Evaluation of surgeon’s muscle fatigue during thoracoscopic pulmonary lobectomy using interoperative surface electromyography
Introduction
Video-assisted thoracoscopic surgery (VATS) has revolutionized the management of most cases of thoracic surgery, having been proven to have advantages over conventional thoracotomy in terms of reduced postoperative pain, an earlier return to normal function, shorter hospital stay and reduced costs, and decreased postoperative morbidities and mortalities (1). However, VATS has also presented surgeons with ergonomic problems and complaints of physical discomfort. According to previous reports of a survey of 216 thoracic surgeons, the majority of respondents suffered discomfort after performing thoracoscopic surgery, particularly in the neck (81.9%), shoulder (76.3%) and back (83.2%) (2). Some researchers express this phenomenon as “patients benefit while surgeons suffer” (3).
Ergonomics is defined as the study of the relationship between humans and their working environment, with the aim in this case of providing a safe working environment for the workers and, at the same time, maintaining the effectiveness and improving the efficiency of the medical devices used (2). Among the several methodologies in ergonomic science, electromyography (EMG) is a technique used to evaluate and record the electrical activity produced by skeletal muscles. EMG is able to measure the activity and fatigue of a specific muscle, and has therefore been applied to the diagnosis of various work-related muscular diseases in ergonomics (4). Some studies have applied EMG to surgeons and the surgical environment (5,6). However, they measured the surgeon’s EMG in an experimental setting (dry-lab) (5,6). No previous studies, as far as we are aware, have measured EMG during surgery itself.
We hypothesized that the intraoperative measurement of EMG could reflect the real surgical environment during VATS, and therefore it could be helpful for the detection of specific muscles related to discomfort during VATS lobectomy. This study was undertaken to measure the muscle activity and fatigue, and to identify the specific muscles related to discomfort, during VATS lobectomy using intraoperative EMG.
Methods
Surgeon
The intraoperative surface EMG was measured during 12 cases of VATS lobectomy and mediastinal lymph node dissection for lung cancer. All operations were performed by a single surgeon (the corresponding author) who had no previous history of musculoskeletal disease, especially cervical and lumbar disease. In addition, he had sufficient experience, having performed more than 300 cases of VATS lobectomy for lung cancer during the five years prior to this experiment. Each operation was scheduled as the first case of the day, to exclude the possibility of accumulated muscle fatigue. All 12 lobectomy cases were performed with the same thoracoscopic instruments, and the ports and working window were created in the same intercostal space, under the surgeon’s routine practice. Because we focused on the information about the operation itself such as operation time, the identifying information of patients were not collected. The institutional review board (AJIRB-MED-EXP-16-045) allowed the exemption from the individual consent, according to the institutional guidelines for waiving consent.
Electromyography
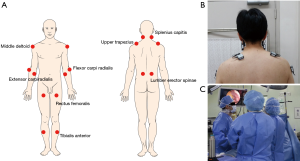
The 16 channels of a wireless EMG system (TeleMyo 2400T DTS, Noraxon USA Inc., Scottsdale, AZ, USA) were used to collect surface EMG signals. The 16 circular Ag/AgCl bipolar electrodes were attached with double-sided tape to the bilateral splenius capitis (SC), upper trapezius (UT), middle deltoid (MD), flexor carpi radialis (FCR), extensor carpi radialis (ECR), lumbar erector spinae (LES), rectus femoralis (RF), and tibialis anterior (TA) before the operation to measure the stress on the surgeon’s muscles (Figure 1A,B). These muscles were selected from the entire body to find the specific area (muscle) susceptible to discomfort. The diameter of each electrode was 10 mm and the center-to-center inter-electrode distance was 20 mm. The signals were amplified using a single differential amplifier with an input impedance of 1,000 MΩ, a common mode rejection ratio of 110 dB, and a gain of 1,000. The signals were filtered with a bandwidth of 20–450 Hz and sampled at 1,024 Hz. All surface electrodes were attached according to landmarks by an experienced physiatrist who majored in musculoskeletal rehabilitation (first author), based on the recommendations published by SENIAM (Surface EMG for Non-Invasive Assessment of Muscles) (7). Before the electrodes were attached, the attachment sites were shaved and then cleaned with an alcohol swab. All signals from the 16 channels were zeroed before the operation, while the surgeon was in a fully-relaxed state. EMG parameters were measured for 1 minute at 5-minute intervals during the operation (Figure 1C). The normalization technique which required the surgeon to exert maximum force of every muscle usually three times in order to estimate the percentage of maximal voluntary contraction (%MVC) was not utilized for this study because it could cause the fatigue of the surgeon before the operation.
