has been used to create a pneumoperitoneum in laparoscopic surgery (32) and has also been used in sympathetic or mediastinal surgery (33). In pediatric thoracic surgery (34), where double lumen tubes are not available, a low flow and pressure (<8 cmH2O) infusion of CO2 into the thoracic cavity helps partially compress the lung and increases the visualization of intrathoracic structures, as in our series. In thoracic surgery, the optimal endoscopic surgical view can usually be achieved by insufflating carbon dioxide during the procedure. However, there have been few reports of lung resection under two-lung anesthesia with the exception of drainage for pleural effusion or biopsy for a pleural lesion (35). Our consecutive 130 cases of single-port VATS for primary spontaneous pneumothorax utilized a SILS port under TLVA with low tidal volume and CO2 gas infusion into the thoracic cavity. OLVA may be indicated in most thoracoscopic surgeries for better visualization of the surgical field after proper collapse of the lung (17). However, OLVA requires a double endotracheal tube or a Univent with a blocker, which is costly compared with a single lumen endotracheal tube (23). It also requires additional time for confirming the proper positioning of the endotracheal tube by intraoperative bronchoscopy. Anesthesiologists may also have concerns regarding unexpected complications related to double lumen tube intubation such as hypoxia that can result from improper tube positioning whereas the VATS procedure for pneumothorax is short and simple. Some clinicians have reported that low tidal volume with high frequency can be a feasible option in simple thoracoscopic procedures (35). Despite the availability of TLVA for simple thoracoscopic procedures, pneumothorax requires VATS to ensure an adequate surgical field for the stapling of bullae or blebs or the inspection of additional fissural blebs. This technique was well-tolerated in most patients in our series (22). However, some other series reported potential complications including CO2 embolism and hypotension resulting from impaired venous returns (36). Stopping the gas infusion and relieving the pneumothorax can promptly reverse hypercarbia and hypoxia.
Initially, we did not use CO2 gas during multiport VATS for pneumothorax under TLVA because it is possible to identify the apical bullous lesion with low tidal volume without CO2. However, in single-port VATS, the apical bullous lesions can be missed due to the limited thoracoscopic view when using a previous improper chest drain site under TLVA. CO2 insufflation may not be a mandatory component of this procedure for experienced surgeons, but represents a useful technique for beginners performing SITS with a SILS port for pneumothorax. Nevertheless, our two-lung anesthetic strategy for SITS using a SILS port has several potential advantages such as reduced postoperative pain compared with single-port surgery using a uniportal trocar and reduced anesthetic and operative times compared with one-lung ventilation. The limitation of this study is that a disposable SILS port is mandatory to our surgical strategy, increasing surgical cost. However, the benefits of our surgical strategy may outweigh the high instrument cost inherent in most minimally invasive surgeries.
We routinely performed mechanical and chemical pleurodesis in all our cases. Although there was no early (<30 days) recurrence of ipsilateral thorax and no need to reoperate, additional pleurodesis during surgery for pneumothorax for the prevention of recurrence remains controversial (37,38) and may be considered in select recurrent cases. In our series, TLVA strategy had a little impact on the postoperative outcomes compared to historical papers (13). Our relatively longer chest drain indwelling time (3.7±1.4 days) may have been caused by the strict criteria for chest drain removal (less than twice the body weight) in our center. In addition, the relatively longer hospital stay (4.8±1.5 days) noted in our series is due to patients’ reluctance to leave the hospital early as a result of the comprehensive national insurance coverage in our country.
In conclusion, our anesthetic strategy using two-lung ventilation with low tidal volume and CO2 infusion through a SILS port was a technically feasible and safe procedure for simple thoracoscopic bulla resection. Using a SILS port provides the additional benefits of improved instrumental maneuverability and procedural performance in single-port thoracoscopic surgery during two-lung ventilation. This procedure can represent a safe alternative to VATS for the treatment of primary spontaneous pneumothorax with the advantages of reduced anesthetic and operative times.
Acknowledgements
Funding: This work was supported by a grant from the National Research Foundation of Korea (NRF) grant funded by the Ministry of Education, Science and Technology (NRF-2015R1A2A2A04005760) and “the Technology Innovation Program” (N0001689) funded By the Ministry of Trade, industry & Energy (MI, Korea).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Noppen M. Spontaneous pneumothorax: epidemiology, pathophysiology and cause. Eur Respir Rev 2010;19:217-9. [Crossref] [PubMed]
- Noppen M, De Keukeleire T. Pneumothorax. Respiration 2008;76:121-7. [Crossref] [PubMed]
- Tschopp JM, Rami-Porta R, Noppen M, et al. Management of spontaneous pneumothorax: state of the art. Eur Respir J 2006;28:637-50. [Crossref] [PubMed]
- Ng CS, Rocco G, Yim AP. Video-assisted thoracoscopic surgery (VATS) pleurodesis for pneumothorax. Multimed Man Cardiothorac Surg 2005;2005(425):mmcts.2004.000349.