The EMG signals were analyzed with MyoResearch XP (ver. 1.07.25; Noraxon USA Inc.). The root mean square (RMS) and median frequency (MF) were analyzed for every signal measurement. RMS usually indicates the activity of muscles, and a high RMS corresponds to high muscle activity. MF usually indicates the level of muscle fatigue, therefore a decreased MF from the initial status indicates increased muscle fatigue during the operation.
Statistical analysis
Statistical analysis was performed using the SPSS for Windows software (ver. 13.0; SPSS Inc., Chicago, IL, USA). Variances were calculated to investigate the variability of each parameter. To evaluate the decrements of MF, a paired t-test was performed to compare the initial MF of the first measurement with the final MF of the last measurement. The time trends of MF were also analyzed with linear mixed models with random slope and intercept.
Results
General characteristics of the 12 patients
All operations were completed without the occurrence of any intraoperative events, and none of the patients experienced any postoperative complications or operative mortality during their recovery. The clinical characteristics of the 12 patients are summarized in Table 1. The mean operation time was 99.16±35.15 minutes.

Full table
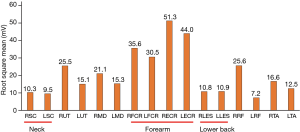
Root-mean-squares of the 16 muscles
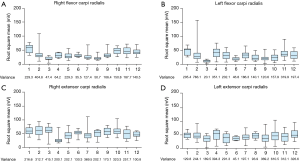
The mean RMS of each muscle during the operations is illustrated in Figure 2. The mean RMS of all 16 muscles was 21.91±12.85 mV. High muscle activity (high RMS) was observed in forearm muscles such as the bilateral FCR and ECR, whereas low muscle activity (low RMS) was observed in neck and spine muscles such as the bilateral SC and LES. The RMS of the bilateral SC, LES, FCR, and ECR in each operation is shown in Figures 3 and 4. In general, the variance of FCR and ECR was higher than the variance of SC and LES, indicating that the variability of muscle activity in FCR and ECR was higher than in SC and LES, and that SC and LES showed more static activity than FCR and ECR.
Median frequencies of the 16 muscles
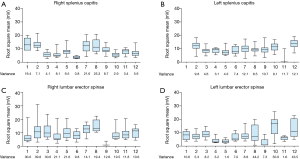
The final MFs (observed at the operation end time) were found to have decreased from the initial status in the bilateral SC and LES located in the cervical and lumbar spine (Figure 5), indicating increased muscle fatigue. The muscles of the right and left LES were significantly fatigued by up to 29% and 37% compared to the initial status (P=0.021 and P=0.007, respectively). On the other hand, the final MFs of the bilateral MD, FCR, ECR, RF, and TA were increased compared to the initial status.
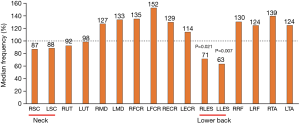
The changes in MFs were compared according to the operation time. The final MFs of all the muscles in operations taking less than 100 minutes (the mean operation time) and greater than 100 minutes were (103.3±10.9)% and (42.9±30.9)%, respectively (P=0.004). This shows that increased operation time is related to muscle fatigue.
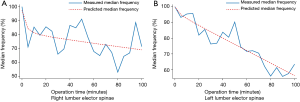
Time trends of the median frequencies of the bilateral lumbar erector spinae
The time trends of the MF measured every five minutes during the operations showed the most prominent decrease in MF in bilateral LES (Figure 6). The MF showed an average decreases of 0.008/5 minutes [95% confidence interval (CI): −0.013 to −0.003, P=0.002] in right LES and 0.004/5 minutes (95% CI: −0.021 to −0.002, P=0.018) in left LES.
Discussion
We found that muscle fatigue occurred in muscles with low activity and a low variability of muscle activity, and was related to a static posture in the neck and lower back during VATS lobectomy. In particular, there was prominent fatigue of the bilateral LES, and this increased gradually over time.
This study provides an advantage over previous studies, in terms of the intraoperative measurement of EMG. Previous studies have measured EMG in an experimental setting which reproduces the environment of the operating room (5,6). Even though such experimental settings can allow for measurement of the factors of interest while controlling other related risk factors, these experiments were not able to reflect the real surgical setting. In addition, in an experimental setting the measurement of EMG during the performance of a specific task within a limited time, such as endoscopic suturing or the transfer of objects (8), cannot reflect the time factors present during an actual operation, particularly since an operation can take a long time to complete. This study measured intraoperative surface EMG; therefore, it reflects the real surgical environment and long operation time. Our results are well correlated with previous reports of a survey of 216 thoracic surgeons that showed that the majority of respondents suffered from a variety of discomfort sensations, particularly in the neck (81.9%), shoulder (76.3%) and lower back (83.2%) after performing thoracoscopic surgery (2). The muscles located in the area where most thoracic surgeons described discomfort, such as the neck and lower back, showed a decreased MF compared to the initial status. Therefore, muscle fatigue might be related to muscle discomfort.
This study provided some interesting results. First, several muscles with high activity (high RMS) showed an increased final MF (greater than 100%) compared to the initial status. According to the Cinderella hypothesis (9), muscles initially use slow twitch fibers for low activity and then fast twitch fibers for high activity. Slow twitch fibers generally have the characteristics of low frequency and low activity, while fast twitch fibers have those of high frequency and high activity. Unlike the neck and lower back muscles that only required slow twitch fiber (low activity) during the operation, some muscles such as the bilateral FCR and ECR muscles often required fast twitch fibers as well because the surgeon was often highly active with his hands and wrists during the operation. Therefore, these muscles showed a high mean RMS and increased final MF and, thus, large variations as seen in Figure 3 (10). In contrast, low muscle activity was observed in the neck and lower back muscles, and these muscles showed a decreased MF. These findings correlate well with previous studies, which showed that the constant, low-activity activation of a motor unit is related to chronic muscle pain (4,10), because a specific motor unit that continuously shows low-level activity may become metabolically overloaded with mitochondrial disturbance (4,9). Additionally, a static back posture has been implicated in increasing back pain in surgeons (11). Nguyen reviewed the intraoperative video tape and reported that static neck and trunk postures were frequently observed during laparoscopic surgery (12). Second, muscle fatigue was prominent in cases with a longer operation time (greater than 100 minutes), and the graphs (Figure 6) show that the MF of the bilateral LES gradually decreased over time. Our data showed that a prolonged operation time could be a risk factor for ergonomic problems, in addition to previously-suggested risk factors such as awkward body posture and frequent uncomfortable repetitive movements (11).
Based on the findings of this study and the results from previous studies, we can suggest some ergonomic improvements. Berguer et al. reported that laparoscopic surgeons often maintained a head-straight, back-straight stance (13), and Nguyen also reported that surgeons performing laparoscopic surgery have significantly less back flexion than surgeons who perform the open surgery (12). In addition, reduced body movement and weight-shifting were observed in laparoscopic surgery compared with open surgery (13). These factors could be the cause of muscle fatigue during VATS lobectomy. During the operation, intentional posture change and relaxation, and efforts to maintain natural spine alignment, could be helpful for reducing fatigue around the neck and lower back muscles. In addition, since the MF gradually decreased with increasing time, shortening of the overall operation time would help to reduce muscle fatigue during VATS surgery.