- Joshi V, Kirmani B, Zacharias J. Thoracotomy versus VATS: is there an optimal approach to treating pneumothorax? Ann R Coll Surg Engl 2013;95:61-4. [Crossref] [PubMed]
- Salati M, Brunelli A, Xiumè F, et al. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg 2008;7:63-6. [Crossref] [PubMed]
- Berlanga LA, Gigirey O. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax using a single-incision laparoscopic surgery port: a feasible and safe procedure. Surg Endosc 2011;25:2044-7. [Crossref] [PubMed]
- Rocco G, La Rocca A, La Manna C, et al. Uniportal video-assisted thoracoscopic surgery pericardial window. J Thorac Cardiovasc Surg 2006;131:921-2. [Crossref] [PubMed]
- Tam JK, Lim KS. Total muscle-sparing uniportal video-assisted thoracoscopic surgery lobectomy. Ann Thorac Surg 2013;96:1982-6. [Crossref] [PubMed]
- Kim HK, Choi YH. The feasibility of single-incision video-assisted thoracoscopic major pulmonary resection performed by surgeons experienced with a two-incision technique. Interact Cardiovasc Thorac Surg 2015;20:310-5. [Crossref] [PubMed]
- Ng CS, Kim HK, Wong RH, et al. Single-Port Video-Assisted Thoracoscopic Major Lung Resections: Experience with 150 Consecutive Cases. Thorac Cardiovasc Surg 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Liu CY, Lin CS, Shih CH, et al. Single-port video-assisted thoracoscopic surgery for lung cancer. J Thorac Dis 2014;6:14-21. [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [Crossref] [PubMed]
- Tang B, Hou S, Cuschieri SA. Ergonomics of and technologies for single-port lapaxroscopic surgery. Minim Invasive Ther Allied Technol 2012;21:46-54. [Crossref] [PubMed]
- Mirzabeigi E, Johnson C, Ternian A. One-lung anesthesia update. Semin Cardiothorac Vasc Anesth 2005;9:213-26. [Crossref] [PubMed]
- Cohen E. Physiology of the lateral position and one-lung ventilation. Chest Surg Clin N Am 1997;7:753-71. [PubMed]
- Dunn PF. Physiology of the lateral decubitus position and one-lung ventilation. Int Anesthesiol Clin 2000;38:25-53. [Crossref] [PubMed]
- Varma S, Beardow Z, Elliot SC, et al. Intraoperative bronchoscopy prevents hypoxaemia during one-lung ventilation for second-stage oesophagectomy: a prospective cohort study. Eur J Anaesthesiol 2010;27:919-21. [Crossref] [PubMed]
- Gothard J. Lung injury after thoracic surgery and one-lung ventilation. Curr Opin Anaesthesiol 2006;19:5-10. [Crossref] [PubMed]
- Kim H, Kim HK, Choi YH, et al. Thoracoscopic bleb resection using two-lung ventilation anesthesia with low tidal volume for primary spontaneous pneumothorax. Ann Thorac Surg 2009;87:880-5. [Crossref] [PubMed]
- Kim H, Kim HK, Kang DY, et al. A comparative study of two- versus one-lung ventilation for needlescopic bleb resection. Eur Respir J 2011;37:1183-8. [Crossref] [PubMed]
- Lee DK, Kim HK, Lee K, et al. Optimal Respiratory Rate for Low-Tidal Volume and Two-Lung Ventilation in Thoracoscopic Bleb Resection. J Cardiothorac Vasc Anesth 2015;29:972-6. [Crossref] [PubMed]
- Han KN, Kim HK, Lee HJ, et al. Single-port thoracoscopic surgery for pneumothorax under two-lung ventilation with carbon dioxide insufflation. Asvide 2016;3:226. Available online: http://www.asvide.com/articles/985
- El-Dawlatly A, Al-Dohayan A, Riyad W, et al. Thoracoscopic sympathectomy: endobronchial anesthesia vs endotracheal anesthesia with intrathoracic CO2 insufflation. J Anesth 2002;16:13-6. [Crossref] [PubMed]
- Rocco G. One-port (uniportal) video-assisted thoracic surgical resections--a clear advance. J Thorac Cardiovasc Surg 2012;144:S27-31. [Crossref] [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. [Crossref] [PubMed]
- Rocco G, Romano V, Accardo R, et al. Awake single-access (uniportal) video-assisted thoracoscopic surgery for peripheral pulmonary nodules in a complete ambulatory setting. Ann Thorac Surg 2010;89:1625-7. [Crossref] [PubMed]
- Galvez C, Bolufer S, Navarro-Martinez J, et al. Awake uniportal video-assisted thoracoscopic metastasectomy after a nasopharyngeal carcinoma. J Thorac Cardiovasc Surg 2014;147:e24-6. [Crossref] [PubMed]
- Gigirey Castro O, Berlanga González L, Sánchez Gómez E. Single port thorascopic surgery using the SILS tool as a novel method in the surgical treatment of pneumothorax. Arch Bronconeumol 2010;46:439-41. [Crossref] [PubMed]
- Woolcott R. The safety of laparoscopy performed by direct trocar insertion and carbon dioxide insufflation under vision. Aust N Z J Obstet Gynaecol 1997;37:216-9. [Crossref] [PubMed]
- Shachor D, Jedeikin R, Olsfanger D, et al. Endoscopic transthoracic sympathectomy in the treatment of primary hyperhidrosis. A review of 290 sympathectomies. Arch Surg 1994;129:241-4. [Crossref] [PubMed]
- Rothenberg SS. Thoracoscopic pulmonary surgery. Semin Pediatr Surg 2007;16:231-7. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Sheils TM, et al. Video-assisted thoracoscopic surgery using single-lumen endotracheal tube anesthesia. Chest 2004;126:281-5. [Crossref] [PubMed]
- Falt P, Liberda M, Smajstrla V, et al. Combination of water immersion and carbon dioxide insufflation for minimal sedation colonoscopy: a prospective, randomized, single-center trial. Eur J Gastroenterol Hepatol 2012;24:971-7. [Crossref] [PubMed]
- Park JS, Han WS, Kim HK, et al. Pleural abrasion for mechanical pleurodesis in surgery for primary spontaneous pneumothorax: is it effective? Surg Laparosc Endosc Percutan Tech 2012;22:62-4. [Crossref] [PubMed]
- Min X, Huang Y, Yang Y, et al. Mechanical pleurodesis does not reduce recurrence of spontaneous pneumothorax: a randomized trial. Ann Thorac Surg 2014;98:1790-6; discussion 1796.