This study had several limitations. First, we measured surface EMG in a single surgeon. Therefore, our results might be influenced by the individual habits and operation method preferences of the surgeon. While generalizing the results of this study should be done cautiously, we consider that using this individualized approach to determine the ergonomic problems of each surgeon is useful and valid for tailored diagnosis and prescription. Second, we could not attach the surface electrodes to the hands in the intraoperative setting. Even though finger numbness and fatigue of the wrist and hand are among the frequent discomfort complaints during VATS surgery (2,12), attaching the surface electrodes to the hands during an operation is practically impossible because it can violate the sterile intraoperative conditions and interfere with the hand movements of the surgeon. According to a previous report, the factor contributing most towards wrist and hand fatigue is awkward wrist movements (12). Therefore, video analysis of the surgeon to detect awkward wrist movements might be more useful, instead of obtaining EMG data (e.g., the RMS and MF of the hand muscles). In spite of these limitations, this study is important because it is the first to attempt intraoperative measurement of EMG.
In conclusion, muscle fatigue was observed in muscles with low-activity and low variability of muscle activity, and was related to a static neck and waist posture during VATS lobectomy. Bilateral LES fatigue was particularly prominent, and increased gradually over time. More data from a greater number of surgeons are needed to validate these results and correlate the surface EMG data with the surgeon’s subjective symptoms. The results from intraoperative surface EMG can be applied to consider ergonomic strategies, and to reduce muscle fatigue during VATS surgery.
Acknowledgements
This work was supported by the new faculty research fund of Ajou University School of Medicine.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Yim AP. VATS major pulmonary resection revisited--controversies, techniques, and results. Ann Thorac Surg 2002;74:615-23. [Crossref] [PubMed]
- Welcker K, Kesieme EB, Internullo E, et al. Ergonomics in thoracoscopic surgery: results of a survey among thoracic surgeons. Interact Cardiovasc Thorac Surg 2012;15:197-200. [Crossref] [PubMed]
- Park A, Lee G, Seagull FJ, et al. Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg 2010;210:306-13. [Crossref] [PubMed]
- Zennaro D, Läubli T, Krebs D, et al. Continuous, intermitted and sporadic motor unit activity in the trapezius muscle during prolonged computer work. J Electromyogr Kinesiol 2003;13:113-24. [Crossref] [PubMed]
- Berquer R, Smith WD, Davis S. An ergonomic study of the optimum operating table height for laparoscopic surgery. Surg Endosc 2002;16:416-21. [Crossref] [PubMed]
- Berguer R, Gerber S, Kilpatrick G, et al. An ergonomic comparison of in-line vs pistol-grip handle configuration in a laparoscopic grasper. Surg Endosc 1998;12:805-8. [Crossref] [PubMed]
- Hermens HJ, Freriks B, Merletti R, et al. European recommendations for surface electromyography. Roessingh Research and Development 1999;8:13-54.
- Lee GI, Lee MR, Clanton T, et al. Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc 2014;28:456-65. [Crossref] [PubMed]
- Hägg GM. Human muscle fibre abnormalities related to occupational load. Eur J Appl Physiol 2000;83:159-65. [Crossref] [PubMed]
- Thorn S. Motor unit firing patterns in light manual work. Licentiatavhandling Institutionen för Produkt-och produktionsutveckling/Människa-tekniksystem (HFE), Chalmers Tekniska Högskola 2002.
- Berguer R. Surgery and ergonomics. Arch Surg 1999;134:1011-6. [Crossref] [PubMed]
- Nguyen NT, Ho HS, Smith WD, et al. An ergonomic evaluation of surgeons' axial skeletal and upper extremity movements during laparoscopic and open surgery. Am J Surg 2001;182:720-4. [Crossref] [PubMed]
- Berguer R, Rab GT, Abu-Ghaida H, et al. A comparison of surgeons' posture during laparoscopic and open surgical procedures. Surg Endosc 1997;11:139-42. [Crossref] [PubMed]


